Abstract
Study design
Retrospective study.
Objective
To investigate the incidence of and factors associated with hyponatremia among traumatic cervical spinal cord injury (SCI) patients.
Setting
Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand.
Methods
This retrospective study included traumatic cervical SCI patients that were admitted to the Siriraj Spinal Unit during January 2002 to May 2013. Patient demographic and clinical data were collected.
Results
One hundred and twenty-three patients (98 males, 25 females) were enrolled. The mean age of patients was 47.2 ± 16.9 years (range: 11–84). There were 38 complete and 85 incomplete cord injuries. Seventy-six patients were treated surgically, and all others received conservative treatment. Hyponatremia developed in 54 patients (43.9%), and 74.1% of all cases of hyponatremia presented within 9 days after SCI. Hyponatremia occurred on the first day in 10 patients (18.5%), on the fifth day in 6 patients (11.1%), and on the eighth day in 5 patients (9.26%). Hyponatremia occurred in 6/10 patients (60.0%) with upper cervical spine injury (C1-2), and in 48/113 patients (42.5%) with lower cervical spine injury (C3-7) (odds ratio [OR]: 2.031, 95% confidence interval [CI]: 0.543–7.596; p = 0.292). The incidence of hyponatremia was 65.8% in complete SCI patients, and 34.1% in incomplete SCI patients. Logistic regression analysis revealed complete SCI to be the only factor significantly associated with hyponatremia (OR: 3.714, 95% CI: 1.658–8.317; p < 0.001).
Conclusion
Hyponatremia was found to be common in post-traumatic cervical SCI patients. Complete SCI was identified as the only factor significantly associated with hyponatremia in traumatic cervical SCI patients.
Similar content being viewed by others
Introduction
Hyponatremia, which is defined as an abnormally high water to sodium ratio in extracellular fluid, is a commonly observed electrolyte imbalance in hospitalized patients [1, 2]. Mild hyponatremia (serum sodium <135 mmol per liter) develops in 15–20% of patients admitted to the hospital, and in ~7% of nonhospitalized patients [3]. Medium-severity hyponatremia (serum sodium <130 mmol/l) emerges in 1–7% of in-hospital patients [4, 5]. Sympathetic dysfunction-associated hyponatremia and hypotension are major acute-stage complications that develop following trauma-related cervical spinal cord injury (SCI) [6,7,8,9,10,11]. Heightened activity in renal sympathetic nerves increases renal tubular water and sodium reabsorption within the nephron, lowers glomerular filtration and blood flow in the kidney by contracting the renal blood vessels, and facilitates renin release via juxtaglomerular granular cells, which results in increased endogenous renin–angiotensin–aldosterone activity [7, 12, 13].
Mortality among patients with symptomatic hyponatremia is much higher than among normonatremic patients [14]. The causes of hyponatremia vary and requires proper management. Thailand is middle income country. The traffic problems and development of industrial works increase significantly the number of spinal cord injured patients. Siriraj spinal unit was the first spinal center setting up more than 15 years in Siriraj Hospital, Mahidol University which is one of the world well known medical school and university hospital. It is our strategies to develop high efficiency of early management, reducing mobility and mortality as well as improving the quality of life in spinal cord injured patients.
This study aims to encourage the recognition of hyponatremia condition following acute SCI. The study presents the information of incidence and influencing factors of hyponatremia (serum sodium <135 mmol/l) following acute cervical SCI. Awareness and early effective management will minimize complicated cases with better outcomes to achieve the goal.
Methods
All patients with acute cervical SCI who were transported to the spinal unit of Siriraj Hospital (Bangkok, Thailand) during January 2002 to May 2013 were retrospectively enrolled. Patient demographic and clinical data were collected from patient medical records and from our center’s patient information database. We excluded patients with previously diagnosed chronic hyponatremia, head injury, or systemic or renal disease. We also excluded patients that often took medication that can affect electrolyte level (e.g., carbamazepine, enema, laxative, diuretic, angiotensin-converting enzyme inhibitors) and none of patients received methylprednisolone at acute phase. This study received institutional review board approval (COA no. 86/2014 [EC1]).
