Abstract
Background
The objective of this study was to evaluate associations of diabetes overall, type 1 diabetes (T1D), and type 2 diabetes (T2D) with breast cancer (BCa) risk.
Methods
We included 250,312 women aged 40–69 years between 2006 and 2010 from the UK Biobank cohort. Adjusted hazard ratios (aHRs) and 95% confidence intervals (CIs) were calculated for associations of diabetes and its two major types with the time from enrollment to incident BCa.
Results
We identified 8182 BCa cases during a median follow-up of 11.1 years. We found no overall association between diabetes and BCa risk (aHR = 1.02, 95% CI = 0.92–1.14). When accounting for diabetes subtype, women with T1D had a higher risk of BCa than women without diabetes (aHR = 1.52, 95% CI = 1.03–2.23). T2D was not associated with BCa risk overall (aHR = 1.00, 95% CI = 0.90–1.12). However, there was a significantly increased risk of BCa in the short time window after T2D diagnosis.
Conclusions
Though we did not find an association between diabetes and BCa risk overall, an increased risk of BCa was observed shortly after T2D diagnosis. In addition, our data suggest that women with T1D may have an increased risk of BCa.
Similar content being viewed by others
Background
Diabetes mellitus is a growing epidemic of global proportions. It is estimated that in 2019, 463 million adults aged 20–79 years were living with diabetes, and the number is likely to grow substantially in future decades [1]. Diabetes occurs through two different primary disease processes. Type 2 diabetes mellitus (T2D) accounts for roughly 90% of diabetes cases worldwide [1]. It is characterized by decreased hepatic and extrahepatic insulin sensitivities and/or impaired insulin release. Type 1 diabetes mellitus (T1D) is characterized by autoimmune destruction of insulin-producing pancreatic ß cells that results in deficient insulin production. Diabetes-associated metabolic disorders, hormonal antecedents, and its treatments could plausibly affect the risk of cancer [2].
Breast cancer (BCa) is the most prevalent cancer in women and the most commonly diagnosed cancer globally, with 2.26 million new cases in 2020 [3]. Diabetes has been proposed to promote BCa initiation through several biological pathways, including alterations of the hyperinsulinemia/insulin-like growth factor (IGF) axis, hyperglycemia, fat-induced inflammation, and changes in sex hormone levels [2, 4,5,6]. Insulin resistance and hyperinsulinemia are less prominent in T1D than T2D [7], but mechanisms underlying a possible association with T1D specifically have not been extensively considered.
Meta-analyses and large cohort studies have suggested an increased risk of BCa in diabetic individuals [8,9,10]. In the largest meta-analysis, which included 40 studies [8], women with diabetes had a significantly increased risk of BCa relative to non-diabetic women (summary relative risk = 1.27, 95% confidence interval (CI): 1.16–1.39). In secondary analyses, only T2D was positively associated with BCa risk; the relationship for T1D was null. In addition, diabetes was only associated with the risk of postmenopausal, and not premenopausal, BCa. Though the meta-analysis was significant overall, so too was the heterogeneity among studies. Differences in epidemiological design could not readily explain the differences, and many studies did not adjust for body mass index (BMI) or other potential confounders. Furthermore, most studies were primarily composed of participants with T2D and/or did not distinguish between the two major types of diabetes. Because of differences in etiology, drug therapies, age at onset, and body composition (wherein individuals with T1D are generally leaner than those with T2D), findings for T2D should not be directly applied to T1D.
The heterogeneity of findings and limited research on T1D support the need for further investigation of the relationship between diabetes and BCa. We thus examined associations of diabetes overall, T1D, and T2D with risk of incident BCa using data from the population-based UK Biobank cohort.
