Abstract
Background
We aimed to examine the association of the frequency of adding salt to foods and the hazards of the incidence and mortality risks for a range of vascular outcomes, including microvascular, cerebrovascular, and cardiovascular diseases.
Methods
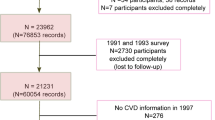
438,307 participants from the UK Biobank who completed the questionnaire on the frequency of adding salt to foods and were free of vascular disease at baseline were enrolled. Information on the frequency of adding salt to foods (do not include salt used in cooking) was collected at baseline through a touch-screen questionnaire. The primary outcomes included incident microvascular diseases, cerebrovascular diseases, and cardiovascular diseases, respectively. The secondary outcomes included: (1) each component of these vascular diseases (10 components in total), (2) first occurrence of fatal and non-fatal vascular diseases.
Results
During a median follow-up of 12.1 years, a total of 17,169 (3.9%), 10,437 (2.4%), and 48,203 (11.0%) participants developed microvascular, cerebrovascular and cardiovascular diseases, respectively. Overall, the hazards of incident microvascular, cerebrovascular and cardiovascular diseases increased with the increasing frequency of adding salt to foods (all P for trend <0.001). Similar trends were found for the secondary outcomes. Moreover, the positive association of always adding salt to foods with hazard of cardiovascular diseases was stronger among current-smokers (P-interaction = 0.010), younger participants (P-interaction <0.001), and those with lower body mass index levels (P-interaction = 0.003).
Conclusions
Higher frequency of adding salt to foods was associated with higher hazards of non-fatal and fatal microvascular, cerebrovascular and cardiovascular diseases, and each component of these vascular diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The UK Biobank data are available on application to the UK Biobank, and the analytic methods, and study materials that support the findings of this study will be available from the corresponding authors on request.
Code availability
The software application or custom code that support the findings of this study will be available from the corresponding authors on request.
References
Aburto NJ, Ziolkovska A, Hooper L, Elliott P, Cappuccio FP, Meerpohl JJ. Effect of lower sodium intake on health: systematic review and meta-analyses. BMJ. 2013;346:f1326.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R, Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
He FJ, MacGregor GA. Role of salt intake in prevention of cardiovascular disease: controversies and challenges. Nat Rev Cardiol. 2018;15:371–7.
O’Donnell M, Mente A, Alderman MH, Brady AJB, Diaz R, Gupta R, et al. Salt and cardiovascular disease: insufficient evidence to recommend low sodium intake. Eur Heart J. 2020;41:3363–73.
Mente A, O’Donnell M, Yusuf S. Sodium intake and health: what should we recommend based on the current evidence? Nutrients. 2021;13:3232.
Liem DG, Miremadi F, Zandstra EH, Keast RS. Health labelling can influence taste perception and use of table salt for reduced-sodium products. Public Health Nutr. 2012;15:2340–7.
De Kock HL, Zandstra EH, Sayed N, Wentzel-Viljoen E. Liking, salt taste perception and use of table salt when consuming reduced-salt chicken stews in light of South Africa’s new salt regulations. Appetite. 2016;96:383–90.
Van der Veen JE, De Graaf C, Van Dis SJ, Van Staveren WA. Determinants of salt use in cooked meals in The Netherlands: attitudes and practices of food preparers. Eur J Clin Nutr. 1999;53:388–94.
Quader ZS, Zhao L, Harnack LJ, Gardner CD, Shikany JM, Steffen LM, et al. Self-reported measures of discretionary salt use accurately estimated sodium intake overall but not in certain subgroups of US adults from 3 geographic regions in the salt sources study. J Nutr. 2019;149:1623–32.
Sutherland J, Edwards P, Shankar B, Dangour AD. Fewer adults add salt at the table after initiation of a national salt campaign in the UK: a repeated cross-sectional analysis. Br J Nutr. 2013;110:552–8.
Webster J, Su’a SA, Ieremia M, Bompoint S, Johnson C, Faeamani G, et al. Salt intakes, knowledge, and behavior in Samoa: monitoring salt-consumption patterns through the World Health Organization’s Surveillance of Noncommunicable Disease Risk Factors (STEPS). J Clin Hypertens (Greenwich). 2016;18:884–91.
Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr. 1991;10:383–93.
Ma H, Xue Q, Wang X, Li X, Franco OH, Li Y, et al. Adding salt to foods and hazard of premature mortality. Eur Heart J. 2022;43:2878–88.
Cohen HW, Hailpern SM, Alderman MH. Sodium intake and mortality follow-up in the Third National Health and Nutrition Examination Survey (NHANES III). J Gen Intern Med. 2008;23:1297–302.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12:e1001779.
Elliott P, Muller DC, Schneider-Luftman D, Pazoki R, Evangelou E, Dehghan A, et al. Estimated 24-hour urinary sodium excretion and incident cardiovascular disease and mortality among 398 628 individuals in UK Biobank. Hypertension. 2020;76:683–91.
Eastwood SV, Mathur R, Atkinson M, Brophy S, Sudlow C, Flaig R, et al. Algorithms for the capture and adjudication of prevalent and incident diabetes in UK Biobank. PLoS One. 2016;11:e0162388.
