Abstract
This narrative review focuses on the clinical use and relevance of cerebral oxygenation measured by NIRS during fetal to neonatal transition. Cerebral NIRS(cNIRS) offers the possibility of non-invasive, continuous, and objective brain monitoring in addition to the recommended routine monitoring. During the last decade, with growing interest in early and sensitive brain monitoring, many research groups worldwide have been working with cNIRS and verified the feasibility of cNIRS monitoring immediately after birth. Cerebral hypoxia during fetal to neonatal transition, defined as cerebral oxygenation values below10th percentile, seems to have an impact on neurological outcomes. Feasibility to guide clinical support using cNIRS to reduce the burden of cerebral hypoxia has been shown. It is well known that in some cases cerebral oxygenation follows different patterns than SpO2. Cerebral oxygenation does not only depend on systemic oxygenation, hemoglobin content and cerebral blood flow, but also on cardiocirculatory condition, ventilation, and metabolic parameters. Hence, measurement of cerebral oxygenation may uncover problems not detectable by standard monitoring. Therefore, applying NIRS can provide caregivers a more complete clinical overview, especially in critically ill neonates. In this review, we aim to describe the additional information which can be provided by cNIRS during fetal to neonatal transition.
Impact
-
This narrative review focuses on the clinical use and relevance of cerebral oxygenation measured by near infrared spectroscopy (NIRS) during fetal to neonatal transition.
-
During the last decade, interest on brain monitoring is growing continuously as the measurement of cerebral oxygenation may uncover problems which are not detectable by routine monitoring.
-
Therefore, it will be crucial to have additional information to get a complete overview, especially in critically ill neonates in need of medical and respiratory support.
-
In this review, we offer additional information which can be provided by cerebral NIRS during fetal to neonatal transition.
Similar content being viewed by others
Introduction
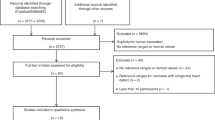
Fetal to neonatal transition is a susceptible period that includes complex physiological processes affecting all vital organ systems1. To objectify the neonate’s condition during this period, Virginia Apgar in 1953 established a scoring system2, which considers heart rate (HR), respiratory effort, reflex irritability, muscle tone and skin color. The Apgar score is based on visual inspection, palpation or auscultation and is routinely used worldwide due to its simple and quick assessment3. However, there is a significant inter-observer and intra-observer variability4,5, which leads us to the following question: which objective monitoring system is adequate to recognise perturbations in neonates in need of support during immediate neonatal transition after birth? According to the latest resuscitation guidelines6, non-invasive monitoring of arterial oxygen saturation (SpO2) and HR by pulse oximetry or electrocardiogram is recommended in neonates during stabilization immediately after birth. However, this approach does not provide information about oxygen transport to tissues, especially to the brain which is the most vulnerable organ to hypo- and hyperoxia during fetal to neonatal transition. The interest to monitor the brain properly7 has grown steadily during the last decade, as disturbances affecting this exposed organ may lead to short- and long-term sequelae. Cerebral near infrared spectroscopy (cNIRS) is a non-invasive objective method, which offers the continuous monitoring of cerebral tissue oxygen saturation (crSO2) and cerebral perfusion8. Since the exact technical aspects of NIRS and the differences between several devices are beyond the scope of this paper, we refer to other already published papers describing this topic in detail9,10,11. Many study groups have already performed research with cNIRS and have clearly demonstrated the feasibility of applying cNIRS during fetal to neonatal transition in term and preterm neonates, with and without respiratory and/or medical support12,13,14,15,16,17,18. Furthermore, normative values for crSO2 have been established for different devices19,20.
In this narrative review article, we provide an overview of literature (Table 1) with a focus on emphasizing clinical values using cNIRS during fetal to neonatal transition where we explore what additional information may be provided by cNIRS.
cNIRS during fetal to neonatal transition
Oxygenation
Oxygenation in neonates in the delivery room is a hot topic and has already been the focus of numerous study groups worldwide. However, several questions remain unclear.
First, the use of supplemental oxygen during neonatal stabilization. It is unknown which oxygen concentration is appropriate for preterm infants during fetal to neonatal transition21. The recommended monitoring of SpO2 during the transitional period does not provide any information about oxygen transport to brain, an organ that is extremely vulnerable to hypo- and hyperoxia. Looking at the normative values of SpO222 and crSO219,20 in term and healthy neonates during neonatal stabilization, we can observe a significant increase of both parameters during the first 6–7 min, with crSO2 reaching a constant plateau phase for the rest of the observational period and SpO2 continuing to increase. Using cNIRS, Baik et al. could observe that preterm infants who develop brain injury after birth had significantly lower crSO2 values during neonatal stabilization compared with preterm neonates without brain injury23. These differences in crSO2 occurred even when the SpO2 values were within the normal range showing no differences between the groups. The study group from Ulm, Germany, described a similar phenomenon in 2012 in two preterm infants24. In preterm neonates who developed brain injury, the SpO2 and crSO2 values took different courses already during first minutes after birth, showing lower values of crSO2 with SpO2 values in normal range, suggesting the presence of cerebral hypoxia. This led to the assumption that additional monitoring of the brain using cNIRS provides valuable, supplementary information to identify these differences. These neonates seem to suffer from different underlying pathology.
