Abstract
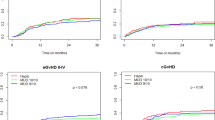
Adolescent and young adult (AYA) patients with acute leukemia (AL) have inferior outcomes in comparison to younger patients, and are more likely to develop acute and chronic GVHD than younger children following HLA matched sibling donor stem cell transplant (SCT). We compared the incidence of grade II–IV acute GVHD, chronic GVHD, and survival in AYA (age 13–21 years) to younger children (age 2–12 years) who received an unrelated donor SCT for acute leukemia on Children’s Oncology Group trials between 2004–2017. One hundred and eighty-eight children and young adults ages 2–21 years underwent URD SCT. Sixty-three percent were aged 2–12 and 37% were age 13–21. Older age was a risk factor for grade II–IV acute GVHD in multivariate analysis with a hazard ratio (HR) of 1.95 [95% confidence interval (CI) 1.23–3.10], but not for chronic GVHD, HR 1.25 [95% CI 0.57–2.71]. Younger patients relapsed more often (34.5 ± 4.4% vs. 22.8 ± 4.0%, p = 0.032), but their Event-Free Survival (42.6 ± 4.7% vs. 51.8 ± 6.1%, p = 0.18) and Overall Survival at 5 years (48.5 ± 4.9% vs. 51.5 ± 6.4%, p = 0.56) were not different than AYA patients. AYA patients who receive an URD SCT for acute leukemia are significantly more likely to develop grade II–IV acute GVHD, though survival is similar.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Bleyer A, Barr R, Hayes-Lattin B, Thomas D, Ellis C, Anderson B. The distinctive biology of cancer in adolescents and young adults. Nat Rev Cancer. 2008;8:288–98. https://doi.org/10.1038/nrc2349. e-pub ahead of print 2008/03/21.
McNeer JL, Bleyer A. Acute lymphoblastic leukemia and lymphoblastic lymphoma in adolescents and young adults. Pediatr Blood Cancer. 2018;65:e26989 https://doi.org/10.1002/pbc.26989. e-pub ahead of print 2018/02/09.
Creutzig U, Kutny MA, Barr R, Schlenk RF, Ribeiro RC. Acute myelogenous leukemia in adolescents and young adults. Pediatr Blood Cancer. 2018;65:e27089 https://doi.org/10.1002/pbc.27089.
Curran E, Stock W. How I treat acute lymphoblastic leukemia in older adolescents and young adults. Blood. 2015;125:3702–10. https://doi.org/10.1182/blood-2014-11-551481. e-pub ahead of print 2015/03/26.
Hochberg J, Khaled S, Forman SJ, Cairo MS. Criteria for and outcomes of allogeneic haematopoietic stem cell transplant in children, adolescents and young adults with acute lymphoblastic leukaemia in first complete remission. Br J Haematol. 2013;161:27–42. https://doi.org/10.1111/bjh.12239. e-pub ahead of print 2013/02/07.
Eisner MD, August CS. Impact of donor and recipient characteristics on the development of acute and chronic graft-versus-host disease following pediatric bone marrow transplantation. Bone Marrow Transpl. 1995;15:663–8.
Zecca M, Prete A, Rondelli R, Lanino E, Balduzzi A, Messina C, et al. Chronic graft-versus-host disease in children: incidence, risk factors, and impact on outcome. Blood. 2002;100:1192–1200. https://doi.org/10.1182/blood-2001-11-0059.
Qayed M, Wang T, Hemmer MT, Spellman S, Arora M, Couriel D. et al. Influence of age on acute and chronic GVHD in children undergoing HLA-identical sibling bone marrow transplantation for acute leukemia: implications for prophylaxis. Biol Blood Marrow Transpl. 2018;24:521–8. https://doi.org/10.1016/j.bbmt.2017.11.004.
