Abstract
Hereditary cancer syndromes (HCS) predispose individuals to a higher risk of developing multiple cancers. However, current screening strategies have limited ability to screen for all cancer risks. Circulating tumour DNA (ctDNA) detects DNA fragments shed by tumour cells in the bloodstream and can potentially detect cancers early. This study aimed to explore patients’ perspectives on ctDNA’s utility to help inform its clinical adoption and implementation. We conducted a qualitative interpretive description study using semi-structured phone interviews. Participants were purposively sampled adult HCS patients recruited from a Canadian HCS research consortium. Thirty HCS patients were interviewed (n = 19 women, age range 20s-70s, n = 25 were white). Participants were highly concerned about developing cancers, particularly those without reliable screening options for early detection. They “just wanted more” than their current screening strategies. Participants were enthusiastic about ctDNA’s potential to be comprehensive (detect multiple cancers), predictive (detect cancers early) and tailored (lead to personalized clinical management). Participants also acknowledged ctDNA’s potential limitations, including false positives/negatives risks and experiencing additional anxiety. However, they saw ctDNA’s potential benefits outweighing its limitations. In conclusion, participants’ belief in ctDNA’s potential to improve their care overshadowed its limitations, indicating patients’ support for using ctDNA in HCS care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author YB upon request.
References
Garber JE, Offit K. Hereditary cancer predisposition syndromes. J Clin Oncol. 2005;23:276–92. https://doi.org/10.1200/JCO.2005.10.042
Petrucelli N, Daly MB, Pal T BRCA1- and BRCA2-Associated Hereditary Breast and Ovarian Cancer. GeneReviews. Published online 2022:1–37.
Dominguez-Valentin M, Sampson JR, Seppälä TT, Ten Broeke SW, Plazzer JP, Nakken S, et al. Cancer risks by gene, age, and gender in 6350 carriers of pathogenic mismatch repair variants: findings from the Prospective Lynch Syndrome Database. Genet Med. 2020;22:15–25. https://doi.org/10.1038/s41436
Barrow E, Hill J, Gareth D. Cancer risk in Lynch Syndrome. Fam Cancer. 2013;12:229–40. https://doi.org/10.1007/s10689-013-9615-1
Rabeneck L, Paszat LF, Saskin R, Stukel TA. Association between colonoscopy rates and colorectal cancer mortality. Am J Gastroenterol. 2010:1–6. https://doi.org/10.1038/ajg.2010.83
Mandelblatt JS, Cronin KA, Bailey S, Berry DA, De Koning HJ, Draisma G, et al. Effects of mammography screening under different screening schedules: Model Estimates of Potential Benefits and Harms. 2009;151:738–47.
Patel KM, Tsui DWY. The translational potential of circulating tumour DNA in oncology. Clin Biochem. 2015;48:957–61. https://doi.org/10.1016/j.clinbiochem.2015.04.005
Campos-Carrillo A, Weitzel JN, Sahoo P, Rockne R, Mokhnatkin JV, Murtaza M, et al. Circulating tumor DNA as an early cancer detection tool. Pharm Ther. 2020;207:107458. https://doi.org/10.1016/j.pharmthera.2019.107458
Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N, et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6:69–122. https://doi.org/10.1126/scitranslmed.3007094.Detection
Chen KZ, Lou F, Yang F, Zhang JB, Ye H, Chen W, et al. Circulating tumor DNA detection in early-stage non-small cell lung cancer patients by targeted sequencing. Sci Rep. 2016;6:3–10. https://doi.org/10.1038/srep31985
Shickh S, Oldfield LE, Clausen M, Mighton C, Sebastian A, Calvo A, et al. “Game Changer”: Health professionals’ views on the clinical utility of circulating tumor DNA testing in hereditary cancer syndrome management. Oncologist. 2022:1–9. https://doi.org/10.1093/oncolo/oyac039
Paramathas S, Guha T, Pugh TJ, Malkin D, Villani A. Considerations for the use of circulating tumor DNA sequencing as a screening tool in cancer predisposition syndromes. Pediatr Blood Cancer. 2020;67:e28758. https://doi.org/10.1002/pbc.28758
Batis N, Brooks JM, Payne K, Sharma N, Nankivell P, Mehanna H. Lack of predictive tools for conventional and targeted cancer therapy: Barriers to biomarker development and clinical translation. Adv Drug Deliv Rev. 2021;176:113854. https://doi.org/10.1016/j.addr.2021.113854
Vanstone M, Cernat A, Nisker J, Schwartz L. Women’s perspectives on the ethical implications of non-invasive prenatal testing: a qualitative analysis to inform health policy decisions. BMC Med Ethics. 2018;19:1–3. https://doi.org/10.1186/s12910-018-0267-4
Persky S, Kaphingst KA, Condit CM, McBride CM. Assessing hypothetical scenario methodology in genetic susceptibility testing analog studies: A quantitative review. Genet Med. 2007;9:727–38. https://doi.org/10.1097/GIM.0b013e318159a344
Mackley MP, Fletcher B, Parker M, Watkins H, Ormondroyd E. Stakeholder views on secondary findings in whole-genome and whole-exome sequencing: A systematic review of quantitative and qualitative studies. Genet Med. 2017;19:283–93. https://doi.org/10.1038/gim.2016.109
Bombard Y, Miller FA, Hayeems RZ, Barg C, Cressman C, Carroll JC, et al. Public views on participating in newborn screening using genome sequencing. Eur J Hum Genet. 2014;22:1248–54. https://doi.org/10.1038/ejhg.2014.22
Mighton C, Clausen M, Shickh S, Baxter NN, Scheer A, Sebastian A, et al. How do members of the public expect to use variants of uncertain significance in their health care? A population-based survey. Genet Med. 2023;25:100819. https://doi.org/10.1016/j.gim.2023.100819
Thorne S Interpretive Description. Left Coast Press; 2008. https://doi.org/10.4324/9781315426259
Morse JM, Field PA Qualitative Research Methods for Health Professionals. SAGE Publications, 1995.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. https://doi.org/10.1093/intqhc/mzm042
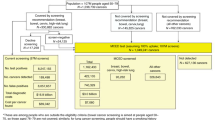
Pugh TJ, Kim R, Pollett A Early detection of cancer in high-risk patients through profiling of circulating tumour DNA. CIHR Funding Decisions Database. Published 2018. Accessed January 17, 2021. https://webapps.cihr-irsc.gc.ca/decisions/p/project_details.html?applId=382384&lang=en
Cresswell J, Poth C Qualitative Inquiry and Research Design: Choosing Among Five Approaches. 4th ed. SAGE, 2018.
