Abstract
Background
Sepsis related acute lung injury (ALI) is established in adults but has not been investigated in premature infants. Herein, we used pulmonary severity score (PSS) trajectories and C-reactive protein (CRP) to examine the relation between sepsis and ALI in premature infants.
Methods
This retrospective study identified 211 sepsis and 123 rule out (RO) events in 443 infants born <31 weeks and <1500 grams. The PSS was calculated prior to, at the time of, and up to 1 week after each event. Initial and peak CRP values were collected for each event.
Results
PSS significantly increased at 0 h from baseline (−72h) and remained increased at all subsequent time points (all p < 0.002) in sepsis events. Mean PSS in sepsis episodes were also higher compared to RO events at +24 h, +48 h, +72 h, and +168 h (all p < 0.004). A positive correlation was noted between peak CRP values in sepsis events and PSS at 0 h, +24 h, +48 h, and +72 h.
Conclusions
The temporal PSS trends and correlation with CRP levels observed in sepsis but not in RO events supports the hypothesis that neonatal sepsis is associated with ALI and contributes to the accumulating evidence that neonatal ARDS occurs.
Impact
-
To evaluate pulmonary severity scores and c-reactive protein values over time to establish an association between preterm neonatal sepsis and acute lung injury (ALI).
-
Though sepsis is well established as the most common indirect cause of ALI leading to acute respiratory distress syndrome (ARDS) in adults and pediatrics, this phenomenon remains undefined in neonates.
-
This study validates the proposal by the Neonatal ARDS Project that ARDS also occurs in neonates by demonstrating acute and sustained changes in markers of pulmonary injury temporally related to a diagnosis of neonatal sepsis in preterm infants.
Similar content being viewed by others
Introduction
Late onset sepsis (LOS) is a common complication of preterm birth, occurring in 15–30% of very low birth weight infants (VLBW)1,2. LOS confers significant morbidity including increased length of hospital stay, increased duration of mechanical ventilation, neurodevelopmental delay, and increased mortality3. Sepsis is also an independent risk factor for bronchopulmonary dysplasia (BPD), a debilitating chronic lung disease3,4,5,6,7. In the adult and pediatric populations, sepsis is the most common indirect cause of acute lung injury (ALI) and/or acute respiratory distress syndrome (ARDS)8,9,10. The diagnosis of ARDS confers a significant increase in morbidity and mortality10. Though, ALI/ARDS is well described in the adult and pediatric populations, this phenomenon remains undefined in neonates likely secondary to residual lung disease from conditions such as surfactant deficiency, meconium aspiration syndrome, and evolving BPD confounding the designation of a normal baseline. The first description of neonatal ARDS was by Faix et al. in 1989, who described ARDS in 11 term neonates11. Despite this early report, the current pediatric consensus definition of ARDS excludes neonatal patients specifically as a score obtained at a single point in time cannot account for the compounding effects of prematurity-related chronic lung disease on acute lung injury12.
In 2017 the Neonatal ARDS Project recognized that ARDS does occur in infants and attempted to produce a consensus definition for neonatal ARDS termed the Montreaux definition13. As the systemic inflammatory response generated by sepsis in adults and children is the key mediator for the development of ARDS, the group also suggested that classic neonatal inflammatory diseases such as necrotizing enterocolitis (NEC) may be unique triggers for the occurrence of ARDS in neonates13. In this study we specifically evaluated whether LOS and other systemic inflammatory diseases in premature neonates such as NEC are temporally correlated with a respiratory decompensation. We used the well-established pulmonary severity score (PSS) to serially quantify respiratory support and to serve as a surrogate for ALI14,15. As C-reactive protein (CRP) is often used as a biomarker for systemic inflammation, we also investigated the correlation between CRP and the rise in PSS. We hypothesized that sepsis and other diseases in preterm neonates associated with a systemic inflammatory response cause ALI and investigated this by analyzing temporal PSS and CRP trajectories.
