Abstract
Background
We aimed to identify the impact of COVID infection in children in the US prior to vaccine availability on clinical and healthcare utilization outcomes within 6 months of infection.
Methods
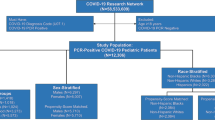
Using claims data from a large national insurer, we identified 223,842 children with a COVID diagnosis in May 2020–March 2021 and matched them to 223,842 children with a COVID test and no diagnosis. We compared the two cohorts’ outcomes during the 6 months after infection/test.
Results
Uncommon acute adverse events occurring in <0.5% of cases, including MIS-C (relative risk (RR) = 45.2), myocarditis (RR = 10.3), acute heart failure (RR = 2.14), sepsis (RR = 2.02), and viral pneumonia (RR = 2.43) were more frequent in the COVID cohort (all p < 0.001). Development of arrhythmias (RR = 1.24, p < 0.001) and atherosclerotic cardiovascular disease (RR = 1.41, p = 0.007) were more common in the COVID group, while behavioral health disorders were less common (RR = 0.94, p < 0.001). Lab testing and imaging were slightly higher in the COVID group (RR ranging 1.05–1.11 depending on the service and timeframe), though medical costs did not increase.
Conclusion
Severe disease and diagnoses of new conditions are rare in children following COVID infection. We observed an increase in cardiac complications, though they may not last long term.
Impact
-
Few studies have analyzed the association between COVID infection and medium-term outcomes in children.
-
Our study of >447,000 geographically and socioeconomically diverse children in the US found that uncommon acute adverse events, including myocarditis, MIS-C, and acute heart failure, were more frequent in children with COVID than matched controls, and development of arrhythmias and cardiovascular disease were 1.2 and 1.4 times more common, respectively.
-
Six-month healthcare utilization was similar between cohorts.
-
We provide data on the risks of COVID in children, particularly with respect to cardiac complications, that decision makers may find useful when weighing the benefits and harms of preventive measures.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data used for this study included proprietary health claims and clinical data. Further information concerning access to a limited dataset would be provided upon reasonable request to the corresponding author.
References
Centers for Disease Control and Prevention. Nationwide Commercial Lab Pediatric Antibody Prevalence. covid.cdc.gov/covid-data-tracker/#pediatric-seroprevalence.
Children and COVID-19: State-Level Data Report. American Academy of Pediatrics. aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-state-level-data-report/ (2022).
Centers for Disease Control and Prevention. Provisional COVID-19 Deaths: Focus on Ages 0-18. https://data.cdc.gov/NCHS/Provisional-COVID-19-Deaths-Focus-on-Ages-0-18-Yea/nr4s-juj3/data.
Bowe B., Xie Y. & Al-Aly Z. Acute and postacute sequelae associated with SARS-CoV-2 reinfection. Nature Medicine. 28, 2398–2405 (2022).
Children and COVID-19 Vaccination Trends. American Academy of Pediatrics. aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-vaccination-trends/ (2023).
Ashkenazi-Hoffnung, L. et al. Long COVID in children: observations from a designated pediatric clinic. Pediatr. Infect. Dis. J. 40, e509–e511 (2021).
Buonsenso, D. et al. Preliminary evidence on long COVID in children. Acta Paediatr. 110, 2208–2211 (2021).
Say, D. et al. Post-acute COVID-19 outcomes in children with mild and asymptomatic disease. Lancet Child Adolesc. Health 5, e22–e23 (2021).
Ludvigsson, J. F. Case report and systematic review suggest that children may experience similar long-term effects to adults after clinical COVID-19. Acta Paediatr. 110, 914–921 (2021).
Brackel, C. L. H. et al. Pediatric long-COVID: an overlooked phenomenon? Pediatr. Pulmonol. 56, 2495–2502 (2021).
Osmanov, I. M. et al. Risk factors for post-COVID-19 condition in previously hospitalised children using the ISARIC Global follow-up protocol: a prospective cohort study. Eur. Respir. J. 59, 2101341 (2022).
Molteni, E. et al. Illness duration and symptom profile in symptomatic UK school-aged children tested for SARS-CoV-2. Lancet Child Adolesc. Health 5, 708–718 (2021).
Stephenson, T. et al. Physical and mental health 3 months after SARS-CoV-2 infection (long COVID) among adolescents in England (CLoCk): a national matched cohort study. Lancet Child Adolesc. Health 6, 230–239 (2022).
Radtke, T., Ulyte, A., Puhan, M. A. & Kriemler, S. Long-term symptoms after SARS-CoV-2 infection in children and adolescents. JAMA 326, 869–871 (2021).