Methods
Study population
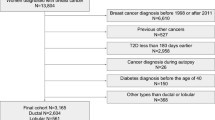
The UK Biobank is a prospective cohort of 502,647 adults aged 40–69 years when they were recruited between 2006 and 2010. The UK Biobank has approval from the North West Multi-centre Research Ethics Committee. At recruitment, all participants provided written informed consent, completed baseline questionnaires and interviews, supplied biospecimens, and underwent physical exams. Since baseline, participants have been followed via linkage to the National Health Service (NHS) Central Register. For these analyses, we excluded participants who: self-reported as male and/or demonstrated male genetic sex (n = 229,255); self-reported cancer but did not have cancer registry records or had neoplasms of uncertain or unknown behavior (n = 1262); had a history of any cancer prior to baseline or a cancer diagnosis without a corresponding diagnosis date (n = 15,348); had a mastectomy (NHS procedure codes: OPCS version 3—383, 384, 385; OPCS version 4—B27) before baseline or mastectomy without corresponding surgery date (n = 6469); or had a recorded death date prior to baseline (n = 1). The remaining 250,312 women comprised our study population.
Exposure
Prevalent and incident diabetes cases were identified using the 10th Revision of the International Classification of Diseases (ICD-10) and/or self-report [11]. ICD-10 codes for insulin-dependent diabetes mellitus (IDDM) and non-insulin-dependent diabetes mellitus (NIDDM) were E10 and E11, respectively. Self-reported diabetes (any diabetes, T1D, or T2D) and the corresponding date that a doctor first diagnosed diabetes were collected during the baseline interview and subsequent assessment center visits based on a standardized questionnaire with good internal validity. Only 8% of diabetes cases, all of which were prevalent, were identified by self-report alone. Based on our meta-analysis of 70 studies investigating the relationship between diabetes and BCa risk [12], the method of diabetes ascertainment does not seem to substantially influence results.
We determined that IDDM and NIDDM do not adequately distinguish T1D and T2D; many participants diagnosed with IDDM had been previously diagnosed with NIDDM or had self-reported T2D that had become insulin dependent. As suggested by previous studies [7, 13], we therefore reclassified participants as having T1D if their earliest age at diabetes diagnosis, whether based on ICD-10 codes or self-reported, was 30 years or younger. All remaining participants were classified as having T2D. Diabetes was considered prevalent if the date of diagnosis was prior to study entry and incident if the diabetes was diagnosed during follow-up. Those who reported only having diabetes during pregnancy (i.e., gestational diabetes) were included in the non-diabetic group.
For secondary analyses, we also identified baseline self-reported history of anti-diabetic medication use, including metformin (yes, no) and insulin (yes, no), among participants with T2D.
Outcome
The outcome of interest was first diagnosis of BCa. Incident cancer cases were identified through linkage to national cancer registries, which is considered to be the gold standard approach in the UK [14]. BCa was determined by an ICD-9 code of 174 or an ICD-10 code of C50. Follow-up data for the UK Biobank cohort were available until June 30, 2020 for England, January 31, 2019 for Wales, and 30 June 2018 for Scotland, at which points the relevant cancer registries last captured a BCa diagnosis.
Covariates
Multivariable models were adjusted for a set of confounding and BCa risk factors determined a priori, namely age at baseline assessment (continuous), self-reported race (white, non-white), Townsend Deprivation Index (TDI; quintiles; higher scores indicate greater levels of deprivation or socioeconomic disadvantage) [15], BMI (<25.0, 25.0−< 30.0, ≥30.0 kg/m2), physical activity (<20, 20− < 40, 40− < 60, ≥60 metabolic equivalent hours (METh)/week, unknown), smoking status and intensity (never, former, current <15 cigarettes/day, current ≥15 cigarettes/day, current intensity unknown), alcohol consumption (never, special occasions or 1–3 times per month, 1–4 times per week, daily or almost daily), educational level (higher, secondary, vocational, other), family history of BCa in a mother or sister (yes, no), ever mammography (yes, no), ever use of oral contraceptives (OCs; yes, no), ever use of hormone replacement therapy (HRT; yes, no), age at menarche (<12, 12–13, 14–15, ≥16 years), menopausal status (pre, post; age 50 was used as a proxy for menopausal status for the <5% of women for whom data for this field were missing); parity (nulliparous, 1, 2, ≥3 children), and age at first live birth (nulliparous, <20 years, 20– < 29, ≥30). All covariables were measured at baseline.
