Abstract
Introduction Guidelines on the length of treatment of dental infections with systemic antibiotics vary across different countries. We aimed to determine if short-duration (3-5 days) courses of systemic antibiotics were as effective as longer-duration courses (≥7 days) for the treatment of dental infections in adults in outpatient settings.
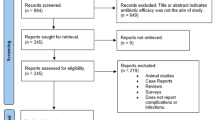
Methods We searched Ovid Medline, Ovid Embase, Cochrane, trials registries, Google Scholar and forward and backward citations for studies published between database inception and 30 March 2021. All randomised clinical trials (RCT) and non-randomised trials which compared length of treatment with systemic antibiotics for dental infections in adults in outpatient settings published in English were included.
Results One small RCT met our defined inclusion criteria. The trial compared three-day versus seven-day courses of amoxicillin in adults with odontogenic infection requiring tooth extraction. There was no significant difference between groups in terms of participant-reported pain or clinical assessment of wound healing.
Discussion While a number of observational studies were supportive of shorter-course therapy, only one small RCT concluded that a three-day course of amoxicillin was clinically non-inferior versus seven days for the treatment of odontogenic infection requiring tooth extraction. Limited conclusions on shorter-course therapy can be drawn from this study as all participants commenced amoxicillin two days before tooth extraction which is not common clinical practice. The variability in guidelines for use of antimicrobials in dental infections suggests that guidelines are based on local or national historical practice and indicates the need for further research to determine the optimum length of treatment. RCTs are required to investigate if short-duration courses of antibiotics are effective and to provide evidence to support consistent guidance for dental professionals.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Matthews D C, Sutherland S, Basrani B. Emergency management of acute apical abscesses in the permanent dentition: a systematic review of the literature. J Can Dent Assoc 2003; 69: 660.
Scottish Dental Clinical Effectiveness Programme. Drug prescribing for dentistry: Dental clinical guidance. 3rd ed. Dundee: SDCEP, 2016.
Aminoshariae A, Kulild J C. Evidence-based recommendations for antibiotic usage to treat endodontic infections and pain: A systematic review of randomized controlled trials. J Am Dent Assoc 2016; 147: 186-191.
National Services Scotland. Scottish One Health Antimicrobial Use and Antimicrobial Resistance in 2019: Annual Report. 2020. Available at https://www.nss.nhs.scot/publications/scottish-one-health-antimicrobial-use-and-antimicrobial-resistance-in-2019/ (accessed October 2021).
Angel Fastina M, Geetha R. Knowledge and awareness about antibiotic policy among dentists. Drug Invent Today 2019; 11: 2531-2533.
Jain M R, Ganapathy D, Sivasamy V. A survey on knowledge, attitude, and perception of antibiotic resistance and usage among dental students. Drug Invent Today 2020; 13: 465-469.
Martin-Jimenez M, Martin-Biedma B, Lopez-Lopez J et al. Dental students' knowledge regarding the indications for antibiotics in the management of endodontic infections. Int Endod J 2018; 51: 118-127.
Ramadan A M, Al Rikaby O A, Abu-Hammad O A, Dar-Odeh N S. Knowledge and attitudes towards antibiotic prescribing among dentists in Sudan. Pesqui Bras Odontopediatr Clin Integr 2019; DOI: 10.4034/PBOCI.2019.191.17.
Srinivasan S, Pradeep S. The attitude of dentists towards the prescription of antibiotics during endodontic treatment - a questionnaire based study. Int J Pharm Technol 2016; 8: 15895-15900.
Wehr C, Cruz G, Young S, Fakhouri W D. An insight into acute pericoronitis and the need for an evidence-based standard of care. Dent J (Basel) 2019; DOI: 10.3390/dj7030088.
Lockhart P B, Tampi M P, Abt E et al. Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal-and periapical-related dental pain and intraoral swelling: A report from the American Dental Association. J Am Dent Assoc 2019; DOI: 10.1016/j.adaj.2019.08.020.
Palmer N. Antimicrobial prescribing in dentistry: good practice guidelines. 3rd ed. London: FGDP, 2020.
American Association of Endodontists. AAE Position Statement: AAE Guidance on the Use of Systemic Antibiotics in Endodontics. J Endod 2017; 43: 1409-1413.