Methods
Study design and data collection
This study was a retrospective study which included premature infants admitted to the neonatal intensive care unit (NICU) at Children’s Mercy Hospital Kansas City (CMKC) from 2010-2018. Inclusion criteria included infants born <31 weeks gestational age and <1500 grams. Infants were identified by searching the CMKC Children’s Hospital Neonatal Consortium database which tracks all admissions to the CMKC NICU. We also worked with the CMKC Medical Informatics team to identify patients in the electronic medical record who met the inclusion criteria in addition to receiving antibiotics for >6 consecutive days. Infants born with serious congenital anomalies or underlying genetic conditions were excluded. Additional exclusion criteria included: death prior to 72 h of life, transfer to CMKC after 1 week of life, and transfer to an outside facility prior to 36 weeks corrected gestational age. The study was approved by the institutional review board at CMKC.
Definition sepsis and systemic inflammatory diseases
Patient charts were reviewed in the electronic medical record for instances of antibiotic administration to treat LOS defined as sepsis which occurs >72 h after birth3. After review, 5 categories of antibiotic administration emerged: (1) Rule out (RO) events defined as episodes of suspected sepsis with discontinuation of antibiotics after 48–72 h of treatment when blood cultures remained negative and no other biochemical evidence of sepsis persisted. (2) Culture positive (CP) sepsis defined as at least 1 positive blood culture treated with >6 days of antibiotics. (3) Culture negative (CN) sepsis defined as clinical suspicion of sepsis treated with >6 days of antibiotics, but with a negative blood culture. In addition to be classified as CN sepsis, the event also had to meet 1 of the following 5 lab criteria: white blood cell count <5,000 or >20,000 (x103/mcl); immature to total neutrophil ratio ≥0.2; platelet count <100,000 (x103/mcl); or CRP > 20 mg/L (2.0 mg/dL)16,17. (4) Necrotizing enterocolitis-spontaneous intestinal perforation (NEC-SIP) defined as stage II or greater by the Bell classification and treated with >6 days of antibiotics18. (5) Urosepsis (UTI) defined as a positive urine culture treated with antibiotics >6 days, and the event had to meet 1 of the lab criteria used to define CN sepsis. We excluded diagnoses of pneumonia or tracheitis as these processes induce direct lung injury. We collected the initial and peak CRP levels during the sepsis and RO events as a marker for the severity of the systemic inflammatory response. In our unit, the collection of CRP values during a sepsis or RO event is clinician dependent. Therefore, CRP data was not available for all events. The data collected on RO events served as a control group for antibiotic use to distinguish PSS trajectories between true sepsis episodes and RO events not consistent with a sepsis diagnosis. Every sepsis and RO event identified was included for analysis. Therefore, multiple events were possible for each infant included in the study. To qualify as a distinct sepsis episode, the patient had to be off antibiotics or if on prolonged antibiotics have a positive culture with an organism not covered by the current antibiotic regimen.
Timeline for calculating pulmonary severity score trajectories
For each episode of LOS and RO identified, we obtained the PSS at −72, −48, and −24 h before, at the time of (0 h), and +24, +48, +72, and +168 hours after sepsis diagnosis. The PSS calculated prior to 0 h captured each infant’s baseline respiratory support needs. The magnitude of change from this baseline score surrounding a diagnosis of sepsis allowed us to capture the acute-on-chronic lung injury related to sepsis. No reliable method to determine the exact time of sepsis onset exists, as the time interval from the start of an infection to detection of vital and clinical signs of physiological compromise can be variable19. Therefore, we used time of first antibiotic administration to define time of sepsis diagnosis. Time of antibiotic administration usually occurs soon after sepsis is suspected, and it is also the time when treatment for sepsis begins.
The PSS is a validated scoring index that accounts for the level of respiratory support, fraction of inspired oxygen (FiO2), and respiratory medications to measure the overall severity of lung disease in neonates. The PSS was calculated as defined by Madan et al:14 (FiO2 x respiratory support) + (respiratory medications). FiO2 is the actual FiO2 if on positive pressure ventilation or the effective FiO2 if nasal cannula is used. Effective FiO2 was calculated using published tables which consider the infant’s weight, liter flow, and percent FiO220,21,22. The respiratory support score is 2.5 for ventilator or tracheostomy, 1.5 for nasal continuous positive airway pressure including high-flow nasal cannula (flow ≥ 2 L per minute), or 1.0 for nasal cannula flow or room air. The medication score is a sum of 0.2 for systemic steroids, 0.1 each for regular diuretics (daily or every other day) or inhaled steroids, and 0.05 each for methylxanthines or intermittent diuretics14. The PSS was collected at the same prespecified time intervals for RO events.