Secondly, targeting of SpO2 values. Oei et al. recently described increased risk of mortality and severe intraventricular hemorrhage (IVH) in neonates who did not reach a SpO2 target >80% at 5 min after birth25. Based on this information Binder-Heschl et al. published additional information about cerebral oxygenation in neonates not reaching a SpO2 target ≥80% at minute 5. These neonates showed significantly lower crSO2 over the whole study period. Interestingly, even in neonates reaching the SpO2 target of ≥80% at 5 min still 20% of them showed a crSO2 below the 10th percentile26.
Thirdly, Pichler et al. launched a randomized controlled pilot feasibility study, to assess monitoring of crSO2 to guide respiratory and supplemental oxygen support27. They explored if additional monitoring of crSO2 during resuscitation after birth could help to reduce the burden of cerebral hypoxia in preterm neonates of gestation <34 weeks. In the NIRS-visible group, crSO2 monitoring in addition to pulse oximetry was used to guide respiratory and supplemental oxygen support, whereas in the control group only pulse oximetry was used. In the NIRS-visible group cerebral hypoxia was halved [55.4% (95% CI 37.6–73.2%; P = 0.028)]27.
Additional Information provided by NIRS:
-
There are normative data available for several devices of cNIRS during fetal to neonatal transition. This enables the physician or researcher to identify possible pathological values of crSO2.
-
Low crSO2 values – below the 10th percentile –were associated with brain injury in preterm neonates.
-
If preterm infants obtained SpO2 ≥ 80% at minute 5 after birth, 80% of these displayed crSO2 values within normal ranges. Nevertheless, still 20% will display cerebral oxygen saturation below the 10th percentile for crSO2. As low crSO2 values are associated with brain injury, those 20% might benefit from additional cNIRS monitoring.
-
A randomized trial in preterm infants showed that a reduction of burden of cerebral hypoxia during immediate postnatal stabilization was feasible by crSO2 monitoring to guide respiratory and supplemental oxygen support.
The findings of the above-mentioned studies underscore that using SpO2 monitoring alone may miss valuable information especially related with the brain during fetal to neonatal transition.
Circulatory parameters
Heart rate
According to resuscitation guidelines6, circulatory, respiratory, and medical support is advocated in presence of bradycardia and/or hypoxia in newborns not reaching the recommended SpO2 goals. In the Bradyprem-study, it has been shown that prolonged bradycardia over 2 min during the first 10 min after birth is associated with increased mortality and cerebral hemorrhage28. Does the presence of bradycardia during the neonatal transition have an impact on cerebral oxygenation? Bresesti et al. analysed the vital parameters in 150 preterm neonates during the first 15 min after birth. The neonates were divided into different groups according to duration of bradycardia (no bradycardia, brief bradycardia <2 min, prolonged bradycardia >2 min) and to SpO2 values at 5 min of life (<80% or >80%). They observed that presence of bradycardia alone did not influence the courses of crSO2. However, the degree of bradycardia had a significant impact on the course of SpO2. Only if the bradycardia was associated with presence of hypoxemia, a significant impact on cerebral oxygenation was observed29. These findings emphasize that bradycardia was only detrimental for cerebral oxygenation if combined with hypoxemia. If no hypoxemia was associated, bradycardia alone had no impact on crSO2 in late preterm infants.
Cerebral blood volume (CBV)
Another approach to interpret cNIRS during fetal to neonatal transition is to look at the cerebral blood volume (CBV). With some NIRS devices, it is possible to measure changes in total hemoglobin (ΔHbT) values. In one study, ΔHbT values for each minute were calculated by subtracting the mean HbT value at 15 min after birth from the mean HbT value of each minute30. The 15-minute value was used as reference value, because at that time point NIRS signal quality was most stable and reliable. In this study a significant decrease of HbT within the first 15 min after birth was demonstrated in healthy term infants. Next, ΔHbT values were converted to ΔCBV by the following equation, whereby Hb represents the hemoglobin concentration (g/dl)31.