National Institute for Health and Care Excellence. Antimicrobial Prescribing Guidelines. Available at https://www.nice.org.uk/guidance/published?ngt=Antimicrobial%20prescribing%20guidelines&ndt=Guidance (accessed October 2021).
Segura-Egea J J, Gould K, Şen B H et al. European Society of Endodontology position statement: the use of antibiotics in endodontics. Int Endod J 2018; 51: 20-25.
Vasudavan S, Grunes B, McGeachie J, Sonis A L. Antibiotic prescribing patterns among dental professionals in Massachusetts. Pediatr Dent 2019; 41: 25-30.
Sturrock A, Landes D, Robson T, Bird L, Ojelabi A, Ling J. An audit of antimicrobial prescribing by dental practitioners in the north east of England and Cumbria. BMC Oral Health 2018; DOI: 10.1186/s12903-018-0682-4.
Silva M, Paulo M, Cardoso M et al. The use of systemic antibiotics in endodontics: A cross-sectional study. Revista Portuguesa Estomatologia Medicina Dentaria Cirurgia Maxilofacial 2017; 58: 205-211.
Maslamani M, Sedeqi F. Antibiotic and analgesic prescription patterns among dentists or management of dental pain and infection during endodontic treatment. Med Princ Pract 2018; 27: 66-72.
Krishnaa K, Ganapathy D, Bennis M A. Status on the use of antibiotics in endodontic infections among dentists. Drug Invent Today 2020; 14: 562-567.
Inchara R, Ganapathy D, Kiran Kumar P. Preference of antibiotics in pediatric dentistry. Drug Invent Today 2019; 11: 1495-1198.
Bjelovucic R, Par M, Rubcic D, Marovic D, Prskalo K, Tarle Z. Antibiotic prescription in emergency dental service in Zagreb, Croatia- a retrospective cohort study. Int Dent J 2019; 69: 273-280.
Baudet A, Kichenbrand C, Pulcini C et al. Antibiotic use and resistance: a nationwide questionnaire survey among French dentists. Eur J Clin Microbiol Infect Dis 2020; 39: 1295-1303.
Al-Zobaidy M A H J. Evaluation of drug prescription pattern among Iraqi dentists in Babylon city. J Global Pharma Tech 2019; 11(2 Supplement): 204-210.
Ahsan S, Hydrie M Z I, Naqvi S M Z H et al. Antibiotic prescription patterns for treating dental infections in children among general and pediatric dentists in teaching institutions of Karachi, Pakistan. PLoS One 2020; DOI: 10.1371/journal.pone.0235671.
Krah-Sinan A, Adou-Assoumou M, Adou J, Dossahoua K T, Faye D, Mansilla E. Antibiotic therapy in endodontics: a survey from dental surgeons in Ivory Coast. Giornale Italiano Endodonzia 2019; 33: 21-26.
Koyuncuoglu C Z, Aydin M, Kirmizi N I et al. Rational use of medicine in dentistry: do dentists prescribe antibiotics in appropriate indications? Eur J Clin Pharmacol 2017; 73: 1027-1032.
Bolfoni M R, Pappen F G, Pereira-Cenci T, Jacinto R C. Antibiotic prescription for endodontic infections: a survey of Brazilian Endodontists. Int Endod J 2018; 51: 148-156.
Asmar G, Cochelard D, Mokhbat J, Lemdani M, Haddadi A, Ayoubz F. Prophylactic and therapeutic antibiotic patterns of Lebanese dentists for the management of dentoalveolar abscesses. J Contemp Dent Pract 2016; 17: 425-433.
Goossens H, Ferech M, Vander Stichele R, Elseviers M, ESAC Project Group. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 2005; 365: 579-587.
Costelloe C, Metcalfe C, Lovering A, Mant D, Hay A D. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ 2010; DOI: 10.1136/bmj.c2096.
Dawson-Hahn E E, Mickan S, Onakpoya I et al. Short-course versus long-course oral antibiotic treatment for infections treated in outpatient settings: a review of systematic reviews. Fam Pract 2017; 34: 511-519.