Malik R, Georgakis MK, Neitzel J, Rannikmäe K, Ewers M, Seshadri S, et al. Midlife vascular risk factors and risk of incident dementia: longitudinal cohort and Mendelian randomization analyses in the UK Biobank. Alzheimers Dement. 2021;17:1422–31.
Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, et al. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373:n604.
Mente A, O’Donnell M, Rangarajan S, Dagenais G, Lear S, McQueen M, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388:465–75.
Welsh CE, Welsh P, Jhund P, Delles C, Celis-Morales C, Lewsey JD, et al. Urinary sodium excretion, blood pressure, and risk of future cardiovascular disease and mortality in subjects without prior cardiovascular disease. Hypertension. 2019;73:1202–9.
Ji C, Sykes L, Paul C, Dary O, Legetic B, Campbell NR, et al. Systematic review of studies comparing 24-hour and spot urine collections for estimating population salt intake. Rev Panam Salud Publica. 2012;32:307–15.
Wang CY, Cogswell ME, Loria CM, Chen TC, Pfeiffer CM, Swanson CA, et al. Urinary excretion of sodium, potassium, and chloride, but not iodine, varies by timing of collection in a 24-hour calibration study. J Nutr. 2013;143:1276–82.
Sun Q, Bertrand KA, Franke AA, Rosner B, Curhan GC, Willett WC. Reproducibility of urinary biomarkers in multiple 24-h urine samples. Am J Clin Nutr. 2017;105:159–68.
Cogswell ME, Maalouf J, Elliott P, Loria CM, Patel S, Bowman BA. Use of urine biomarkers to assess sodium intake: challenges and opportunities. Annu Rev Nutr. 2015;35:349–87.
Weaver CM, Martin BR, McCabe GP, McCabe LD, Woodward M, Anderson CA, et al. Individual variation in urinary sodium excretion among adolescent girls on a fixed intake. J Hypertens. 2016;34:1290–7.
Mills KT, Chen J, Yang W, Appel LJ, Kusek JW, Alper A, et al. Sodium excretion and the risk of cardiovascular disease in patients with chronic kidney disease. JAMA. 2016;315:2200–10.
Olde Engberink RHG, van den Hoek TC, van Noordenne ND, van den Born BH, Peters-Sengers H, Vogt L. Use of a single baseline versus multiyear 24-hour urine collection for estimation of long-term sodium intake and associated cardiovascular and renal risk. Circulation. 2017;136:917–26.
Golledge J, Moxon JV, Jones RE, Hankey GJ, Yeap BB, Flicker L, et al. Reported amount of salt added to food is associated with increased all-cause and cancer-related mortality in older men in a prospective cohort study. J Nutr Health Aging. 2015;19:805–11.
Messner B, Bernhard D. Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol. 2014;34:509–15.
He FJ, Tan M, Ma Y, MacGregor GA. Salt reduction to prevent hypertension and cardiovascular disease: JACC state-of-the-art review. J Am Coll Cardiol. 2020;75:632–47.
Kawarazaki W, Fujita T. Kidney and epigenetic mechanisms of salt-sensitive hypertension. Nat Rev Nephrol. 2021;17:350–63.
Zhou L, Wen X, Peng Y, Zhao L, Yu Y. Salt added to food and body mass index: a bidirectional Mendelian randomisation study. Nutr Diet. 2021;78:315–23.
Acknowledgements
This research has been conducted using the UK Biobank Resource under Application Number 73201. We specially thank all the participants of UK Biobank and all the people involved in building the UK Biobank study.
Funding
The study was supported by the National Natural Science Foundation of China (81973133, 81730019 to XHQ); the National Key Research and Development Programme (2022YFC2009600, 2022YFC2009605 to XHQ); the Outstanding Youths Development Scheme of Nanfang Hospital, Southern Medical University (2017J009 to XHQ); the National Natural Science Foundation of China (Key Programme) (82030022 to FFH); the Programme of Introducing Talents of Discipline to Universities, 111 Plan (D18005 to FFH); Guangdong Provincial Clinical Research Centre for Kidney Disease (2020B1111170013 to FFH); Key Technologies R&D Programme of Guangdong Province (2023B1111030004 to FFH).
Author information
Authors and Affiliations
Contributions
ML, FFH, and XQ designed and conducted the research; ML and ZY performed the data management and statistical analyses; ML and XQ wrote the manuscript. All authors reviewed/edited the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
XQ reports grants from the National Natural Science Foundation of China (81973133, 81730019), the National Key Research and Development Programme (2022YFC2009600, 2022YFC2009605), and the Outstanding Youths Development Scheme of Nanfang Hospital, Southern Medical University (2017J009); FFH reports grants from the National Natural Science Foundation of China (Key Programme) (82030022); the Programme of Introducing Talents of Discipline to Universities, 111 Plan (D18005); Guangdong Provincial Clinical Research Centre for Kidney Disease (2020B1111170013); Key Technologies R&D Programme of Guangdong Province (2023B1111030004); no other disclosures were reported.
Ethics approval and consent to participate
The UK Biobank was approved by the North West Research Ethics Committee (06/MRE08/65) and all participants signed an informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, M., Ye, Z., He, P. et al. Adding salt to foods and hazards of microvascular, cerebrovascular and cardiovascular diseases. Eur J Clin Nutr 78, 141–148 (2024). https://doi.org/10.1038/s41430-023-01354-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01354-z