They estimated a decrease of CBV of 1.0 ml/100 g brain from 2 min to 15 min after birth. In another study, Schwaberger et al. investigated 204 neonates with and without respiratory support (RS) and studied differences in CBV changes. In the total study population, they could describe a significant decrease in CBV within the first 15 min after birth with a trend toward smaller ΔCBV in neonates with RS compared to neonates without RS. If the changes concerning CBV in healthy neonates without respiratory support reflect physiological fetal to neonatal transition, the smaller change of ΔCBV in neonates in need of respiratory support might be a sign of cerebral vasoconstriction depending on pO2 levels, likely to be lower in neonates needing respiratory support and/or supplemental oxygen32.
Noori et al. observed similar results in 20 neonates immediately after birth. They described a rising tendency of SpO2 and crSO2 and reduction in cerebral blood flow (CBF) due to an increase in arterial pO2 content, persistent ductus arteriosus (PDA) shunting or both33.
Concerning different respiratory support techniques, Fuchs et al. applied in 24 preterm neonates sustained lung inflations (SLI) after birth for lung recruitment. They used three SLI approaches of 20, 25, 30 cm H2O of 15 s duration, each followed by nasal continuous positive airway pressure (nCPAP). They could observe a rapid increase of heart rate and cerebral tissue oxygen saturation. However, SpO2 increase was slightly delayed as compared to HR and crSO2. It was concluded that effective SLI increased HR and crSO2 earlier than SpO234.
Schwaberger et al. calculated CBV in 40 preterm neonates receiving either up to three SLI (30 cmH2O for 15 s) or standard respiratory support (CPAP with 5 cm H2O positive end-expiratory pressure (PEEP) and if needed positive pressure ventilation at 30 cm H2O PIP via face mask) and compared these two groups. In the standard care group CBV was significantly decreased, whereas the SLI group showed similar CBV values during the whole period of 15 min without decreasing tendency. Based on this observation, they hypothesized that the RS itself might influence postnatal CBV changes, most probably by increasing the intrathoracic pressure leading to cerebral venous stasis and an impairment of venous return to the heart35.
Chest compression
The need for chest compressions during fetal to neonatal transition is rare. Li et al. published a case report of an extremely preterm neonate (24 weeks, 650 g) with prolonged bradycardia after birth. This neonate was treated with ventilation and chest compression for 90 s until return of spontaneous circulation (ROSC). During resuscitation the neonate was monitored with ECG, SpO2, respiratory function monitor and cNIRS. They could observe a delayed increase in cerebral oxygenation, approximately 120 s after the rapid increase in HR, despite normal oxygen saturation when reaching ROSC. This observation highlights that cerebral oxygenation depends on several factors apart from SpO2. Likely, post resuscitation low cardiac output may have caused the delay in increase in cerebral oxygenation36.
Furthermore, in an experimental study in near-term sheep foetuses, it was found, that ROSC from perinatal asphyxia was characterised by excess oxygen delivery that was driven by rapid increases in cerebrovascular pressure, flow, and oxygen saturation, and may be monitored non-invasively with NIRS37. Thus, further work to describe and limit injury mediated by oxygen toxicity following ROSC is warranted.
Hemodynamics
As described above, crSO2 depends not only on the arterial oxygen content, but also on hemodynamic parameters. The presence of shunt volumes during fetal to neonatal transition is a well-known fact. Urlesberger et al., observed in 72% of 80 neonates born at term the presence of a left to right (LR) shunt via ductus arteriosus (DA). The rest of the observed population didn’t show any shunt flow via DA. They compared these two groups and found that the shunt group showed significantly higher values of cerebral oxygenation and heart rates compared to the non-shunt group. In term neonates, where there is no flow via the DA, there might be reduced left ventricular output leading to impairment of carotid blood flow and resulting in lower crSO2 values38.
The shunting does not only exist through DA, but also through Foramen ovale (FO). Baik et al. investigated the potential influence on cerebral oxygenation in 60 term neonates who had a LR shunt via both, DA and FO. They could describe that the increasing sum of DA and FO diameters were correlated negatively with cerebral oxygenation. This finding suggests that considering DA alone might not be sufficient to obtain the whole picture regarding the influence of LR shunting especially on cerebral oxygenation. Taken together, when the LR flow via DA and FO are present, the positive effect of LR shunting via DA might be reduced again by possible steal phenomenon of combined LR shunting via FO and DA39.
