Abstract
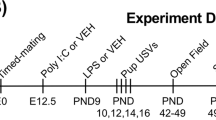
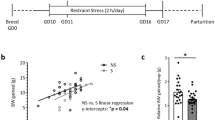
Maternal immune activation (MIA) puts offspring at greater risk for neurodevelopmental disorders associated with impaired social behavior. While it is known that immune signaling through maternal, placental, and fetal compartments contributes to these phenotypical changes, it is unknown to what extent the stress response to illness is involved and how it can be harnessed for potential interventions. To this end, on gestational day 15, pregnant rat dams were administered the bacterial mimetic lipopolysaccharide (LPS; to induce MIA) alongside metyrapone, a clinically available 11β-hydroxylase (11βHSD) inhibitor used to treat hypercortisolism in pregnant, lactating, and neonatal populations. Maternal, placental, and fetal brain levels of corticosterone and placental 11βHSD enzymes type 1 and 2 were measured 3-hrs post treatment. Offspring social behaviors were evaluated across critical phases of development. MIA was associated with increased maternal, placental, and fetal brain corticosterone concentrations that were diminished with metyrapone exposure. Metyrapone protected against reductions in placental 11βHSD2 in males only, suggesting that less corticosterone was inactivated in female placentas. Behaviorally, metyrapone-exposure attenuated MIA-induced social disruptions in juvenile, adolescent, and adult males, while females were unaffected or performed worse. Metyrapone-exposure reversed MIA-induced transcriptional changes in monoamine-, glutamate-, and GABA-related genes in adult male ventral hippocampus, but not in females. Taken together, these findings illustrate that MIA-induced HPA responses act alongside the immune system to produce behavioral deficits. As a clinically available drug, the sex-specific benefits and constraints of metyrapone should be investigated further as a potential means of reducing neurodevelopmental risks due to gestational MIA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Data availability
RNA-seq data has been deposited to GEO (GSE240604). All other data is available on request.
Code availability
There is no code associated with this work.
Change history
05 April 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41386-024-01849-8
References
Han VX, Patel S, Jones HF, Nielsen TC, Mohammad SS, Hofer MJ, et al. Maternal acute and chronic inflammation in pregnancy is associated with common neurodevelopmental disorders: a systematic review. Transl Psychiatry. 2021;11:71.
Quagliato LA, de Matos U, Nardi AE. Maternal immune activation generates anxiety in offspring: a translational meta-analysis. Transl Psychiatry. 2021;11:245.
Estes ML, McAllister AK. Maternal immune activation: implications for neuropsychiatric disorders. Science. 2016;353:772–7.
Wu WL, Hsiao EY, Yan Z, Mazmanian SK, Patterson PH. The placental interleukin-6 signaling controls fetal brain development and behavior. Brain Behav Immun. 2017;62:11–23.
Choi GB, Yim YS, Wong H, Kim S, Kim H, Kim SV, et al. The maternal interleukin-17a pathway in mice promotes autism-like phenotypes in offspring. Science. 2016;351:933–9.
Hsiao EY, McBride SW, Chow J, Mazmanian SK, Patterson PH. Modeling an autism risk factor in mice leads to permanent immune dysregulation. Proc Natl Acad Sci USA. 2012;109:12776–81.
Stelzer IA, Urbschat C, Schepanski S, Thiele K, Triviai I, Wieczorek A, et al. Vertically transferred maternal immune cells promote neonatal immunity against early life infections. Nat Commun. 2021;12:4706.
Iqbal M, Ho HL, Petropoulos S, Moisiadis VG, Gibb W, Matthews SG. Pro-inflammatory cytokine regulation of P-glycoprotein in the developing blood-brain barrier. PLoS One. 2012;7:e43022.
Glover V, O’Donnell KJ, O’Connor TG, Fisher J. Prenatal maternal stress, fetal programming, and mechanisms underlying later psychopathology-A global perspective. Dev Psychopathol. 2018;30:843–54.
Wyrwoll CS, Holmes MC. Prenatal excess glucocorticoid exposure and adult affective disorders: a role for serotonergic and catecholamine pathways. Neuroendocrinology. 2012;95:47–55.