Vaughn V M, Flanders S A, Snyder A et al. Excess antibiotic treatment duration and adverse events in patients hospitalized with pneumonia. Ann Intern Med 2019; 171: 153-163.
Bye M, Whitten T, Holzbauer S. Antibiotic prescribing for dental procedures in community-associated Clostridium difficile cases, Minnesota, 2009-2015. Open Forum Infect Dis 2017; DOI: 10.1093/ofid/ofx162.001.
Spellberg B. The new antibiotic mantra - 'shorter is better'. JAMA Intern Med 2016; 176: 1254-1255.
Teoh L, Cheung M C, Dashper S, James R, McCullough M J. Oral antibiotic for empirical management of acute dentoalveolar infections - a systematic review. Antibiotics (Basel) 2021; DOI: 10.3390/antibiotics10030240.
Page M J, McKenzie J E, Bossuyt P M et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; DOI: 10.1136/bmj.n71.
Chardin H, Yasukawa K, Nouacer N et al. Reduced susceptibility to amoxicillin of oral streptococci following amoxicillin exposure. J Med Microbiol 2009; 58: 1092-1097.
Tancawan A L, Pato M N, Abidin K Z et al. Amoxicillin/clavulanic acid for the treatment of odontogenic infections: a randomised study comparing efficacy and tolerability versus clindamycin. Int J Dent 2015; DOI: 10.1155/2015/472470.
Adriaenssen C F. Comparison of the efficacy, safety and tolerability of azithromycin and co-amoxiclav in the treatment of acute periapical abscesses. J Int Med Res 1998; 26: 257-265.
Martin M V, Longman L P, Hill J B, Hardy P. Acute dentoalveolar infections: an investigation of the duration of antibiotic therapy. Br Dent J 1997; 183: 135-137.
Ellison S J. An outcome audit of three-day antimicrobial prescribing for the acute dentoalveolar abscess. Br Dent J 2011; 211: 591-594.
Woolf S H, Grol R, Hutchinson A, Eccles M, Grimshaw J. Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. BMJ 1999; 318: 527-530.
Saltaji H, Armijo-Olivo S, Cummings G G, Amin M, Flores-Mir C. Randomized clinical trials in dentistry: Risks of bias, risks of random errors, reporting quality, and methodologic quality over the years 1955-2013. PLoS One 2017; DOI: 10.1371/journal.pone.0190089.
van der Wouden P, Shemesh H, van der Heijden G J M G. Research priorities for oral healthcare: agenda setting from the practitioners' perspective. Acta Odontol Scand 2021; 79: 451-457.
National Institute for Health Research. The TOP 10 Priorities for oral and dental health research. 2017. Available at https://oralanddentalhealthpsp.wordpress.com/participate/ (accessed October 2021).
Royer S, DeMerle K M, Dickson R P, Prescott H C. Shorter versus longer courses of antibiotics for infection in hospitalized patients: a systematic review and meta-analysis. J Hosp Med 2018; 13: 336-342.
Dinh A, Ropers J, Duran C et al. Discontinuing β-lactam treatment after 3 days for patients with community-acquired pneumonia in non-critical care wards (PTC): a double-blind, randomised, placebo-controlled, non-inferiority trial. Lancet 2021; 397: 1195-1203.
Spellberg B. Shorter is better. 2021. Available at https://www.bradspellberg.com/shorter-is-better (accessed October 2021).
Funding
The Scottish Antimicrobial Prescribing Group receives funding from the Scottish Government. No specific funding was provided for this work. Registration number: Prospero CRD42021241767.
Author information
Authors and Affiliations
Contributions
L. Cooper, J. Sneddon, R. A. Seaton and A. Smith designed the study. L. Cooper and J. Sneddon drafted the manuscript. L. Cooper and N. Stankiewicz completed the literature search, data collection and quality assessment, analysis and synthesis. J. Sneddon, N Stankiewicz, A. Smith and R. A. Seaton critically reviewed and revised the draft manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
The authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Rights and permissions
About this article
Cite this article
Cooper, L., Stankiewicz, N., Sneddon, J. et al. Optimum length of treatment with systemic antibiotics in adults with dental infections: a systematic review. Evid Based Dent (2022). https://doi.org/10.1038/s41432-022-0801-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41432-022-0801-6