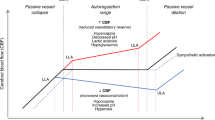
Another important hemodynamical parameter is blood pressure, which can be readily obtained during newborn resuscitation. In an observational study, a total of 462 preterm and term neonates were investigated. A significant negative correlation has been observed between mean arterial blood pressure (MABP) and cerebral fractional tissue oxygenation extraction (cFTOE) in preterm infants but not in term infants40. cFTOE can be calculated from SpO2 and crSO2 with following equation: cFTOE = (SpO2 – crSO2)/ SpO241, and represents the relation between oxygen delivery and oxygen consumption. Turning back to the former described study40, MABP had an impact on cerebral oxygenation primarily in preterm infants. Therefore, blood pressure monitoring during the immediate neonatal transition might be relevant for improving cerebral oxygenation, especially in preterm infants40. Several studies have already described that cerebral oxygenation is dependent on especially in critically ill preterm infants due to possibly impaired cerebral autoregulation42,43. Cerebral autoregulation is a complex and multifactorial process and it is unclear, whether there is a developmental aspect during the first min of life. The observational studies, however, point out the possibility, that cerebral autoregulation might be impaired in preterm infants during fetal to neonatal transition and therefore low blood pressure might be more detrimental to cerebral perfusion and finally oxygenation.
Another relevant hemodynamical parameter during neonatal transition is cardiac output (CO). Baik-Schneditz et al. showed in 99 term healthy neonates a decreasing tendency of cardiac output until 10 min after birth. Furthermore, there was no significant correlation between CO and crSO2. Contrary to the hypothesis that higher CO would result in higher cerebral oxygenation as oxygen delivery is dependent on CO and oxygen content, they could not observe any significant correlation between CO and cerebral oxygenation. Nonetheless, this finding may be a sign of intact cerebral autoregulation in term neonates44. In 60 cardio-circulatory stable neonates Bruckner et al. could observe, that there is no correlation between crSO2 and parameters of cardiac function in the first day after birth45.
According to the studies, crSO2 seems to be influenced by the presence of LR shunts. Moreover, hemodynamic parameters seem to have no impact on crSO2, especially in cardio-circulatory stable neonates as a sign of intact cerebral autoregulation.
Additional information provided by NIRS:
-
During fetal to neonatal transition, bradycardia was only harmful for cerebral oxygen saturation if combined with hypoxia.
-
The steep postnatal increase in PaO2 results in cerebral vasoconstriction and leads to a significant fall of CBV, which is a physiological response.
-
Increasing intrathoracic pressure, e.g. using SLI, results in less reduction of CBV.
-
The presence of LR shunt via ductus arteriosus leads to higher crSO2 values. This fact confirms animal data about the importance of ductal shunting in providing substitute for loss of preload immediately after cord clamping.
-
The sum of DA and FO diameters is correlated negatively with cerebral oxygenation. If shunt volume is (too) big, crSO2 may be influenced negatively.
-
Cardiac output alone is not significantly correlated to crSO2.
-
A significant negative correlation is observed between MABP and cFTOE in preterm neonates, but this phenomenon is not replicable in term neonates indicating maturation of cerebral autoregulation.
Metabolic parameters
Cerebral activity
Maintaining cerebral metabolic function during transition might be the ultimate objective of resuscitation efforts and is crucial for short- and long-term neurological outcomes. Tamussino et al. could observe that low levels of crSO2 were accompanied by low levels of cerebral activity despite normal levels of SpO246. The data of 59 term neonates were analysed in the study. In addition to routine monitoring with pulse oximetry, amplitude integrated electroencephalography (aEEG) and cNIRS measurements were performed during the first 15 min after birth. Neonates with initial low cerebral activity using aEEG monitoring, which normalized during transition, were compared to neonates with normal aEEG values throughout the whole monitoring period. The low-cerebral activity group showed lower levels of crSO2 despite the normal levels of SpO2 and interestingly, this group showed increased cFTOE. This phenomenon can be explained by primarily low oxygen delivery with depletion of oxygen to maintain the low activity46.
Blood glucose
To assess a possible association of blood glucose concentration with cerebral oxygenation in preterm and term neonates, Mattersberger et al. analysed data of 75 neonates (50 term and 25 preterm). crSO2 was inversely correlated with blood glucose concentrations. Higher blood glucose concentrations were associated with lower crSO2 in preterm and term neonates. Low blood glucose concentrations were shown to cause cerebral vasodilatation, and this resulted in increased cerebral blood flow and oxygen supply. This might explain the higher crSO2 in neonates with low blood glucose levels. These findings suggest that immediately after birth, cerebral blood vessels in neonates are reactive to blood glucose concentrations47.
Body temperature
Body temperature (BT) management remains a challenge in neonatal intensive care, especially during resuscitation after birth. To analyse, whether there is an association between the BT and crSO2, SpO2 and heart rate, Bruckner et al. investigated 169 preterm and 417 term neonates. BT was lower in preterm compared to term neonates and the prevalence of hypothermia was higher in preterm neonates. BT did not correlate with SpO2 and crSO2, however there was a weak positive correlation between the BT and HR in the whole cohort. The absent association between BT and cerebral oxygenation may be explained by the neonatal brain autoregulation ability to overcome the only mild deviation of body temperature in the cohort or by a possibly decreased oxygen consumption in association with lower temperature48.