Núñez Estevez KJ, Rondón-Ortiz AN, Nguyen JQT, Kentner AC. Environmental influences on placental programming and offspring outcomes following maternal immune activation. Brain Behav Immun. 2020;83:44–55.
Neumann ID, Johnstone HA, Hatzinger M, Liebsch G, Shipston M, Russell JA, et al. Attenuated neuroendocrine responses to emotional and physical stressors in pregnant rats involve adenohypophysial changes. J Physiol. 1998;508:289–300.
Wyrwoll CS, Holmes MC, Seckl JR. 11β-hydroxysteroid dehydrogenases and the brain: from zero to hero, a decade of progress. Front Neuroendocrinol. 2011;32:265–86.
Welberg LA, Seckl JR, Holmes MC. Inhibition of 11beta-hydroxysteroid dehydrogenase, the foeto-placental barrier to maternal glucocorticoids, permanently programs amygdala GR mRNA expression and anxiety-like behaviour in the offspring. Eur J Neurosci. 2000;12:1047–54.
Mairesse J, Lesage J, Breton C, Bréant B, Hahn T, Darnaudéry M, et al. Maternal stress alters endocrine function of the feto-placental unit in rats. Am J Physiol Endocrinol Metab. 2007;292:E1526–33.
Jensen Peña C, Monk C, Champagne FA. Epigenetic effects of prenatal stress on 11β-hydroxysteroid dehydrogenase-2 in the placenta and fetal brain. PLoS One. 2012;7:e39791.
Sze Y, Fernandes J, Kołodziejczyk ZM, Brunton PJ. Maternal glucocorticoids do not directly mediate the effects of maternal social stress on the fetus. J Endocrinol. 2022;255:143–58.
Straley ME, Togher KL, Nolan AM, Kenny LC, O’Keeffe GW. LPS alters placental inflammatory and endocrine mediators and inhibits fetal neurite growth in affected offspring during late gestation. Placenta. 2014;35:533–8.
Connors EJ, Shaik AN, Migliore MM, Kentner AC. Environmental enrichment mitigates the sex-specific effects of gestational inflammation on social engagement and the hypothalamic pituitary adrenal axis-feedback system. Brain Behav Immun. 2014;42:178–90.
Zhao X, Rondón-Ortiz AN, Lima EP, Puracchio M, Roderick RC, Kentner AC. Therapeutic efficacy of environmental enrichment on behavioral, endocrine, and synaptic alterations in an animal model of maternal immune activation. Brain Behav Immun Health. 2020;3:100043.
Zhao X, Mohammed R, Tran H, Erickson M, Kentner AC. Poly (I:C)-induced maternal immune activation modifies ventral hippocampal regulation of stress reactivity: prevention by environmental enrichment. Brain Behav Immun. 2021;95:203–15.
Azzola A, Eastabrook G, Matsui D, Berberich A, Tirona RG, Gray D, et al. Adrenal cushing syndrome diagnosed during pregnancy: successful medical management with metyrapone. J Endocr Soc. 2020;5:bvaa167.
Kersten M, Hancke K, Janni W, Kraft K. Pregnancy induced Cushing’s syndrome and primary aldosteronism: a case report. BMC Pregnancy Childbirth. 2020;20:421.
Bass IR, Leiter A, Pozharny Y, Shrivastava R, Shah NA. Cushing disease treated successfully with metyrapone during pregnancy. AACE Clin Case Rep. 2021;8:78–81.
Duke ME, Britten FL, Pretorius CJ, McWhinney BC, Ungerer JPJ, Barrett HL, et al. Maternal metyrapone use during breastfeeding: safe for the breastfed infant. J Endocr Soc. 2019;3:973–8.
Lourenço R, Dias P, Gouveia R, Sousa AB, Oliveira G. Neonatal McCune-Albright syndrome with systemic involvement: a case report. J Med Case Rep. 2015;9:189.
de Mingo C, Brugada M, León S, Moreno F, Vila N, Palanques-Pastor T, et al. Metyrapone as treatment in the neonatal McCune–Albright syndrome. J Pediatr Endocrinol Metab. 2020;33:1093–6.
Leret ML, Rua C, Garcia-Montojo M, Lecumberri M, González JC. Influence of metyrapone treatment during pregnancy on the development and maturation of brain monoaminergic systems in the rat. Acta Physiol (Oxf). 2009;197:333–40.