Statistical analysis
The primary outcome was to demonstrate an association between PSS trajectories over time and late-onset sepsis and systemic inflammatory diseases in preterm infants. A secondary analysis was performed to assess for an association between PSS and systemic inflammation as measured by the initial and peak CRP values. Other secondary outcomes included establishing a timeline regarding injurious effects of sepsis induced respiratory decompensation and determining sepsis subtypes associated with the greatest increases in PSS.
CRP and PSS were log-transformed (base 10) to approximate Gaussian distributions (log-PSS and log-CRP herein after); log-PSS was then multiplied by a factor of 10 for numerical stability in the subsequent modeling step. Due to the multi-level nature of our data in the hierarchical order of patients, sepsis episodes, and time (PSS only), both log-CRP and log-PSS were fitted by a linear mixed-effects model (LMM) to account for the within-patient and within-episode data dependency. For the primary outcome log-PSS, we fitted separate LMM with different fixed effects: (1) time with respect to antibiotics usage, episode diagnosis (sepsis, RO), and their interaction; (2) time with respect to antibiotic usage, sepsis subtypes, and their interaction; (3) time with respect to antibiotic usage, timing of CRP (initial, peak), and their interaction. All these LMM used random patient intercepts, random episode intercepts nested within patients, and the first-order autoregressive correlation structure. For the secondary outcome log-CRP, a LMM included CRP timing (initial, peak), episode type, and measure-by-type interaction as the fixed-effects, and random patient intercepts, random sepsis episode intercepts nested within patients. The parameters of LMM were estimated by the restricted maximum likelihood method. The post-hoc comparisons and correlations were estimated with p-values adjusted by the Tukey’s procedure for multiple comparisons, and their effect sizes were estimated by Cohen’s D (for changes and differences) or Pearson’s r (for correlations with CRP) converted from the t-statistic and degrees of freedom23. Cohen’s D 0.2-0.5, 0.5-0.8, >0.8 were considered as small, medium, and large effects respectively, and Pearson’s r 0.1-0.3, 0.3-0.5, >0.5 were considered as weak, moderate, and strong correlations respectively24. The analyses were conducted on R version 4.02. using the nlme package version 3.1-15325,26.
Results
Description of the study population
Among the 502 VLBW infants admitted during the study period, 59 (11.8%) were excluded for serious congenital anomalies or due to transfer from our unit, and 443 infants were eligible for analysis (Fig. 1). Of these eligible infants, 275 infants did not meet criteria for a sepsis diagnosis prior to 36 weeks corrected gestational age, and 168 infants had a least 1 episode of sepsis. RO events identified in both groups of infants were included for analysis. 122 infants had only sepsis events, 46 infants had both sepsis and RO events, 62 infants had only RO events, and 213 infants had neither. In total, 230 infants contributed to 334 total events, with 211 sepsis events and 123 RO events analyzed, providing 2588 PSS observations. Among the 211 sepsis episodes, CP, CN, NEC-SIP, and UTI accounted for 37.4%, 24.2%, 28.4%, and 10.0%, respectively (Fig. 1). The incidence of CP sepsis among all VLBW infants admitted to our NICU was 15.7% (79/502). Staphylococcus epidermidis comprised the most CP sepsis cases at 46.9% (46/79). Demographics of the entire population are outlined in Supplement Table 1. Mean gestational age was 26 1/7 weeks (SD ± 1.8) and mean birth weight 859 grams (SD ± 235). The population was comprised primarily of white (45%) and African American infants (39%). Males comprised 60% and females 40%.
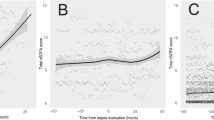
Association between sepsis events and PSS
For initial analysis, all sepsis subtypes were combined into one group. The LMM-derived mean PSS trajectories for sepsis and RO events are shown in Fig. 2a. In sepsis events, the PSS remained stable during the baseline time period of −72h to −24h. However, the PSS increased significantly from −72h to the time of sepsis diagnosis (0 h) (D = 0.35, p < 0.001) and remained significantly elevated from baseline at +24 h, +48 h, +72 h and +168 h after sepsis diagnosis (D ranged 0.17–0.32, p values < 0.001–0.002).
a Mean PSS trajectories between all sepsis events combined and all rule out events combined over time in hours. b Mean PSS trajectories between 1st episode of sepsis and 1st rule out event. * Indicates statistically significant difference between the PSS at −72h and subsequent time points. †Indicates statistically significant difference in PSS between sepsis and RO events. Abbreviations: ABXs, antibiotics; h, hours; PSS, pulmonary severity score; RO, rule out event.