Chaudhury SS, Morison JK, Gibson BE, Keeshan K. Insights into cell ontogeny, age, and acute myeloid leukemia. Exp Hematol. 2015;43:745–55. https://doi.org/10.1016/j.exphem.2015.05.008.
Bleyer A, Budd T, Montello M. Adolescents and young adults with cancer: the scope of the problem and criticality of clinical trials. Cancer. 2006;107:1645–55. https://doi.org/10.1002/cncr.22102.
Smith AW, Keegan T, Hamilton A, Lynch C, Wu XC, Schwartz SM, et al. Understanding care and outcomes in adolescents and young adult with Cancer: A review of the AYA HOPE study. Pediatr Blood Cancer. 2019;66:e27486 https://doi.org/10.1002/pbc.27486.
Pulsipher MA, Langholz B, Wall DA, Schultz KR, Bunin N, Carroll WL, et al. The addition of sirolimus to tacrolimus/methotrexate GVHD prophylaxis in children with ALL: a phase 3 Children’s Oncology Group/pediatric blood and marrow transplant consortium trial. Blood. 2014;123:2017–25. https://doi.org/10.1182/blood-2013-10-534297.
Gamis AS, Alonzo TA, Meshinchi S, Sung L, Gerbing RB, Raimondi SC, et al. Gemtuzumab ozogamicin in children and adolescents with de novo acute myeloid leukemia improves event-free survival by reducing relapse risk: results from the randomized phase III Children’s Oncology Group trial AAML0531. J Clin Oncol. 2014;32:3021–32. https://doi.org/10.1200/jco.2014.55.3628.
Aplenc R, Meshinchi S, Sung L, Alonzo T, Choi J, Fisher B, et al. Bortezomib with standard chemotherapy for children with acute myeloid leukemia does not improve treatment outcomes: a report from the Children’s Oncology Group. Haematologica. 2020;105:1879–86. https://doi.org/10.3324/haematol.2019.220962.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus conference on acute GVHD grading. Bone Marrow Transplant 1995;15:825–8.
Flowers ME, Kansu E, Sullivan KM. Pathophysiology and treatment of graft-versus-host disease. Hematol Oncol Clin North Am. 1999;13:1091–112. https://doi.org/10.1016/s0889-8588(05)70111-8.
Kalbfleisch JD, Prentice RL. The statistical analysis of failure time data. 2nd ed. New York: John Wiley & Sons; 2002.
Kleinbaum DG KLL, Nizam A., Rosenberg, E.S. Applied regression analysis and other multivariable methods. 5th ed. Cengage Learning: Boston, MA; 2013.
StataCorp. Stata statistical software: release 15. In: College Station. TX: StataCorp LLC.; 2017.
Pulsipher MA, Langholz B, Wall DA, Schultz KR, Bunin N, Carroll W, et al. Risk factors and timing of relapse after allogeneic transplantation in pediatric ALL: for whom and when should interventions be tested? Bone Marrow Transpl. 2015;50:1173–9. https://doi.org/10.1038/bmt.2015.103.
Yeshurun M, Weisdorf D, Rowe JM, Tallman MS, Zhang MJ, Wang HL, et al. The impact of the graft-versus-leukemia effect on survival in acute lymphoblastic leukemia. Blood Adv. 2019;3:670–80. https://doi.org/10.1182/bloodadvances.2018027003.
Woolfrey AE, Anasetti C, Storer B, Doney K, Milner LA, Sievers EL, et al. Factors associated with outcome after unrelated marrow transplantation for treatment of acute lymphoblastic leukemia in children. Blood. 2002;99:2002–8. https://doi.org/10.1182/blood.v99.6.2002.
Bitan M, Ahn KW, Millard HR, Pulsipher MA, Abdel-Azim H, Auletta JJ, et al. Personalized prognostic risk score for long-term survival for children with acute leukemia after allogeneic transplantation. Biol Blood Marrow Transpl. 2017;23:1523–30. https://doi.org/10.1016/j.bbmt.2017.05.011.