Ménard J, Rigel DF, Watson C, Jeng AY, Fu F, Beil M, et al. Aldosterone synthase inhibition: cardiorenal protection in animal disease models and translation of hormonal effects to human subjects. J Transl Med. 2014;12:340.
Minck D, Braithwaite E. Non-clinical reviews: osilodrostat. FDA center for drug evaluation and research. 2019. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2020/212801Orig1s000PharmR.pdf. Accessed 2 August 2023.
Kentner AC, Bilbo SD, Brown AS, Hsiao EY, McAllister AK, Meyer U, et al. Maternal immune activation: reporting guidelines to improve the rigor, reproducibility, and transparency of the model. Neuropsychopharmacology. 2019;44:245–58.
Hayley S, Kelly O, Anisman H. Murine tumor necrosis factor-alpha sensitizes plasma corticosterone activity and the manifestation of shock: modulation by histamine. J Neuroimmunol. 2002;131:60–9.
Bronson SL, Bale TL. Prenatal stress-induced increases in placental inflammation and offspring hyperactivity are male-specific and ameliorated by maternal antiinflammatory treatment. Endocrinology. 2014;155:2635–46.
Miyajima A, Sunouchi M, Mitsunaga K, Yamakoshi Y, Nakazawa K, Usami M. Sexing of postimplantation rat embryos in stored two-dimensional electrophoresis (2-DE) samples by polymerase chain reaction (PCR) of an Sry sequence. J Toxicol Sci. 2009;34:681–5.
Spencer SJ, Martin S, Mouihate A, Pittman QJ. Early-life immune challenge: defining a critical window for effects on adult responses to immune challenge. Neuropsychopharmacology. 2006;31:1910–8.
Bodi CM, Vassoler FM, Byrnes EM. Adolescent experience affects postnatal ultrasonic vocalizations and gene expression in future offspring. Dev Psychobiol. 2016;58:714–23.
Kentner AC, Scalia S, Shin J, Migliore MM, Rondón-Ortiz AN. Targeted sensory enrichment interventions protect against behavioral and neuroendocrine consequences of early life stress. Psychoneuroendocrinology. 2018;98:74–85.
Van Segbroeck M, Knoll AT, Levitt P, Narayanan S. MUPET-Mouse Ultrasonic Profile ExTraction: a signal processing tool for rapid and unsupervised analysis of ultrasonic vocalizations. Neuron. 2017;94:465–85e5.
Yan S, Kentner AC. Mechanical allodynia corresponds to Oprm1 downregulation within the descending pain network of male and female rats exposed to neonatal immune challenge. Brain Behav Immun. 2017;63:148–59.
Scarborough J, Mueller F, Arban R, Dorner-Ciossek C, Weber-Stadlbauer U, Rosenbrock H, et al. Preclinical validation of the micropipette-guided drug administration (MDA) method in the maternal immune activation model of neurodevelopmental disorders. Brain Behav Immun. 2020;88:461–70.
Green SB, Salkind NJ. Using SPSS for Windows and Macintosh Analyzing and Understanding Data. 4th ed. Pearson: New Jersey; 2005.
Ordoñes Sanchez E, Bavley CC, Deutschmann AU, Carpenter R, Peterson DR, Karbalaei R, et al. Early life adversity promotes resilience to opioid addiction-related phenotypes in male rats and sex-specific transcriptional changes. Proc Natl Acad Sci USA. 2021;118:e2020173118.
Miles J, Shevlin M. Applying regression and correlation: a guide for students and researchers. Sage: London; 2001.
Robinson MD, Oshlack A. A scaling normalization method for differential expression analysis of RNA-seq data. Genome Biol. 2010;11:R25.
Cahill KM, Huo Z, Tseng GC, Logan RW, Seney ML. Improved identification of concordant and discordant gene expression signatures using an updated rank-rank hypergeometric overlap approach. Sci Rep. 2018;8:9588. https://doi.org/10.1038/s41598-018-27903-2.