PSS increased significantly from baseline (−72h) in RO events to the time of evaluation for sepsis (0 h) (D = 0.21, p < 0.001). However, the PSS did not remain significantly elevated at +24 h and subsequent time points unlike in sepsis events. PSS scores did not significantly differ between RO and sepsis events at the −72h, −48h, and −24h time points (D ranged 0.01–0.09). However, at all time points after sepsis diagnosis the mean PSS in sepsis was significantly elevated compared to RO events (D ranged 0.12–0.19, p values < 0.001–0.004). This shows that sepsis was associated with significant and persistent increases in PSS, but RO events were not. Untransformed raw PSS trajectories also showed the same trend with a sustained increase in PSS trajectories with sepsis events but not with RO events, and these trajectories are displayed in Supplement Fig. 1. Tables with mean PSS values are provided as Supplement Table 2A.
As sepsis and RO events overlapped amongst infants eligible for analysis, we performed PSS analysis on only the first episode of a sepsis or RO event to eliminate crossover between these patients and the potential compounding effect of lung injury from a prior sepsis or RO event (Fig. 2b). Despite the overlap of sepsis and RO events within infants, the change in mean PSS from baseline remained significantly elevated only in sepsis events (D ranged 0.15-0.35, p values < 0.001-0.02) but not in RO events. This further illustrates that persistent lung injury occurs in association with sepsis but not RO. Tables with mean PSS values are provided as Supplement Table 2B. Additional analysis provided in the supplement section shows that only sepsis was associated with sustained increases in PSS independent of if an infant had a previous sepsis or RO event (Supplement Fig. 2A–D, Supplement Tables A–D).
PSS trajectories by sepsis subtypes
To investigate the relation between ALI and different types of sepsis, we analyzed the PSS by the 4 sepsis subtypes defined above: CP, CN, NEC-SIP, and UTI (Fig. 3). All sepsis subtypes with the exception of UTI, followed a similar trajectory to the combined sepsis analysis with a significant increase in PSS from baseline to the time of sepsis diagnosis (0 hr) and to at least +48 hr after diagnosis. PSS scores in CP sepsis were significantly elevated from baseline (−72h) at 0 h, +24 h, +48 h, +72 h, and +168 h (D ranged 0.14–0.30, p values < 0.001–0.02). PSS scores in CP sepsis had the highest rise in magnitude compared to other sepsis subtypes and were also significantly increased compared to RO at all time points after sepsis diagnosis (+24 h, +48 h, +72 h, and +168 h, D ranged 0.14–0.18, p values < 0.001–0.01). A significant increase in PSS from baseline in the NEC-SIP events occurred at 0 h, +24 h, +48 h, and +72 h (D ranged 0.14–0.17, p values 0.001-0.009). PSS in infants with CN sepsis also showed a significant increase from baseline at 0 h, +24 h, and +48 h (D ranged 0.13–0.14, all p values 0.03). There was no significant change in PSS from baseline for UTI events or RO events, except for a significant increase at the 0 h time point in RO (D 0.21, p < 0.001). Tables with mean PSS values corresponding to each sepsis subtype in Fig. 3 are provided as Supplement Tables 3A and 3B.