Additional information provided by NIRS:
-
Low crSO2 values are associated with low levels of cerebral electrophysiological activity measured with aEEG. In that phase cFTOE is increased, representing an increase in cerebral oxygen extraction.
-
Immediately after birth, cerebral blood vessels are reactive to blood glucose concentrations. An increase in blood glucose levels is associated with a decrease in crSO2 values, indicating a vasoconstrictive reaction of cerebral blood vessels, resulting in lower oxygen delivery to the brain.
-
Mild changes in body temperature do not correlate with changes in crSO2.
Particular circumstances
Intrauterine growth restriction (IUGR)
IUGR is associated with adverse perinatal outcomes49. Research interest concerning IUGR is growing in neonatology. Baik-Schneditz et al. investigated evolving crSO2 in IUGR neonates matched for gestational age and sex with neonates appropriate for gestational age (AGA). Forty-five IUGR neonates and 135 AGA neonates were compared. There was a significant difference in crSO2 beginning at 5 min and continuing for the rest of the observational period of 15 min with higher crSO2 values in the IUGR group compared to AGA group. Contrarily, there were no differences regarding SpO2 and HR, between groups50. IUGR is the result of an insufficient uteroplacental perfusion. Hence, the fetus is alternatively exposed to phases of both acute and chronic hypoxia. The fetus redistributes cardiac output (“brain sparing”) to optimize oxygen and nutrient supply to the brain using a combination of cerebral vasodilatation and increasing peripheral vascular resistance51. This suggests that the significantly higher crSO2 values are due to a combination of both an increase in cerebral oxygen delivery, i.e increased hemoglobin concentration and increased cardiac output, and a decrease in cerebral oxygen extraction due to a pronounced reduction of cFTOE.
Delayed cord clamping
Delayed cord clamping (DCC) has become a hot topic in neonatology. It has been shown that DCC for 5 min improves cardiac output in term, healthy, vaginally delivered infants52. Additionally, another study observed 282 term healthy newborn infants after vaginal delivery who underwent DCC > 60 s following phenomenon. These term neonates achieved higher SpO2 and HR values in the first 5 min after birth compared with term neonates with immediate cord clamping53.
Infants at risk for resuscitation may benefit from extended placental transfusion by increased blood volume. Katheria et al., conducted a randomized controlled trial of vaginally delivered term neonates who required the attendance of a neonatal provider because of an at-risk delivery. At delivery, the attending team randomised each neonate to receive 1 minute or 5 min of DCC. Sixty term neonates were included into this study. There were no differences between groups in HR or SpO2. Furthermore, there were no differences concerning postnatal non-invasive measured hemoglobin or bilirubin. However, neonates in the 5 min DCC group had higher mean blood pressure (BP), crSO2 and lower cFTOE at 12 h of life compared with the 1-minute group54.
Another study group investigated the DCC in 39 preterm neonates. They compared newly borns with DCC of 60–90 s to a control group with immediate cord clamping. Cerebral blood volume was not different between these two groups. However, crSO2 was higher in the experimental group during the first 24 h after birth. Additionally, they could observe higher haematocrit values in neonates in the experimental group compared with the control group. These findings suggest that delayed clamping of the umbilical cord results in higher crSO2 and improves cerebral oxygenation during the first day of life. This observation might reflect that DCC led to higher haematocrit concentration. Since the concentration of the oxygen carrier is higher, the oxygen extraction is lower, which led to the significantly higher crSO2 in the DCC group55. Contrary to this, Finn et al. described in their randomized controlled trial of 45 neonates, 12 neonates with immediate cord clamping, 19 neonates with umbilical cord milking and 14 neonates with DCC, that there were no significant differences between groups for measurements of EEG activity or cerebral oxygenation, during the first 12 h of life56.
Fetal inflammatory response syndrome
Fetal inflammatory response syndrome (FIRS) is associated with an increased risk of neonatal morbidity and mortality. Wolfsberger et al., investigated a potential influence of FIRS on cerebral oxygenation in preterm neonates. There were no significant differences in crSO2 within the first 15 min after birth comparing neonates with and without FIRS, but at several time points, SpO2 and heart rate were significantly lower in the FIRS group. In preterm neonates with FIRS, the crSO2 was similar despite significantly lower cFTOE values compared to neonates without FIRS. This observation may be a result of compromised oxygen consumption and delivery in preterm neonates in the first minutes after birth. This suggests that in the FIRS group not only oxygen consumption, but also oxygen delivery was lower resulting in a similar crSO2 in both groups57.