Maheu C, Thorne S. Receiving inconclusive genetic test results: An interpretive description of the BRCA1/2 experience. Res Nurs Heal. 2008;31:553–62. https://doi.org/10.1002/nur.20286
Morse JM. Determining sample size what factors should be considered? Qual Health Res. 2000;10:3–5.
Sandelowski M. Focus on qualitative methods qualitative analysis: what it is and how to begin. Res Nurs Health. 1995;18:371–5.
Sebastian A, Carroll JC, Vanstone M, Clausen M, Kodida R, Reble E, et al. Widening the lens of actionability: A qualitative study of primary care providers views and experiences of managing secondary genomic findings. Eur J Hum Genet. 2022;30:595–603. https://doi.org/10.1038/s41431-021-00876-z
Kohler JN, Turbitt E, Lewis KL, Wilfond BS, Jamal L, Peay HL, et al. Defining personal utility in genomics: A Delphi study. Clin Genet. 2017;92:290–7. https://doi.org/10.1111/cge.12998
Bombard Y, Rozmovits L, Trudeau ME, Leighl NB, Deal K, Marshall DA. Patients’ perceptions of gene expression profiling in breast cancer treatment decisions. Curr Oncol. 2014;21:e203–11. https://doi.org/10.3747/co.21.1524
Mateo J, Steuten L, Aftimos P, André F, Davies M, Garralda E, et al. Delivering precision oncology to patients with cancer. Nat Med. 2022;28:658–65. https://doi.org/10.1038/s41591-022-01717-2
Ross J, Bojadzieva J, Peterson S, Noblin SJ, Yzquierdo R, Askins M, et al. The psychosocial effects of the Li-Fraumeni Education and Early Detection (LEAD) program on individuals with Li-Fraumeni syndrome. Genet Med. 2017;19:1064–71. https://doi.org/10.1038/GIM.2017.8
Jhaveri AP, Bale A, Lovick N, Zuckerman K, Deshpande H, Rath K, et al. The benefit and burden of cancer screening in Li-fraumeni syndrome: a case report. Yale J Biol Med. 2015;88:181–5.
Behring M, Hale K, Ozaydin B, Grizzle WE, Manne U. Inclusiveness and ethical considerations for observational, translational, and clinical cancer health disparity research. Cancer. 2019;125:4452–61. https://doi.org/10.1002/cncr.32495
Acknowledgements
We would like to thank our study participants for generously sharing their time and insights for this study. This study was supported by the Canadian Institutes of Health Research.
Funding
This study was supported by a grant from The Canadian Institutes of Health Research (CIHR-159453). EA received support from the Research Training Centre at St. Michael’s Hospital. YB was supported by a New Investigator Award from the Canadian Institutes of Health Research during the conduct of this work. RHK was supported by the Princess Margaret Foundation and the Bhalwani Family Charitable Foundation. As well, this study was performed under the auspice of the LIBERATE study (NCT 03702309), supported by the BMO Chair in Precision Cancer Genomics.
Author information
Authors and Affiliations
Consortia
Contributions
Conceptualization: YB, MC, EA; Formal analysis: YB, EA, MC, SS, JS, ER; Funding acquisition: YB, RHK, TJP, AP; Methodology: YB, EA, MC; Investigation: MC, EA; Resources: YB, LEO, KAS; Writing – original draft: EA, YB; Writing – review and editing: all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted with the approval from Research Ethics Board at Clinical Trials Ontario (REB#1655) in Toronto, Ontario, Canada. All participants interviewed for this study consented to the audio-recording and transcription of their interview. Transcripts were de-identified prior to analysis.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has not been published nor is it under consideration at any other journal or the internet.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Adi-Wauran, E., Clausen, M., Shickh, S. et al. “I just wanted more”: Hereditary cancer syndromes patients’ perspectives on the utility of circulating tumour DNA testing for cancer screening. Eur J Hum Genet 32, 176–181 (2024). https://doi.org/10.1038/s41431-023-01473-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-023-01473-y