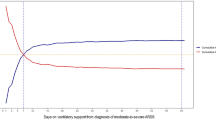
Association between Initial and Peak CRP values and Sepsis
CRP is a biomarker for systemic inflammation; therefore, we analyzed the initial and peak CRP values during a sepsis or RO event to estimate the correlation between severity of the systemic inflammatory response and the rise in the PSS. Figure 4a shows significantly higher initial [median and interquartile range 1.8 (0.7, 4.5) vs. 0.6 (0.5,1.1), p < 0.001] and peak values [3.6 (0.8, 8.7) vs. 0.8 (0.5, 1.4), p < 0.001] for sepsis events vs. RO events. As collection of CRP values during a sepsis or RO event is clinician dependent in our unit, this data was missing in 34 out of 334 (10.2%) total events analyzed.
a Scatter plot by initial and peak CRP in sepsis and rule out events. b CRP trajectory from initial to peak CRP. * Indicates statistically significant difference in magnitude of change from initial CRP to peak CRP in sepsis group vs RO group (p value 0.004). Data representative of 300 events (sepsis: 183; RO: 117). Abbreviations: CRP C-reactive protein; RO rule out event.
The associations between the PSS and initial and peak CRP values are shown in Fig. 5a, b (Supplement Tables 5A and 5B). The ß represents the slope coefficient at each time point. There was a statistically significant positive relationship between the initial CRP and PSS at +24 h (ß 0.07; 95% CI 0.02 to 0.12; p = 0.004), and this effect was considered moderate (Pearson’s r 0.45) following Cohen’s guideline. No significant relationship was observed between the initial CRP and other time points. There were statistically significant positive slopes between peak CRP and PSS at 0 h, +24 h, +48 h, and +72 h (0 hr ß 0.03; 95% CI 0.01 to 0.06; p = 0.02; +24 h 0.05; 95% CI 0.02 to 0.07; p = 0.002; +48 h 0.04; 95% CI 0.02 to 0.07; p = 0.003; +72 h 0.03; 95% CI 0.00 to 0.06, p = 0.03). These slopes corresponded to Pearson’s r range from 0.36 to 0.50.
a Associations between initial CRP and PSS. b Associations between peak CRP and PSS. All differences marked with an asterisk represent statistically significant difference in slope coefficients between CRP and PSS from baseline of −72h to other various time points. PSS is log transformed and multiplied by a factor of 10. Abbreviations: CRP, C-reactive protein; PSS, pulmonary severity score.
Discussion
Sepsis is a cause of ALI and ARDS in the adult and pediatric populations8,9,10. However, sepsis-related ALI is not clearly defined in neonates. In this study we found that sepsis and other systemic diseases associated with an inflammatory response were associated with elevated PSS trajectories in preterm infants. In contrast, RO events were not associated with sustained changes in PSS scores. This finding suggests that worsening lung disease is temporally associated with LOS and implies that ALI occurs during sepsis events. Furthermore, PSS trajectories correlated with peak CRP levels after sepsis diagnosis, suggesting that respiratory deterioration associated with sepsis parallels the systemic inflammatory response. These findings support both our hypothesis and that of the Neonatal ARDS Project that ARDS occurs in infants and that neonatal inflammatory diseases are triggers for its occurrence13.
Currently neonates are excluded from the pediatric classification for ARDS due to the inability to account for underlying chronic lung conditions with the current definition. We accounted for these underlying pulmonary conditions by obtaining a baseline PSS at −72h to −24h. The PSS is validated for use in those with chronic lung disease and is associated with severity of lung injury and subsequent pulmonary morbidity. Though the PSS is validated as a measure of severity of lung illness and respiratory needs in older infants with BPD, it has not been widely used in preterm infants nor has it been validated as a measure of ALI. However, by calculating the PSS prior to sepsis events, we captured baseline pulmonary illness and used the magnitude of change from this baseline in relation to sepsis diagnosis as a surrogate measure of ALI14,15. The inclusion of baseline respiratory severity allowed us to capture acute respiratory deterioration on top of existing chronic lung disease related to disorders of prematurity.
Many sepsis evaluations are prompted by an acute respiratory decompensation, which is consistent with our results that show a rise in PSS in RO events at the time of sepsis evaluation (0 h). However, the PSS in RO events quickly returned to baseline despite discontinuation of antibiotics, whereas they remained elevated from baseline in sepsis up to 1 week after a sepsis event. This trend with only a transient increase in PSS with RO events was independent of whether the episode was the first episode or a subsequent episode, unlike the sustained increase in PSS seen with sepsis events (Fig. 2b, Supplement Fig. 2A–D). This suggests that the elevated PSS in RO events were likely secondary to a transient cause other than sepsis-associated ALI. These results may prompt clinicians to consider early discontinuation of antibiotics after 48 h if cultures remain negative and respiratory status returns to baseline.