Data that were collected included age, gender, cause of injury, severity (complete or incomplete SCI) and level of SCI, serum sodium level, treatment strategy (conservative treatment or surgery), and day of presentation of hyponatremia after injury. A serum sodium concentration <135 mmol/L defined hyponatremia in our study, and we categorized cervical SCI as either high (C1-2) or low (C3-7).
Statistical analysis
All data analyses were performed using SPSS statistical analysis software. Categorical data are given as number or number and percentage, and continuous data are described as mean ± standard deviation. Chi-square test or Fisher’s exact test was used to assess categorical data, and Student’s t test was used to evaluate continuous data. Logistic regression analysis was used to identify factors significantly associated with hyponatremia. Statistical significance was defined as a p value < 0.05.
Results
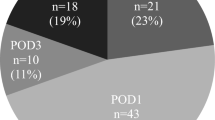
This study included 123 traumatic cervical SCI patients. There were 98 males and 25 females, with a mean age of 47.2 years (range: 11–84). Motorcycle accident was the leading cause of injury (70/123, 56.9%), followed by simple fall (25/123, 20.3%), fall from height (18/123, 14.6%), and gunshot wound (4/123, 3.3%). Concerning the severity of SCI using the American Spinal Injury Association (ASIA) [15] Impairment Scale, there were 38 (30.9%) complete SCI patients, and 85 (69.1%) incomplete SCI patients. The mean length of hospital stay was 131.4 days (median: 65 days) (Table 1). The distribution of injury level was C1 in 3 cases (2.4%), C2 in 7 cases (5.7%), C3 in 25 cases (20.3%), C4 in 25 cases (20.3%), C5 in 34 cases (27.6%), C6 in 19 cases (15.4%), and C7 in 10 cases (8.1%) (Table 1). Fifty-four patients (43.9%) had hyponatremia (Na < 135 mmol/L), and 69 (56.1%) had normal serum sodium (Na ≥ 135 mmol/L) (Table 2). Regarding course of treatment, 76 (61.8%) patients had surgery, and 47 (38.2%) patients received conservative management. Among the 54 hyponatremia patients, 40 (74.1%) developed hyponatremia within 9 days after sustaining their injury. Peak hyponatremia was observed on the first day after injury in 10/54 (18.5%) patients, on day 5 after injury in 6/54 (11.1%) patients, and on day 8 after injury in 5/54 (11.1%) patients (Fig. 1). Among the 54 patients who developed hyponatremia, the distribution of level of SCI was C3 injury in 13/54 (24.1%), C4 in 11/54 (20.4%), C5 in 10/54 (18.5%), C6 in 10/54 (18.5%), C7 in 4/54 (7.4%), C2 in 4/54 (7.4%), and C1 in 2/54 (3/7%) (Fig. 2).
Hyponatremia occurred 2 times more often in patients with upper cervical spine injury (C1-2) (6/10, 60%) than in patients with lower cervical spine injury (C3-7) (48/113, 42.5%), but the difference between groups did not achieve statistical significance (odds ratio [OR]: 2.031, 95% confidence interval [CI]: 0.543–7.596; p = 0.292) (Table 3).
Of the 25 patients with complete SCI, 65.8% developed hyponatremia, and 29 of 113 (34.1%) incomplete SCI patients developed hyponatremia. Logistic regression analysis revealed complete SCI (ASIA Impairment Scale score A) to be the only factor significantly associated with hyponatremia (OR: 3.714, 95% CI: 1.658–8.317; p < 0.001) (Table 3). No significant association was found between hyponatremia and age, gender, or level of cervical SCI.
Discussion
Hyponatremia is common in patients with neurological conditions, and the prevalence of hyponatremia is known to be much higher in patients with acute SCI than in general medical or surgical patients. Hyponatremia is commonly observed after SCI, and the reported incidence ranged from 29% to 86% [6, 8, 16,17,18].