To explore possible underlying mechanisms of any relationship between diabetes and BCa, a set of biomarkers was identified for additional multivariable models. Per the protocol of the UK Biobank Biomarkers Project, blood samples were collected at the assessment centers, and serum concentrations of a range of key biomarkers were measured using a phased analysis approach [16]. For these analyses, we utilized testosterone (nmol/L), IGF-1 (nmol/L), sex hormone binding globulin (SHBG; nmol/L), C-reactive protein (CRP; mg/L), and haemoglobin A1c (HbA1c; mmol/mol). Estrogen was not considered due to substantial missingness.
Statistical analysis
Participants were followed from study enrollment until the first of the following events: BCa diagnosis, diagnosis of a different cancer, non-cancer-related radical mastectomy, death, or the last date at which follow-up was considered complete. The non-BCa endpoints were considered censoring events. Diabetes was treated as a time-varying exposure, wherein women with incident diabetes contributed person-years to the no diabetes group before their diagnosis of diabetes and contributed person-years to the diabetes group thereafter. Kaplan–Meier curves were used to summarize survival for women with diabetes (any diabetes, T1D, or T2D) at baseline compared to those without diabetes at baseline. Differences in survival by diabetes status and types were assessed using log-rank tests.
Cox proportional hazards models were employed to estimate hazard ratios (HRs) and 95% CIs for associations between diabetes and risk of BCa. Length of follow-up was the time scale in all models. Multivariable models were adjusted for the aforementioned set of covariables. In secondary analyses, we implemented multivariable models further categorizing women with T2D by metformin use (no, yes), insulin use (no, yes), and diabetes duration (<5, 5− < 10, 10− < 15, ≥15 years). Diabetes duration was calculated from the date of diabetes diagnosis to the date of BCa diagnosis or censoring. We tested the proportional hazards assumption using the Schoenfeld residual test and did not find evidence of a violation.
We assessed effect modification of associations between diabetes and BCa by the following variables, all measured at baseline: age at assessment (40− < 50, 50−< 60, ≥60 years), BMI (<25, 25− < 30, ≥30 kg/m2), ever had a mammogram (yes, no), ever HRT use (yes, no), age at menarche (<12, ≥12 years), menopausal status (pre, post), and parity (nulliparous, parous). Interactions between diabetes and potential effect modifiers were tested by entering cross-product terms into the multivariable models. In additional analyses, the aforementioned pre-determined biomarkers were entered in the multivariable models individually and in combination. The potential role of these serologic factors was evaluated with likelihood ratio tests.
Finally, we conducted several sensitivity analyses for the associations of diabetes and its two major types with BCa: (1) limiting exposure to incident diabetes; (2) redefining T1D as diagnosis prior to age 20 years; (3) redefining T2D as diagnosis after age 40 years; (4) excluding participants diagnosed with BCa within one year of study entry or diabetes diagnosis; (5) using Fine and Gray competing risks analysis to account for malignant cancers other than breast and death; (6) using age as the underlying time scale; (7) and including an interaction term between diabetes (or diabetes subtype) and BMI.
All statistical tests were two-sided with P < 0.05 considered to be statistically significant. Analyses were conducted using R statistical software, version 4.0.2.
Results
Our study included 575 women with T1D at baseline, 7891 women with T2D at baseline, 6821 women who developed T2D over a median follow-up of 11.1 years (interquartile range: 10.4–11.8 years), and 235,025 women who had never been diagnosed with either type of diabetes by the end of follow-up (Table 1). Compared to non-diabetic participants, women with either type of diabetes were more likely to be non-White, have higher TDIs, and never have used OCs. Women with T1D were also less likely to have ever had a mammogram, be postmenopausal, and be parous at baseline. Women with prevalent versus incident T2D had similar baseline characteristics, excepting the substantially less frequent use of metformin or insulin for the latter women. Relative to both non-diabetic women and women with T1D, women with T2D consumed less alcohol and had less education. They were also more likely to have higher BMI, have undergone mammography, have ever used HRT, and be postmenopausal than non-diabetic women. Regarding serum markers, women with T1D demonstrated the highest levels of SHBG and HbA1c, while the participants with T2D had the lowest levels of SHBG but the highest serum concentrations of CRP. In all, 76.3% of the participants with T1D and 53.8% of the participants with prevalent T2D had elevated HbA1c (HbA1c ≥47.5 mmol/mol). Among women who developed incident diabetes during follow-up, 13.6% had elevated HbA1c at baseline versus 0.33% in those who did not develop diabetes.