Our data also offers insight into the clinical course of ALI. Mean PSS did not increase from −72h to −24h prior to starting antibiotics. The time period between −24h to 0 h captured an increase in PSS coinciding with the commencement antibiotics for a sepsis diagnosis. However, this increase in PSS was only sustained in sepsis events and not RO events. This suggests that ALI has already occurred by the time sepsis is diagnosed. As there is no way to determine the exact time of sepsis onset, we used time of first antibiotic administration to define the onset of sepsis (0 h). It is possible that there may have been variations in the duration of time between when sepsis was suspected, when laboratory values and blood cultures were obtained, and the time of first antibiotic administration that may have impacted the PSS trajectory timeline. However, the resulting timeline is consistent with the time needed to mount a significant inflammatory response that can be detected clinically, and with other studies that show vital sign changes occur well before sepsis is diagnosed19,27,28. Our timeline also suggests that significant lung injury persists up to 1 week after diagnosis, which is consistent with the clinical course of ARDS described in older populations10,29.
As anticipated when analyzed by category of sepsis event, we found that CP sepsis and NEC-SIP events were associated with elevated PSS trajectories. PSS scores in CP sepsis showed a significant elevation from baseline and remained significantly elevated when compared to RO events at all time points. NEC-SIP events had the lowest mean PSS of any subtype during the baseline time period and showed significant elevation from this baseline after the event occurred implying a significant degree of ALI. However, the PSS in NEC-SIP were significantly elevated compared to those in RO only at the +72 h time point. We speculate this was due to the inclusion of stage II NEC, which may not generate a large inflammatory response like stage III NEC and SIP.
CN sepsis was also associated with elevated PSS trajectories. This is an important group to include as the definition of neonatal sepsis remains broad and ill-defined. Clinicians continue to treat infants for clinical infection despite negative blood cultures based off subjective signs that vary from clinician to clinician. A deterioration in respiratory status is one sign that commonly prompts concern for CN sepsis. Studies show that clinical or CN sepsis is associated with increased morbidity including BPD indicating that some degree of systemic inflammatory response occurs30. Furthermore, recent randomized clinical trials testing novel therapeutic treatments include neonates with both confirmed and clinically suspected or CN sepsis31,32,33. Unfortunately, we are unable to differentiate between CN sepsis events representing true sepsis episodes versus RO events treated with prolonged antibiotics. We anticipate the mean PSS scores in the CN group would be higher if this distinction was possible. The UTI subtype did not show elevated PSS from baseline likely due to the localized nature infection. However, this category is important because the goal was to not only look at CP sepsis, but also to examine the effects on PSS due to other infectious or neonatal causes of systemic inflammation. For some of these phenotypes, a small N precluded further analysis.
Previous work in neonatal animal models and adults show ARDS results in increased vascular permeability, neutrophil influx, cytokine expression, and lung matrix destruction10,34,35. Due to the retrospective nature of our study and the fact that not all neonates included in our analysis were intubated, sepsis episodes included in our study lack corroborative evidence of ALI as measured by lung cytokine expression and known cellular changes. However, as CRP is an established marker of the systemic inflammatory response, our CRP data serves as a biomarker of the presence and severity of this systemic response during sepsis episodes and correlates well with increased PSS trajectories. Both initial and peak CRP levels were higher in sepsis events than in RO events. Most importantly, while initial CRP values measured correlated with the PSS + 24 h after sepsis diagnosis, the peak CRP correlated with the PSS at 0 h, +24 h, +48 h, and +72 h. These findings further support published data that suggests serial CRP measurements may be helpful in determining true sepsis events17,36,37,38.
Although this is one of the first studies to report the association between sepsis and increased PSS as an indicator of ALI, the retrospective nature of the study limits a deterministic interpretation. The proposed Montreaux definition of neonatal ARDS requires invasive arterial blood gas measurements or transcutaneous oxygen values which were unavailable in all patients retrospectively and specific chest x-ray findings, which can be difficult to interpret in preterm infants with underlying lung disease. We considered measuring the respiratory severity score (RSS) which is a product of mean airway pressure (MAP) and FiO2. However, we included non-intubated infants on non-invasive support, in which it is difficult to accurately measure the MAP a patient receives. Furthermore, our aim was to capture a worsening in respiratory support, and the RSS does not capture escalation from noninvasive support to invasive mechanical ventilation.