In this present study, hyponatremia developed in 54 of 123 (43.9%) SCI during the early period following trauma-related cervical SCI, and most of those developed hyponatremia within the first 9 days post-SCI. Hyponatremia developed on the first day in 18.5% of patients with hyponatremia, on the fifth day in 46.3%, and on the ninth day in 74.1%. This result is consistent with another study that found hyponatremia in 86 of 172 (50%) patients with SCI [19]. Furlan and Fehlings et al. reported hyponatremia to be significantly more common in SCI than in controls during the first 2 weeks after hospitalization following trauma-related spine injury, and hyponatremia persisted for 4 to 6 days (mean: 5.3 days, median: 6 days) after acute traumatic SCI [8]. Peruzzi et al. reported that hyponatremia developed an average of 6.4 ± 6.7 days after admission, and it reached its nadir at a mean 8.7 ± 8.8 days [17]. Of 134 patients with spinal injuries, 25 developed hyponatremia within 2 days of injury at a hospital in the UK [6]. These results and reported findings indicate that hyponatremia is highly likely to develop within the first 2 weeks post-SCI, so patient sodium levels should be carefully monitored during this period to improve early diagnosis and treatment to prevent morbidity and mortality.
Hyponatremia frequently occurs in traumatic SCI. Patients with mild hyponatremia, which is defined as a serum Na concentration ranging within 130–135 mmol/l, are commonly asymptomatic during the first days after injury. Although treatment is generally not required, these patients should be carefully watched because the administration of intravenous fluid may be required in some cases. Signs and symptoms that may be demonstrated in patients with a plasma Na concentration <130 mmol/l include anorexia, nausea, vomiting, disorientation, and headache [20]. Substantially increased mortality was also reported to be associated with plasma Na concentration <130 mmol/l [4], so careful observation and appropriate treatment are essential. Reported causes of hyponatremia include morphological alteration in sympathetic ganglion neurons, the descending vasomotor pathway, and/or the descending renal sympathetic pathway [21, 22].
Our research group previously reported a mean length of hospital stay (LOS) of 96.2 days among complete cervical SCI, and that hyponatremia lengthened the LOS and increases the cost of care and hospitalization [23]. In the present study, we found a non-significant trend towards a higher incidence of hyponatremia among older patients compared to younger patients. However, multivariate analysis performed in another study revealed older age to be a risk factor for hyponatremia after SCI [20]. Hyponatremia may be more likely to develop among older SCI due to physiological changes of aging, such as hormonal changes and sclerotic change in the vascular system. However, little is known about the relationship between hyponatremia after SCI and older age status.
In this study, the incidence of hyponatremia was 60% in the upper level (C1-2) SCI group compared to 42.5% in the lower level (C3-7) SCI group, but the difference between groups was not statistically significant (OR: 2.031, 95% CI: 0.543–7.596; p = 0.292). Even though no significant association was found, our finding may heighten physician awareness for a potential higher likelihood of hyponatremia in upper level injury patients. Peruzzi et al. reported hyponatremia in 28% of patients with cervical injuries, in 34% with thoracic injuries, and in 27% with lumbar injuries (p > 0.05) [17]. Therefore, our results and previously reported results suggest that level of injury does not significantly influence the likelihood of hyponatremia.
Among the 123 patients included in our study, there were 38 (30.9%) complete SCI patients, and 85 (69.1%) incomplete SCI patients. Of the 25 patients with complete SCI, 65.8% developed hyponatremia, and 29 of 113 (34.1%) incomplete SCI patients developed hyponatremia. Logistic regression analysis revealed complete SCI to be the only factor significantly associated with hyponatremia (OR: 3.714, 95% CI: 1.658–8.317; p < 0.001). Compared to others studies, Nakao et al. reported that during acute and subacute periods, patients with more severe SCI according to ASIA impairment scale (AIS) classification had a higher frequency of hyponatremia [19]. Peruzzi et al. found the most significant predictor of hyponatremia to be related to degree of severity classification of SCI, not to the level of injury [17]. Frisbie reported severity of SCI to be significantly related to decreased sodium conservation and hyponatremia [7]. The findings of the present and previous studies suggest strong association between severity of SCI and more severe hyponatremia.