Women without diabetes contributed nearly 2.6 million person-years of follow-up versus 119,481 person-years among those with diabetes (Table 2). There were 7745 incident BCa diagnoses in the former group and 383 in the latter. Based on Kaplan–Meier curves, women with diabetes demonstrated similar times to developing BCa as the non-diabetic group (P = 0.20; Fig. 1). The incidence rates of BCa per 100,000 person-years were 300.5 for non-diabetic women and 320.6 for diabetic women. Multivariable Cox models also indicated no overall association between diabetes and BCa risk (adjusted hazard ratio (aHR) = 1.02, 95% CI = 0.92–1.14). Similarly, having T2D was not associated with BCa (aHR = 1.00, 95% CI = 0.90–1.12). Women with T1D, however, had a higher incidence rate of BCa compared to women without diabetes (428.0 vs. 300.5 cases/100,000 person-years), and multivariable models suggested a positive association between history of T1D and developing BCa (aHR = 1.52, 95% CI = 1.03–2.23).
Relative to women without diabetes, neither baseline metformin nor insulin use among women with T2D was associated with BCa risk (Table 2). However, increasing duration of T2D was significantly associated with reduced BCa risk (P for trend <0.001). The risk of BCa was highest in the first 5 years after T2D diagnosis (aHR = 3.94, 95% CI = 3.23–4.80). With increasing time more than 5 years after T2D diagnosis, BCa risk consistently declined. The direction of the association between T2D and BCa reversed after 10 years since T2D diagnosis (aHR = 0.66, 95% CI = 0.53–0.82) and was most strongly inverse among participants diagnosed with T2D more than 15 years prior to BCa diagnosis (aHR = 0.39, 95% CI = 0.30–0.50).
Associations for diabetes overall and T2D with BCa generally remained null in subgroups defined by age at assessment, BMI, ever had a mammogram, ever HRT use, age at menarche, menopausal status, and parity (Fig. 2 and Supplementary Table 1). However, T1D was linked to elevated BCa risk among women aged 60 and older (aHR = 2.40, 95% CI = 1.00–5.78), who had ever had a mammogram (aHR = 1.56, 95% CI = 1.01–2.43), who ever used HRT (aHR = 3.01, 95% CI = 1.35–6.73), who were postmenopausal (aHR = 1.65, 95% CI = 1.05–2.59), and who were parous (aHR = 1.68, 95% CI = 1.08–2.61). We did not observe statistically significant interactions between any of these variables and overall diabetes, T1D, or T2D (Fig. 2 and Supplementary Table 1).
Associations between diabetes and breast cancer risk in the UK Biobank cohort across subgroups defined by age at assessment, BMI, ever had a mammogram, ever HRT use, age at menarche, menopausal status, and parity. BMI body mass index, HRT hormone replacement therapy, kg/m2 kilograms per square meter.
Including serum markers in the multivariable models did not materially change the results (Supplementary Table 2). Results from sensitivity analyses restricting analysis to incident diabetes, redefining T1D and T2D, and excluding BCa cases that occurred within 1 year of baseline or diabetes diagnosis, and from models including an interaction term between diabetes or its subtypes with BMI were similar to the main findings (Supplementary Table 3). However, the results from Fine and Gray models accounting for the competing risks of malignant cancer other than breast and death and Cox proportional hazards models using age as the underlying time scale showed significantly reduced BCa risk for women with T2D (Supplementary Table 3). The cause-specific hazard function for competing events revealed that women with diabetes were likely to have other types of malignant cancer or death than women without diabetes.