Bunin N, Carston M, Wall D, Adams R, Casper J, Kamani N, et al. Unrelated marrow transplantation for children with acute lymphoblastic leukemia in second remission. Blood. 2002;99:3151–7. https://doi.org/10.1182/blood.v99.9.3151.
Yang F, Lu D, Hu Y, Huang X, Huang H, Chen J, et al. Risk factors for graft-versus-host disease after transplantation of hematopoietic stem cells from unrelated donors in the china marrow donor program. Ann Transpl. 2017;22:384–401. https://doi.org/10.12659/aot.902805.
Tan J, Wang Y, Yu SJ, Ma YY, Lei HY, Liu QF. Prognostic factors on graft-versus-host disease-free and relapse-free survival after allogeneic hematopoietic stem cell transplantation for adults with acute leukemia. Leuk Res. 2017;59:1–7. https://doi.org/10.1016/j.leukres.2017.05.011.
Remberger M, Kumlien G, Aschan J, Barkholt L, Hentschke P, Ljungman P, et al. Risk factors for moderate-to-severe chronic graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2002;8:674–82. https://doi.org/10.1053/bbmt.2002.v8.abbmt080674.
Gassas A, Ishaqi MK, Afzal S, Finkelstein-Shechter T, Dupuis A, Doyle J. A comparison of the outcomes of children with acute myelogenous leukemia in either first or second complete remission (CR1 vs.CR2) following allogeneic hematopoietic stem cell transplantation at a single transplant center. Bone Marrow Transplant. 2008;41:941–5. https://doi.org/10.1038/bmt.2008.16.
Davies SM, Wang D, Wang T, Arora M, Ringden O, Anasetti C, et al. Recent decrease in acute graft-versus-host disease in children with leukemia receiving unrelated donor bone marrow transplants. Biol Blood Marrow Transplant. 2009;15:360–6. https://doi.org/10.1016/j.bbmt.2008.12.495.
Acknowledgements
The authors would like to thank the patients and families who participated in the Children’s Oncology Group stem cell transplant trials, as well as the physician investigators who collaborated with the authors. We also appreciate the collaborative efforts of the Cellular Therapy and Adolescent and Young Adult Children’s Oncology Group committees.
Funding
N01 HC-45220/HHSN268200425220C. COG Chair’s grant U10CA098543. U10CA180899. CA98413-08. U10CA180886. R01CA1116660. 2U01HL069254. St. Baldrick’s Foundation
Author information
Authors and Affiliations
Contributions
JRA, LJ, MSC designed the study; YW, LJ collected the data; all authors analyzed and interpreted the results; JRA, LJ, MSC wrote the initial manuscript; all authors edited the manuscript.
Corresponding authors
Ethics declarations
Competing interests
JL: Ironwood None Personal Fees, Incyte None Consultancy and Research Funding, Kamada None Research Funding, Biogen None non-financial support, Bluebird Bio Consultant Consultancy, Novartis Consultant Consultancy, Viracor Inventor Royalty. MAP: Miltenyi N/A Research Support and Educational honoraria, Adaptive N/A Research Suppor and Educational honoraria, Novartis Advisory Board, Study Steering Committee, Educational honoraria. Mesoblast, Advisory board. MSC: Jazz Advisory Board and Speaker Bureau, Amgen Speaker Bureau, Sanofi Speaker Bureau, Nektar Advisory Board, Servier Speaker Bureau. JA, LJ, YW, DF, AG, RA, and LH have nothing to disclose, financial or otherwise.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Andolina, J.R., Wang, YC., Ji, L. et al. Adolescent and young adult (AYA) versus pediatric patients with acute leukemia have a significantly increased risk of acute GVHD following unrelated donor (URD) stem cell transplantation (SCT): the Children’s Oncology Group experience. Bone Marrow Transplant 57, 445–452 (2022). https://doi.org/10.1038/s41409-021-01558-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01558-6