Increased incidence of hyponatremia in patients with higher severity of SCI is multifactorial. First, renal conservation of sodium may be impaired due to sympathetic denervation of the kidney or impaired renal blood flow [7]. Second, antidiuretic hormone is secreted in extremely high concentrations in response to orthostatic hypotension [24]. Third, failure of the tetraplegic patient to excrete water load after the suppression of ADH, which suggests an ADH-independent mechanism of renal conservation of water [25]. Fourth, increased intake of water as evidenced by polyuria provides ample substrate for ADH expression. In summary, hyponatremia in SCI can be related to the effects of enhanced water conservation, increased fluid intake, and partially blocked sodium conservation [7].
Limitations
The limitations of this study are hereafter described. The first limitation includes the collective limitations of retrospective research compared to prospective research, including missing and incomplete information. Second, the relatively small size of our study population may have limited our study’s power to statistically identify all significant associations and differences. Third and last, the Siriraj Spinal Unit is a highly specialized care setting, so our findings may not be fully generalizable to settings with less sophisticated levels of care. Further multicenter study in a much larger population of traumatic cervical SCI will help to elucidate if level of care influences the incidence of hyponatremia in this patient population.
Conclusion
Hyponatremia was found to be common among post-traumatic cervical SCI patients. Three-quarters (74.1%) of all hyponatremia presented within 9 days after SCI, and peak hyponatremia occurred on day one in 10 patients (18.5%). The vast majority of hyponatremia (60.0%) occurred in patients with upper cervical spine injury (C1-2). Logistic regression analysis revealed complete SCI to be the only factor significantly associated with hyponatremia in our study population. Prompt diagnosis and treatment of hyponatremia is necessary to prevent morbidity and mortality, so careful monitoring of sodium level after traumatic cervical SCI is essential.
Data availability
All data generated or analysed during this study are included in this published article.
References
Adrogué HJ, Madias NE. Hyponatremia. N Engl J Med. 2000;342:1581–9. https://doi.org/10.1056/nejm200005253422107.
Baran D, Hutchinson TA. The outcome of hyponatremia in a general hospital population. Clin Nephrol. 1984;22:72–6.
Hennrikus E, Ou G, Kinney B, Lehman E, Grunfeld R, Wieler J, et al. Prevalence, timing, causes, and outcomes of hyponatremia in hospitalized orthopaedic surgery patients. J Bone Jt Surg Am. 2015;97:1824–32. https://doi.org/10.2106/jbjs.O.00103.
Anderson RJ, Chung HM, Kluge R, Schrier RW. Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med. 1985;102:164–8. https://doi.org/10.7326/0003-4819-102-2-164.
Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119:S30–5. https://doi.org/10.1016/j.amjmed.2006.05.005.
Biyani A, Inman CG, el Masry WS. Hyponatraemia after acute spinal injury. Injury. 1993;24:671–3. https://doi.org/10.1016/0020-1383(93)90318-z.
Frisbie JH. Salt wasting, hypotension, polydipsia, and hyponatremia and the level of spinal cord injury. Spinal Cord. 2007;45:563–8. https://doi.org/10.1038/sj.sc.3101984.
Furlan JC, Fehlings MG. Hyponatremia in the acute stage after traumatic cervical spinal cord injury: clinical and neuroanatomic evidence for autonomic dysfunction. Spine. 2009;34:501–11. https://doi.org/10.1097/BRS.0b013e31819712f5.
Palmer BF. Hyponatremia in patients with central nervous system disease: SIADH versus CSW. Trends Endocrinol Metab. 2003;14:182–7. https://doi.org/10.1016/s1043-2760(03)00048-1.
Richard B, Rodgers EMH, Volker KH Sonntag. Acute treatment of patients with spinal cord injury. In: Herkowitz HN, editor. The spine. 2. Philadelphia, Pa.: Saunders/Elsevier; 2011. p. 1422–35.