Discussion
In this large prospective cohort of women in the UK with a median 11.1 years of follow-up, having diabetes was not generally associated with the risk of developing BCa. However, T1D was associated with an increased risk of BCa, and our data showed that women with T2D may be more likely to be diagnosed with BCa during the first decade after diabetes diagnosis.
Previous meta-analyses and large cohorts have indicated a modest increased risk of BCa among postmenopausal women with diabetes [7, 8, 10, 17]. However, studies have demonstrated substantial heterogeneity, and many have not adjusted for BMI—which is strongly associated with diabetes and a well-established risk factor for postmenopausal BCa—or other possible confounding factors. The overall null results of our study are consistent with results from a Women’s Health Initiative (WHI) multicenter study [18, 19], a study within the British Columbia Linked Health Databases (BCLHD) [20], and the most recently published findings from the Sister Study [21]. Consistent with the summary estimate, our null findings did not vary by age categories, menopausal status, BMI, or other BCa risk factors.
The few previous studies that have investigated BCa occurrence among persons with T1D have reported heterogeneous results [7, 13, 22,23,24]. Single-register studies have reported no association [7, 13, 22, 24], but a pooled analysis of five nationwide diabetes registers indicated a statistically significantly decreased risk of BCa in individuals with T1D [23]. These studies, however, did not adjust for BCa-specific risk factors, such as reproductive characteristics. Though we were able to adjust for such factors, our finding of a positive association between T1D and BCa risk should be interpreted with caution. Only 26 incident BCa cases were diagnosed among 576 women with T1D. In addition, all T1D was prevalent at baseline and diagnosed at a young age. Because our dataset did not include follow-up in the early window following T1D onset, we were unable to estimate BCa incidence in the short period following T1D diagnosis.
In our study, the hazard of BCa in participants with T2D showed a clear temporal trend, with an initial spike in the first 5 years following diabetes diagnosis and reduced BCa risk after 10 years from the diabetes index date. It is unlikely that BCa diagnosed shortly after diabetes onset is due to diabetes-related carcinogenesis. Rather, women with newly diagnosed diabetes likely have more frequent contact with health care providers and therefore have more BCa screening opportunities [25, 26]. Indeed, at baseline, a higher proportion of women with than without T2D in our cohort reported having ever undergone BCa screening. Failure to account for detection bias occurring in the early window after diabetes diagnosis may lead to overestimation of the association between diabetes and BCa risk.
More than 10 years after T2D diagnosis, BCa risk was statistically significantly inverse relative to individuals without T2D. T2D was also significantly associated with reduced BCa risk when using age as the underlying time scale in the Cox proportional hazards model. It is challenging to disentangle whether the pattern is solely due to the cumulative effects of T2D or some combination of disease duration, anti-diabetic medication use [21], and lifestyle modification. Survival bias could play a role if factors that improve survival of diabetic patients are associated with lower BCa risk. It is also possible that frequent censoring from competing causes in diabetic individuals results in fewer BCa cases over time. Certainly there is considerable evidence that diabetes is linked to an increased risk of several types of cancer [27] and independently increases mortality related to cardiovascular disease, renal disease, and cancer by 1.3–3.0 times [28]. Our Fine and Gray models indicated a significantly reduced BCa risk in women with diabetes. However, results from an a posteriori analysis of diabetes duration and BCa risk using Fine and Gray models indicated that the inverse association only presented with more than 10 years since diabetes diagnosis (data not shown). It is also plausible that individuals with longstanding chronic disease are less likely to receive routine cancer screening compared to the general population. To determine the likelihood that biology explains the inverse relationship between long-term diabetes and BCa, it would be important to rule out such biases.