Borch, L., Holm, M., Knudsen, M., Ellermann-Eriksen, S. & Hagstroem, S. Long COVID symptoms and duration in SARS-CoV-2 positive children—a nationwide cohort study. Eur. J. Pediatr. 181, 1597–1607 (2022).
Kikkenborg Berg, S. et al. Long COVID symptoms in SARS-CoV-2-positive children aged 0-14 years and matched controls in Denmark (LongCOVIDKidsDK): a national, cross-sectional study. Lancet Child Adolesc. Health 6, 614–623 (2022).
Kompaniyets, L. et al. Post-COVID-19 symptoms and conditions among children and adolescents – United States, March 1, 2020-January 31, 2022. MMWR Morb. Mortal. Wkly. Rep. 71, 993–999 (2022).
Barrett, C. E. et al. Risk for newly diagnosed diabetes >30 days after SARS-CoV-2 infection among persons aged <18 years – United States, March 1, 2020-June 28, 2021. MMWR Morb. Mortal. Wkly. Rep. 71, 59–65 (2022).
Trapani, S. et al. Thromboembolic complications in children with COVID-19 and MIS-C: a narrative review. Front. Pediatr. 11, 944743 (2022).
Moore, B. J., White, S., Washington, R., Coenen, N. & Elixhauser, A. Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: The AHRQ Elixhauser Comorbidity Index. Med. Care 55, 968–705 (2017).
Oster, M. E. et al. Myocarditis cases reported after mRNA-based COVID-19 vaccination in the US from December 2020 to August 2021. JAMA 327, 331–340 (2022).
Patone, M. et al. Risk of myocarditis after sequential doses of COVID-19 vaccine and SARS-CoV-2 infection by age and sex. Circulation 146, 743–754 (2022).
Ali, M. M., Schreier, A., West, K. D. & Plourde E. Mental health conditions among children and adolescents with a COVID-19 diagnosis. Psychiatr. Serv. 73, 1412–1413 (2022).
Magnusson, K., et al. Healthcare use in 700 000 children and adolescents for six months after COVID-19: before and after register based cohort study. BMJ. 376, e066809 (2022).
Centers for Disease Control and Prevention. Underlying medical conditions associated with higher risk for severe COVID-19: information for healthcare professionals. https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-care/underlyingconditions.html#:~:text=Certain%20underlying%20medical%20conditions%20increased,the%20strongest%20association%20with%20death (2022).
Kompaniyets, L. et al. Underlying medical conditions associated with severe COVID-19 illness among children. JAMA Netw. Open 4, e2111182 (2021).
Maddux, A. B. et al. Health impairments in children and adolescents after hospitalization for acute COVID-19 or MIS-C. Pediatrics 150, e2022057798 (2022).
Kushner, L. E., Schroeder, A. R., Kim, J. & Mathew, R. “For COVID” or “With COVID”: classification of SARS-CoV-2 hospitalizations in children. Hosp. Pediatr. 11, e151–e156 (2021).
Acknowledgements
The authors would like to acknowledge Kerrin Gallagher for her assistance in variable creation.
Funding
The authors all are (or were at the time the study was conducted) employees of Elevance Health, Inc., or its subsidiary, Carelon Research. This study was conducted as part of employment duties and the authors did not receive additional funding for this research.
Author information
Authors and Affiliations
Contributions
A.S.G. designed the study and the analytic strategy. S. Shambhu and Y.X. obtained and analyzed the data. S. Shambhu and A.S.G. prepared the tables and figure. A.S.G., S. Shambhu, E.H., P.N.B., and S. Sloop interpreted the data. A.S.G. and Y.X. conducted the literature search. S. Shambhu and A.S.G. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. A.S.G. wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors all are (or were at the time the study was conducted) employees of Elevance Health, or its subsidiary, Carelon Research. As employees of Elevance Health, A.S.G., E.H. P.N.B., S. Shambhu, and S. Sloop hold Elevance Health stocks. E.H. is an advisor with stock options and a shareholder in Hello Pediatrics, a general pediatric telehealth company not specifically focused in COVID management.
Ethics approval
This observational study, conducted under the Research Exception provisions of Privacy Rule 45 CFR 164.514(e), was approved under Exempt Category by the WCB Institutional Board Review.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gordon, A.S., Shambhu, S., Xia, Y. et al. Clinical and healthcare utilization outcomes during the 6 months following COVID infection in children. Pediatr Res 95, 342–349 (2024). https://doi.org/10.1038/s41390-023-02762-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-023-02762-4