Teasell RW, Arnold JM, Krassioukov A, Delaney GA. Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system after spinal cord injury. Arch Phys Med Rehabil. 2000;81:506–16. https://doi.org/10.1053/mr.2000.3848.
DiBona GF. Neural control of the kidney: functionally specific renal sympathetic nerve fibers. Am J Physiol Regul Integr Comp Physiol. 2000;279:R1517–24. https://doi.org/10.1152/ajpregu.2000.279.5.R1517.
DiBona GF. Nervous kidney. Interaction between renal sympathetic nerves and the renin-angiotensin system in the control of renal function. Hypertension. 2000;36:1083–8. https://doi.org/10.1161/01.hyp.36.6.1083.
Anderson RJ. Hospital-associated hyponatremia. Kidney Int. 1986;29:1237–47. https://doi.org/10.1038/ki.1986.134.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46. https://doi.org/10.1179/204577211x13207446293695.
Claydon VE, Krassioukov AV. Orthostatic hypotension and autonomic pathways after spinal cord injury. J Neurotrauma. 2006;23:1713–25. https://doi.org/10.1089/neu.2006.23.1713.
Peruzzi WT, Shapiro BA, Meyer PR Jr., Krumlovsky F, Seo BW. Hyponatremia in acute spinal cord injury. Crit Care Med. 1994;22:252–8. https://doi.org/10.1097/00003246-199402000-00016.
Soni BM, Vaidyanthan S, Watt JW, Krishnan KR. A retrospective study of hyponatremia in tetraplegic/paraplegic patients with a review of the literature. Paraplegia. 1994;32:597–607. https://doi.org/10.1038/sc.1994.95.
Nakao Y, Suda K, Shimokawa N, Fu Y. Risk factor analysis for low blood pressure and hyponatremia in acutely and subacutely spinal cord injured patients. Spinal Cord. 2012;50:285–8. https://doi.org/10.1038/sc.2011.142.
Moore K, Thompson C, Trainer P. Disorders of water balance. Clin Med. 2003;3:28–33. https://doi.org/10.7861/clinmedicine.3-1-28.
Ellison DH, Berl T. Clinical practice. The syndrome of inappropriate antidiuresis. N Engl J Med. 2007;356:2064–72. https://doi.org/10.1056/NEJMcp066837.
Hannon MJ, Thompson CJ. The syndrome of inappropriate antidiuretic hormone: prevalence, causes and consequences. Eur J Endocrinol. 2010;162 Suppl 1:S5–12. https://doi.org/10.1530/eje-09-1063.
Chavasiri C, Wilartratsami S, Ruangchainikom M, Korwutthikulrangsri E, Luksanapruksa P. Demographic and clinical profiles of traumatic spinal injury patients at the Siriraj Spinal Unit-Southeast Asia’s first dedicated spinal injury center. J Med Assoc Thail. 2019;102:79–85.
Jacob G, Ertl AC, Shannon JR, Furlan R, Robertson RM, Robertson D, et al. Effect of standing on neurohumoral responses and plasma volume in healthy subjects. J Appl Physiol. 1998;84:914–21. https://doi.org/10.1152/jappl.1998.84.3.914.
Leehey DJ, Picache AA, Robertson GL. Hyponatraemia in quadriplegic patients. Clin Sci. 1988;75:441–4. https://doi.org/10.1042/cs0750441.
Acknowledgements
The authors gratefully acknowledge Miss Krabkaew Soparat and Mr. Pongsathorn Samphaothong of the Orthopedic Research Unit of the Department of Orthopedic Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University for performing the statistical analyses, manuscript preparation, and the journal submission process.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chavasiri, C., Suriyachat, N., Luksanapruksa, P. et al. Incidence of and factors associated with hyponatremia in traumatic cervical spinal cord injury patients. Spinal Cord Ser Cases 8, 15 (2022). https://doi.org/10.1038/s41394-022-00475-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00475-0