In our analyses, metformin and insulin use among individuals with T2D were not associated with BCa risk compared to those without T2D. Biguanide metformin is the first-line medication for individuals with T2D, and in some situations, it has been repurposed as an anti-cancer drug [29]. Several mechanisms through which metformin could have anti-cancer properties have been proposed, most of which involve AMP kinase activation that leads to inhibition of the insulin/IGF-1 pathway, mammalian target of rapamycin (mTOR) pathway, and human epidermal growth factor receptor type 2 (HER-2) expression [29,30,31]. Multiple studies have suggested reduced BCa incidence and cancer-related mortality in individuals using metformin [32,33,34]. However, these findings may have been confounded by indication [2], since individuals prescribed metformin generally have been only recently diagnosed with diabetes and are in better health. Insulin and its analogs are hormonal treatments for glycemic control. Some studies have suggested that insulin increases the risk of BCa [35, 36], but other studies have been inconclusive [37, 38]. Studies of insulin and BCa may also experience confounding by indication, given that insulin is more often used among participants with a longer duration of T2D and in those with more comorbid conditions. Our results should be interpreted with caution because we assessed metformin and insulin use at baseline only, lacked information on medication dosage, frequency, and duration, and did not evaluate other types of anti-diabetic medications.
Strengths of this study include its prospective design, ICD coding of diabetes and BCa, linkage to cancer registries, available data for a relatively complete set of confounding factors, and the ability to explore anti-diabetic medications and possible biological links between diabetes and BCa. However, there are several limitations that deserve mention. First, competing risks are a concern since women with diabetes are less likely to develop BCa than other types of malignant cancer or death in the long term. Second, the incidence of BCa during follow-up—301 cases per 100,000 person-years—is higher than the estimated 210 cases per 100,000 females per year in the UK [39]. The difference may be attributable to the age distribution of the UK Biobank cohort compared to the general population. Third, the majority of the study participants were white. Generalizations of our results must thus be made cautiously. Fourth, it is essential to explore the relationships between diabetes and molecular subtypes of BCa, which have diverse etiologies and behaviors. Unfortunately, tumor molecular subtypes are currently unavailable in the UK Biobank. Fifth, data from the UK Biobank may include some measurement error, and we were unable to validate our exposure and outcome measurements. Finally, we had limited statistical power to examine the effect modifiers in the context of the association between T1D and BCa.
In conclusion, we did not observe associations between diabetes and BCa among women in the UK Biobank overall. However, our data suggested that women with T1D or recently diagnosed with T2D may have an increased BCa risk. Larger studies among other races/ethnicities are warranted to further investigate the relationship between T1D and BCa risk.
Data availability
Bona fide researchers can apply to use the open-access UK Biobank dataset by registering and applying at http://ukbiobank.ac.uk/register-apply/.
Code availability
Code is available from the authors upon request.
References
Cuadros DF, Li J, Musuka G, Awad SF. Spatial epidemiology of diabetes: methods and insights. World J Diabetes. 2021;12:1042–56.
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, et al. Diabetes and cancer: a consensus report. CA Cancer J Clin. 2010;60:207–21.
Cancer [Internet]. [cited 2021 Oct 24]. Available from: https://www.who.int/news-room/fact-sheets/detail/cancer
Hankinson SE, Willett WC, Colditz GA, Hunter DJ, Michaud DS, Deroo B, et al. Circulating concentrations of insulin-like growth factor-I and risk of breast cancer. Lancet Lond. Engl. 1998;351:1393–6.
Ferroni P, Riondino S, Buonomo O, Palmirotta R, Guadagni F, Roselli M. Type 2 diabetes and breast cancer: the interplay between impaired glucose metabolism and oxidant stress. Oxid Med Cell Longev. 2015;2015:183928.
Crave JC, Lejeune H, Brébant C, Baret C, Pugeat M. Differential effects of insulin and insulin-like growth factor I on the production of plasma steroid-binding globulins by human hepatoblastoma-derived (Hep G2) cells. J Clin Endocrinol Metab. 1995;80:1283–9.
Harding JL, Shaw JE, Peeters A, Cartensen B, Magliano DJ. Cancer risk among people with type 1 and type 2 diabetes: disentangling true associations, detection bias, and reverse causation. Diabetes Care. 2015;38:264–70.
Boyle P, Boniol M, Koechlin A, Robertson C, Valentini F, Coppens K, et al. Diabetes and breast cancer risk: a meta-analysis. Br J Cancer. 2012;107:1608–17.