Additional information provided by NIRS:
-
The presence of IUGR is associated with higher crSO2 values. This observation indicates an increase in cerebral oxygen delivery due to increased hemoglobin concentration and increased cardiac output due to brain sparing phenomenon.
-
Delayed cord clamping results in higher crSO2 values and improves cerebral oxygenation during the first day of life. This might be the consequence of DCC leading to higher haematocrit concentrations.
crSO2 as a proxy for complex physiology
All the associations above prove the fact that crSO2 is a parameter that might serve as a proxy covering many aspects of the complex physiology in neonatal transition. Thus, it seems clear, that the clinical use of NIRS monitoring may be indicated for several conditions, not only oxygenation saturation monitoring alone, as described above. NIRS monitoring displays all these aspects within one parameter, the regional cerebral oxygen saturation. Based on the data of COSGOD I/II trial, the COSGOD III trial has been initiated to investigate whether such an approach is able to improve the overall outcome of preterm infants. The primary objective of this multi-center, multi-national phase III clinical trial - COSGOD III - is to figure out if additional monitoring of crSO2 with dedicated interventions may improve the outcome of preterm neonates as evidenced by increased survival without cerebral injury. 724 preterm infants <32 weeks of gestation has been included in this multi-center study. Recruitment has started in September 2018 and was completed in October 202158.
Summary and future directions
cNIRS provides the advantage of continuous, non-invasive, and objective brain monitoring. It is feasible in preterm and term neonates during fetal to neonatal transition, even when clinical interventions (respiratory, medical support and chest compression) are performed. CrSO2 depends on oxygenation and HR, but also on ventilatory, hemodynamic and metabolic measures. Regarding pathologies such as cerebral injuries and IUGR, crSO2 immediately after birth can provide additional information, as it shows different behavior patterns despite stable SpO2 and HR parameters. CrSO2 monitoring provides additional information that cannot be obtained by SpO2 or HR measurement alone and, therefore, may be useful to guide clinical interventions. A first randomized trial proved feasibility of a clinical NIRS approach during fetal to neonatal transition, and was able to reduce the burden of cerebral hypoxia significantly. The currently running COSGOD III trial will provide further information regarding the contribution of cNIRS monitoring to guide respiratory and medical support and its impact on improvement of neonatal outcomes.
Change history
23 June 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41390-022-02173-x
References
Rudolph, A. M. Fetal and neonatal pulmonary circulation. Annu. Rev. Physiol. 41, 383–395 (1979).
Apgar, V. A proposal for a new method of evaluation of the newborn infant. Curr. Res Anesth. Analg. 32, 260–267 (1953).
Casey, B. M., McIntire, D. D. & Leveno, K. J. The continuing value of the Apgar score for the assessment of newborn infants. N. Engl. J. Med 344, 467–471 (2001).
O’Donnell, C. P., Kamlin, C. O., Davis, P. G., Carlin, J. B. & Morley, C. J. Clinical assessment of infant colour at delivery. Arch. Dis. Child Fetal Neonatal Ed. 92, F465–F467 (2007).
O’Donnell, C. P., Kamlin, C. O., Davis, P. G., Carlin, J. B. & Morley, C. J. Interobserver variability of the 5-minute Apgar score. J. Pediatr. 149, 486–489 (2006).
Madar, J. et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 161, 291–326 (2021).
Pichler, G., Cheung, P. Y., Aziz, K., Urlesberger, B. & Schmölzer, G. M. How to monitor the brain during immediate neonatal transition and resuscitation? A systematic qualitative review of the literature. Neonatology 105, 205–210 (2014).
van Bel, F., Lemmers, P. & Naulaers, G. Monitoring neonatal regional cerebral oxygen saturation in clinical practice: value and pitfalls. Neonatology 94, 237–244 (2008).
Jobsis, F. F. Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 198, 1264–1267 (1977).
Edwards, A. D. et al. Cotside measurement of cerebral blood flow in ill newborn infants by near infrared spectroscopy. Lancet 2, 770–771 (1988).
McCormick, P. W. et al. Noninvasive cerebral optical spectroscopy for monitoring cerebral oxygen delivery and hemodynamics. Crit. Care Med 19, 89–97 (1991).
Peebles, D. M. et al. Changes in human fetal cerebral oxygenation and blood volume during delivery. Am. J. Obstet. Gynecol. 167, 1916–1917 (1992).
Isobe, K. et al. Changes in cerebral hemoglobin concentration and oxygen saturation immediately after birth in the human neonate using full-spectrum near infrared spectroscopy. J. Biomed. Opt. 5, 283–286 (2000).