Conclusion
In conclusion, we found that PSS scores were temporally associated with sepsis episodes but not rule out events, implying ALI. This study supports our hypothesis and that of the Neonatal ARDS network that ARDS secondary to sepsis and other neonatal inflammatory diseases occurs in premature infants. Increased recognition of sepsis-induced ALI in neonates will promote future investigation into the factors that program the severity of ALI and its consequences such as BPD and brain injury. Defining ALI in neonates including the timeline for the clinical course of ARDS, provides insight into the therapeutic window for implementation of therapies that could improve outcomes for premature infants.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stoll, B. J. et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA 314, 1039–1051 (2015).
Letouzey, M. et al. Cause of preterm birth and late-onset sepsis in very preterm infants: the EPIPAGE-2 cohort study. Pediatr. Res 90, 584–592 (2021).
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD neonatal research network. Pediatrics 110, 285–291 (2002).
Rojas, M. A. et al. Changing trends in the epidemiology and pathogenesis of neonatal chronic lung disease. J. Pediatr. 126, 605–610 (1995).
Lahra, M. M., Beeby, P. J. & Jeffery, H. E. Intrauterine inflammation, neonatal sepsis, and chronic lung disease: a 13-year hospital cohort study. Pediatrics 123, 1314–1319 (2009).
Ohlin, A., Björkman, L., Serenius, F., Schollin, J. & Källén, K. Sepsis as a risk factor for neonatal morbidity in extremely preterm infants. Acta Paediatr. 104, 1070–1076 (2015).
Shah, J., Jefferies, A. L., Yoon, E. W., Lee, S. K. & Shah, P. S., Canadian Neonatal Network. Risk factors and outcomes of late-onset bacterial sepsis in preterm neonates born at <32 weeks’ gestation. Am. J. Perinatol. 32, 675–682 (2015).
Monahan, L. J. Acute respiratory distress syndrome. Curr. Probl. Pediatr. Adolesc. Health Care 43, 278–284 (2013).
Meyer, N. J., Gattinoni, L. & Calfee, C. S. Acute respiratory distress syndrome. Lancet 398, 622–637 (2021).
Matthay, M. A. et al. Acute respiratory distress syndrome. Nat. Rev. Dis. Prim. 5, 1–18 (2019).
Faix, R. G., Viscardi, R. M., DiPietro, M. A. & Nicks, J. J. Adult respiratory distress syndrome in full-term newborns. Pediatrics 83, 971–976, https://www.ncbi.nlm.nih.gov/pubmed/2657626 (1989).
Group TPALICC. Pediatric acute respiratory distress syndrome: consensus recommendations from the pediatric acute lung injury consensus conference. Pediatr. Crit. Care Med. 16, 428–439 (2015).
De Luca, D. et al. The Montreux definition of neonatal ARDS: biological and clinical background behind the description of a new entity. Lancet Respir. Med 5, 657–666 (2017).
Madan, A. et al. A pulmonary score for assessing the severity of neonatal chronic lung disease. Pediatrics 115, e450–e457 (2005).
Linafelter, A. et al. Extended course of prednisolone in infants with severe bronchopulmonary dysplasia. Early Hum. Dev. 136, 1–6 (2019).
Hornik, C. P. et al. Use of the complete blood cell count in late-onset neonatal sepsis. Pediatr. Infect. Dis. J. 31, 803–807 (2012).
Aydemir, C., Aydemir, H., Kokturk, F., Kulah, C. & Mungan, A. G. The cut-off levels of procalcitonin and C-reactive protein and the kinetics of mean platelet volume in preterm neonates with sepsis. BMC Pediatr. 18, 253 (2018).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Kumar, N., Akangire, G., Sullivan, B., Fairchild, K. & Sampath, V. Continuous vital sign analysis for predicting and preventing neonatal diseases in the twenty-first century: big data to the forefront. Pediatr. Res 87, 210–220 (2020).
Benaron, D. A. & Benitz, W. E. Maximizing the stability of oxygen delivered via nasal cannula. Arch. Pediatr. Adolesc. Med 148, 294–300 (1994).