Larsson SC, Mantzoros CS, Wolk A. Diabetes mellitus and risk of breast cancer: a meta-analysis. Int J Cancer. 2007;121:856–62.
Coughlin SS, Calle EE, Teras LR, Petrelli J, Thun MJ. Diabetes mellitus as a predictor of cancer mortality in a large cohort of US adults. Am J Epidemiol. 2004;159:1160–7.
UK Biobank: Protocol for a large-scale prospective epidemiological resource [http://www.ukbiobank.ac.uk/wpcontent/uploads/2011/11/UK-Biobank-Protocol.pdf] Access Oct 2021.
Xiong F, Dai Q, Zhang S, Bent S, Tahir P, Blarigan E, et al. Diabetes and incidence of breast cancer and its molecular subtypes: a systematic review and meta-analysis [Internet]. 2023. https://www.medrxiv.org/content/10.1101/2023.05.13.23289893v1
Zendehdel K, Nyrén O, Östenson CG, Adami HO, Ekbom A, Ye W. Cancer incidence in patients with type 1 diabetes mellitus: a population-based cohort study in Sweden. JNCI J Natl Cancer Inst. 2003;95:1797–800.
Conroy MC, Lacey B, Bešević J, Omiyale W, Feng Q, Effingham M, et al. UK Biobank: a globally important resource for cancer research. Br J Cancer. 2023;128:519–27.
Martin D. Townsend deprivation index [Internet]. Geo-Refer Proj. 2007. Available from: https://www.restore.ac.uk/geo-refer/36229dtuks00y19810000.php
serum_biochemistry.pdf [Internet]. [cited 2021 Jul 26]. Available from: https://biobank.ctsu.ox.ac.uk/showcase/showcase/docs/serum_biochemistry.pdf
Hardefeldt PJ, Edirimanne S, Eslick GD. Diabetes increases the risk of breast cancer: a meta-analysis. Endocr Relat Cancer. 2012;19:793–803.
Gong Z, Aragaki AK, Chlebowski RT, Manson JE, Rohan TE, Chen C, et al. Diabetes, metformin and incidence of and death from invasive cancer in postmenopausal women: results from the women’s health initiative. Int J Cancer. 2016;138:1915–27.
Chlebowski RT, McTiernan A, Wactawski-Wende J, Manson JE, Aragaki AK, Rohan T, et al. Diabetes, metformin, and breast cancer in postmenopausal women. J Clin Oncol Off J Am Soc Clin Oncol 2012;30:2844–52.
Bowker SL, Richardson K, Marra CA, Johnson JA. Risk of breast cancer after onset of type 2 diabetes. Diabetes Care. 2011;34:2542–4.
Park YMM, Bookwalter DB, O’Brien KM, Jackson CL, Weinberg CR, Sandler DP. A prospective study of type 2 diabetes, metformin use, and risk of breast cancer. Ann Oncol. 2021;32:351–9.
Hsu PC, Lin WH, Kuo TH, Lee HM, Kuo C, Li CY. A population-based cohort study of all-cause and site-specific cancer incidence among patients with type 1 diabetes mellitus in Taiwan. J Epidemiol. 2015;25:567–73.
Carstensen B, Read SH, Friis S, Sund R, Keskimäki I, Svensson AM, et al. Cancer incidence in persons with type 1 diabetes: a five-country study of 9,000 cancers in type 1 diabetic individuals. Diabetologia. 2016;59:980–8.
Swerdlow AJ, Laing SP, Qiao Z, Slater SD, Burden AC, Botha JL, et al. Cancer incidence and mortality in patients with insulin-treated diabetes: a UK cohort study. Br J Cancer. 2005;92:2070–5.
Bowker SL, Richardson K, Marra CA, Johnson JA. Risk of breast cancer after onset of type 2 diabetes: evidence of detection bias in postmenopausal women. Diabetes Care. 2011;34:2542–4.
Johnson JA, Bowker SL, Richardson K, Marra CA. Time-varying incidence of cancer after the onset of type 2 diabetes: evidence of potential detection bias. Diabetologia. 2011;54:2263.