Isobe, K. et al. Measurement of cerebral oxygenation in neonates after vaginal delivery and cesarean section using full-spectrum near infrared spectroscopy. Comp. Biochem Physiol. A Mol. Integr. Physiol. 132, 133–138 (2002).
Fauchère, J. C. et al. Near-infrared spectroscopy measurements of cerebral oxygenation in newborns during immediate postnatal adaptation. J. Pediatr. 156, 372–376 (2010).
Urlesberger, B. et al. Regional oxygen saturation of the brain and peripheral tissue during birth transition of term infants. J. Pediatr. 157, 740–744 (2010).
Binder, C. et al. Cerebral and peripheral regional oxygen saturation during postnatal transition in preterm neonates. J. Pediatr. 163, 394–399 (2013).
Schwaberger, B. et al. Even mild respiratory distress alters tissue oxygenation significantly in preterm infants during neonatal transition. Physiol. Meas. 35, 2085–2099 (2014).
Pichler, G. et al. Reference ranges for regional cerebral tissue oxygen saturation and fractional oxygen extraction in neonates during immediate transition after birth. J. Pediatr. 163, 1558–1563 (2013).
Baik, N. et al. Reference Ranges for Cerebral Tissue Oxygen Saturation Index in Term Neonates during Immediate Neonatal Transition after Birth. Neonatology 108, 283–286 (2015).
Welsford, M. et al. International Liaison Committee on Resuscitation Neonatal Life Support Task Force: Initial Oxygen Use for Preterm Newborn Resuscitation: A Systematic Review With Meta-analysis. Pediatrics 143, e20181828 (2019).
Dawson, J. A. et al. Defining the reference range for oxygen saturation for infants after birth. Pediatrics 125, e1340–e1347 (2010).
Baik, N. et al. Cerebral haemorrhage in preterm neonates: does cerebral regional oxygen saturation during the immediate transition matter? Arch. Dis. Child Fetal Neonatal Ed. 100, F422–F427 (2015).
Fuchs, H. et al. Brain oxygenation monitoring during neonatal resuscitation of very low birth weight infants. J. Perinatol. 32, 356–362 (2012).
Oei, J. L. et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 103, F446–F454 (2018).
Binder-Heschl, C. et al. Oxygen Saturation Targeting During Delivery Room Stabilization: What Does This Mean for Regional Cerebral Oxygenation? Front Pediatr. 7, 274 (2019).
Pichler, G. et al. Cerebral Oxygen Saturation to Guide Oxygen Delivery in Preterm Neonates for the Immediate Transition after Birth: A 2-Center Randomized Controlled Pilot Feasibility Trial. J. Pediatr. 170, 73–8.e1 (2016).
Kapadia, V. et al. Outcomes of delivery room resuscitation of bradycardic preterm infants: A retrospective cohort study of randomised trials of high vs low initial oxygen concentration and an individual patient data analysis. Resuscitation 167, 209–217 (2021).
Bresesti I. et al. Impact of bradycardia and hypoxemia on oxygenation in preterm infants requiring respiratory support at birth. Resuscitation 164, 62–69 (2021).
Schwaberger, B. et al. Transitional changes in cerebral blood volume at birth. Neonatology 108, 253–258 (2015).
Wyatt, J. S. et al. Response of cerebral blood volume to changes in arterial carbon dioxide tension in preterm and term infants. Pediatr. Res 29, 553–557 (1991).
Schwaberger, B. et al. Cerebral blood volume during neonatal transition in term and preterm infants with and without respiratory support. Front Pediatr. 6, 132 (2018).
Noori, S. et al. Transitional changes in cardiac and cerebral hemodynamics in term neonates at birth. J. Pediatr. 160, 943–948 (2012).
Fuchs, H. et al. Cerebral oxygenation in very low birth weight infants supported with sustained lung inflations after birth. Pediatr. Res 70, 176–180 (2011).
Schwaberger, B. et al. Do sustained lung inflations during neonatal resuscitation affect cerebral blood volume in preterm infants? a randomized controlled pilot study. PLoS One 10, e0138964 (2015).
Li, E. S., Cheung, P. Y., Pichler, G., Aziz, K. & Schmölzer, G. M. Respiratory function and near infrared spectroscopy recording during cardiopulmonary resuscitation in an extremely preterm newborn. Neonatology 105, 200–204 (2014).
Badurdeen, S. et al. Excess cerebral oxygen delivery follows return of spontaneous circulation in near-term asphyxiated lambs. Sci. Rep. 10, 16443–020 (2020).
Urlesberger, B. et al. A left-to-right shunt via the ductus arteriosus is associated with increased regional cerebral oxygen saturation during neonatal transition. Neonatology 103, 259–263 (2013).