STOP-ROP Multicenter Study Group. Supplemental therapeutic oxygen for prethreshold retinopathy of prematurity (STOP-ROP), a randomized, controlled trial. I: primary outcomes. Pediatrics 105, 295–310 (2000).
Walsh, M. et al. Oxygen delivery through nasal cannulae to preterm infants: can practice be improved. Pediatrics 116, 857–861 (2005).
Lüdecke, D., Waggoner, P. & Makowski, D. Insight: a unified interface to access information from model objects in R. J. Open Source Softw. 4, 1412 (2019).
Cohen, J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. (Academic Press, New York 1988).
Pinheiro, J., Bates, D., DebRoy, S., Sarkar, D., R Core Team. nlme: Linear and Nonlinear Mixed Effects Models. R package version 3.1-152. September 2021. https://cran.r-project.org/package=nlme.
R Core Team. R: A language and environment for statistical computing. (R Foundation for Statistical Computing, Vienna, Austria, 2020). https://www.r-project.org/.
Fairchild, K. D. & O’Shea, T. M. Heart rate characteristics: physiomarkers for detection of late-onset neonatal sepsis. Clin. Perinatol. 37, 581–598 (2010).
Sullivan, B. A. & Fairchild, K. D. Predictive monitoring for sepsis and necrotizing enterocolitis to prevent shock. Semin Fetal Neonatal Med 20, 255–261 (2015).
Keim, G., Watson, R. S., Thomas, N. J. & Yehya, N. New morbidity and discharge disposition of pediatric acute respiratory distress syndrome survivors. Crit. Care Med 46, 1731–1738 (2018).
Stoll, B. J. et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 292, 2357–2365 (2004).
Hayes, R. et al. Neonatal sepsis definitions from randomised clinical trials. Pediatr Res. (2021). Online ahead of print. https://doi.org/10.1038/s41390-021-01749-3
INIS Collaborative Group. et al. Treatment of neonatal sepsis with intravenous immune globulin. N. Engl. J. Med 365, 1201–1211 (2011).
ELFIN trial investigators group. Enteral lactoferrin supplementation for very preterm infants: a randomised placebo-controlled trial. Lancet 393, 423–433 (2019).
Menden, H. L. et al. Nicotinamide adenine dinucleotide phosphate oxidase 2 regulates LPS-induced inflammation and alveolar remodeling in the developing lung. Am. J. Respir. Cell Mol. Biol. 55, 767–778 (2016).
Salimi, U., Dummula, K., Tucker, M. H. & Dela Cruz, C. S. Sampath, V. postnatal sepsis and bronchopulmonary dysplasia in premature infants: mechanistic insights into “New BPD. Am. J. Respir. Cell Mol. Biol. 66, 137–145 (2022).
Kawamura, M. & Nishida, H. The usefulness of serial C-reactive protein measurement in managing neonatal infection. Acta Paediatr. 84, 10–13 (1995).
Benitz, W. E., Han, M. Y., Madan, A. & Ramachandra, P. Serial serum C-reactive protein levels in the diagnosis of neonatal infection. Pediatrics 102, E41 (1998).
Pourcyrous, M., Bada, H. S., Korones, S. B., Baselski, V. & Wong, S. P. Significance of serial C-reactive protein responses in neonatal infection and other disorders. Pediatrics 92, 431–435, https://www.ncbi.nlm.nih.gov/pubmed/8361798 (1993).
Author information
Authors and Affiliations
Contributions
M.H.T. conceptualized and designed the study, designed the data collection instruments, collected data, drafted the initial manuscript, and reviewed and revised the manuscript. H.W.Y. carried out data analyses and reviewed and revised the manuscript. D.O. collected data and reviewed and revised the manuscript. N.S. collected data and reviewed and revised the manuscript. N.K. conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. V.S. conceptualized and designed the study, coordinated and supervised data collection, and critically reviewed the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tucker, M.H., Yeh, HW., Oh, D. et al. Preterm sepsis is associated with acute lung injury as measured by pulmonary severity score. Pediatr Res 93, 1050–1056 (2023). https://doi.org/10.1038/s41390-022-02218-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41390-022-02218-1