Wojciechowska J, Krajewski W, Bolanowski M, Kręcicki T, Zatoński T. Diabetes and cancer: a review of current knowledge. Exp Clin Endocrinol Diabetes. 2016;124:263–75.
Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, et al. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet. 2020;396:2019–82.
Kirtonia A, Gala K, Fernandes SG, Pandya G, Pandey AK, Sethi G, et al. Repurposing of drugs: an attractive pharmacological strategy for cancer therapeutics. Semin Cancer Biol. 2021;68:258–78.
Shi Y, Hu FB. The global implications of diabetes and cancer. Lancet. 2014;383:1947–8.
Rojas LBA, Gomes MB. Metformin: an old but still the best treatment for type 2 diabetes. Diabetol Metab Syndr. 2013;5:6.
Libby G, Donnelly LA, Donnan PT, Alessi DR, Morris AD, Evans JMM. New users of metformin are at low risk of incident cancer: a cohort study among people with type 2 diabetes. Diabetes Care. 2009;32:1620–5.
Bodmer M, Meier C, Krähenbühl S, Jick SS, Meier CR. Long-term metformin use is associated with decreased risk of breast cancer. Diabetes Care. 2010;33:1304–8.
Jiralerspong S, Palla SL, Giordano SH, Meric-Bernstam F, Liedtke C, Barnett CM, et al. Metformin and pathologic complete responses to neoadjuvant chemotherapy in diabetic patients with breast cancer. J Clin Oncol. 2009;27:3297–302.
Wu JW, Azoulay L, Majdan A, Boivin JF, Pollak M, Suissa S. Long-term use of long-acting insulin analogs and breast cancer incidence in women with type 2 diabetes. J Clin Oncol. 2017;35:3647–53.
Wang L, Zhang HJ, Liu YF, Chen GY. Impact of insulin use on outcomes of diabetic breast cancer patients: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci. 2021;25:3507–18.
Overbeek JA, van Herk-Sukel MP, Vissers PAJ, van der Heijden AA, Bronsveld HK, Herings RMC, et al. Type 2 diabetes, but not insulin (analog) treatment, is associated with more advanced stages of breast cancer: a national linkage of cancer and pharmacy registries. Diabetes Care. 2019;42:434–42.
Dejgaard A, Lynggaard H, Råstam J, Thomsen MK. No evidence of increased risk of malignancies in patients with diabetes treated with insulin detemir: a meta-analysis. Diabetologia. 2009;52:2507–12.
Breast cancer statistics [Internet]. Cancer Res. 2021. Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/breast-cancer
Acknowledgements
Data from the UK Biobank resource were obtained under application number 14105. We gratefully acknowledge Dr. Travis J. Meyers for his contributions to the data analyses and Dr. Jeffrey Martin for his critical feedback.
Funding
JMC receives funding from the Cancer League Foundation. REG is supported by a Young Investigator Award from the Prostate Cancer Foundation.
Author information
Authors and Affiliations
Contributions
FX, CH, GS, and REG designed the project. FX, JW, and JLN performed the data curation and statistical analyses. FX and REG interpreted the data and prepared the initial draft manuscript. GS, CH, and REG supervised the development of the work. JW, JLN, ELVB, SAK, JMC, GS, CH, and REG made critical revisions of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
JMC declares that her husband is a full-time employee of Adela, Inc. and a prior employee of GRAIL (within the past 3 years).
Ethics approval and consent to participate
The UK Biobank’s study protocol was approved by the UK North West Multicenter Research Ethics Committee. Each participant provided written informed consent to participate.
Consent for publication
No relevant identifiable participant data.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiong, F., Wang, J., Nierenberg, J.L. et al. Diabetes mellitus and risk of breast cancer: a large-scale, prospective, population-based study. Br J Cancer 129, 648–655 (2023). https://doi.org/10.1038/s41416-023-02345-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02345-4
This article is cited by
-
Two-dimensional polymeric cobalt phthalocyanine synthesized by microwave irradiation and its use for continuous glucose monitoring
Korean Journal of Chemical Engineering (2023)