Baik, N. et al. Foramen ovale (FO) - The underestimated sibling of ductus arteriosus (DA): Relevance during neonatal transition. Early Hum. Dev. 103, 137–140 (2016).
Baik, N. et al. Blood pressure during the immediate neonatal transition: is the mean arterial blood pressure relevant for the cerebral regional oxygenation? Neonatology 112, 97–102 (2017).
Naulaers, G. et al. Use of tissue oxygenation index and fractional tissue oxygen extraction as non-invasive parameters for cerebral oxygenation. A validation study in piglets. Neonatology 92, 120–126 (2007).
Wong, F. Y. et al. Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics 121, e604–e611 (2008).
Seri, I., Rudas, G., Bors, Z., Kanyicska, B. & Tulassay, T. Effects of low-dose dopamine infusion on cardiovascular and renal functions, cerebral blood flow, and plasma catecholamine levels in sick preterm neonates. Pediatr. Res 34, 742–749 (1993).
Baik-Schneditz N. et al. Cardiac output and cerebral oxygenation in term neonates during neonatal transition. Children 8, 439 (2021).
Bruckner, M. et al. Cerebral and peripheral tissue oxygenation in stable neonates: Absent influence of cardiac function. Acta Paediatrica 109, 1560–1569 (2020).
Tamussino, A. et al. Low cerebral activity and cerebral oxygenation during immediate transition in term neonates-A prospective observational study. Resuscitation 103, 49–53 (2016).
Matterberger, C. et al. Blood glucose and cerebral tissue oxygenation immediately after birth-an observational study. J. Pediatr. 200, 19–23 (2018).
Bruckner M. et al. Association between regional tissue oxygenation and body temperature in term and preterm infants born by caesarean section. Children 7, 205 (2020).
Garite, T. J., Clark, R. & Thorp, J. A. Intrauterine growth restriction increases morbidity and mortality among premature neonates. Am. J. Obstet. Gynecol. 191, 481–487 (2004).
Baik-Schneditz, N. et al. Effect of intrauterine growth restriction on cerebral regional oxygen saturation in preterm and term neonates during immediate postnatal transition. Neonatology 117, 324–330 (2020).
Baschat, A. A. & Harman, C. R. Antenatal assessment of the growth restricted fetus. Curr. Opin. Obstet. Gynecol. 13, 161–168 (2001).
Katheria, A. C. et al. Measuring cardiac changes using electrical impedance during delayed cord clamping: a feasibility trial. Matern Health Neonatol. Perinatol. 1, 15–015 (2015).
Padilla-Sánchez, C. et al. Delayed vs immediate cord clamping changes oxygen saturation and heart rate patterns in the first minutes after birth. J. Pediatr. 227, 149–156.e1 (2020).
Katheria, A. C. et al. Delayed cord clamping in newborns born at term at risk for resuscitation: a feasibility randomized clinical trial. J. Pediatr. 187, 313–317.e1 (2017).
Baenziger, O. et al. The influence of the timing of cord clamping on postnatal cerebral oxygenation in preterm neonates: a randomized, controlled trial. Pediatrics 119, 455–459 (2007).
Finn D. et al. Clamping the Umbilical Cord in Premature Deliveries (CUPiD): Neuromonitoring in the Immediate Newborn Period in a Randomized, Controlled Trial of Preterm Infants Born at <32 Weeks of Gestation. J Pediatr 208, 121–126 (2019).
Wolfsberger, C. H. et al. Fetal Inflammatory Response Syndrome and Cerebral Oxygenation During Immediate Postnatal Transition in Preterm Neonates. Front Pediatr. 8, 401 (2020).
Pichler G. et al. Cerebral regional tissue Oxygen Saturation to Guide Oxygen Delivery in preterm neonates during immediate transition after birth (COSGOD III): an investigator-initiated, randomized, multi-center, multi-national, clinical trial on additional cerebral tissue oxygen saturation monitoring combined with defined treatment guidelines versus standard monitoring and treatment as usual in premature infants during immediate transition: study protocol for a randomized controlled trial. Trials. 20, 178 (2019).
Author information
Authors and Affiliations
Contributions
(I) Conception and design: NBS, BS, GP, BU. (II) Administrative support: IB, HF, IL, NB, GL, MV, CBH. (III) Data analysis and interpretation: All authors. (IV) Manuscript writing: All authors (V) Final approval of manuscript: All authors
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: all author names were interchanged and they have now been corrected.
Supplementary information
Rights and permissions
About this article
Cite this article
Baik-Schneditz, N., Schwaberger, B., Bresesti, I. et al. Fetal to neonatal transition: what additional information can be provided by cerebral near infrared spectroscopy?. Pediatr Res (2022). https://doi.org/10.1038/s41390-022-02081-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-022-02081-0