Bonauto SM, Greuel OM, Honeycutt JA. Playback of rat 22-kHz ultrasonic vocalizations as a translational assay of negative affective states: an analysis of evoked behavior and brain activity. Neurosci Biobehav Rev. 2023;20:105396. https://doi.org/10.1016/j.neubiorev.2023.105396.
Knutson B, Burgdorf J, Panksepp J. Ultrasonic vocalizations as indices of affective states in rats. Psychol Bull. 2022;128:961.
Shair HN. Parental potentiation of vocalization as a marker for filial bonds in infant animals. Dev Psychobiol. 2014;56:1689–97. https://doi.org/10.1002/dev.21222.
Brunelli SA, Masmela JR, Shair HN, Hofer MA. Effects of biparental rearing on ultrasonic vocalization (USV) responses of rat pups (Rattus norvegicus). J Comp Psychol. 1998;112:331–43.
Haq SU, Bhat UA, Kumar A. Prenatal stress effects on offspring brain and behavior: mediators, alterations and dysregulated epigenetic mechanisms. J Biosci. 2021;46:34.
Gunn BG, Cunningham L, Cooper MA, Corteen NL, Seifi M, Swinny JD, et al. Dysfunctional astrocytic and synaptic regulation of hypothalamic glutamatergic transmission in a mouse model of early-life adversity: relevance to neurosteroids and programming of the stress response. J Neurosci. 2013;33:19534–54.
Boudouresque F, Guillaume V, Grino M, Strbak V, Chautard T, Conte-Devolx B, et al. Maturation of the pituitary-adrenal function in rat fetuses. Neuroendocrinology. 1988;48:417–22.
Conradt E, Lester BM, Appleton AA, Armstrong DA, Marsit CJ. The roles of DNA methylation of NR3C1 and 11β-HSD2 and exposure to maternal mood disorder in utero on newborn neurobehavior. Epigenetics. 2013;8:1321–9.
Marsit CJ, Maccani MA, Padbury JF, Lester BM. Placental 11-beta hydroxysteroid dehydrogenase methylation is associated with newborn growth and a measure of neurobehavioral outcome. PLoS One. 2012;7:e33794.
Alexander B, Fewell JE. Metyrapone restores the febrile response to Escherichia coli LPS in pregnant rats. Am J Physiol Regul Integr Comp Physiol. 2011;300:R1588–95.
Cui K, Luheshi GN, Boksa P. Effects of endogenous glucocorticoid secretion on the interleukin-6 response to bacterial endotoxin in pregnant and non-pregnant rats. J Endocrinol. 2011;209:95–103.
Hsiao EY, Patterson PH. Activation of the maternal immune system induces endocrine changes in the placenta via IL-6. Brain Behav Immun. 2011;25:604–15.
Bermick J, Watson S, Lueschow S, McElroy SJ. The fetal response to maternal inflammation is dependent upon maternal IL-6 in a murine model. Cytokine 2023;167:156210.
Hodes GE, Ménard C, Russo SJ. Integrating Interleukin-6 into depression diagnosis and treatment. Neurobiol Stress. 2016;4:15–22. https://doi.org/10.1016/j.ynstr.2016.03.003.
Burton MD, Sparkman NL, Johnson RW. Inhibition of interleukin-6 trans-signaling in the brain facilitates recovery from lipopolysaccharide-induced sickness behavior. J Neuroinflammation. 2011;8:54. https://doi.org/10.1186/1742-2094-8-54.
Scattoni ML, Crawley J, Ricceri L. Ultrasonic vocalizations: a tool for behavioural phenotyping of mouse models of neurodevelopmental disorders. Neurosci Biobehav Rev. 2009;33:508–15.
Malkova NV, Yu CZ, Hsiao EY, Moore MJ, Patterson PH. Maternal immune activation yields offspring displaying mouse versions of the three core symptoms of autism. Brain Behav Immun. 2012;26:607–16.
Zhao X, Tran H, DeRosa H, Roderick RC, Kentner AC. Hidden talents: Poly (I:C)-induced maternal immune activation improves mouse visual discrimination performance and reversal learning in a sex-dependent manner. Genes Brain Behav. 2021;20:e12755.
Gzielo K, Potasiewicz A, Litwa E, Piotrowska D, Popik P, Nikiforuk A. The effect of maternal immune activation on social play-induced ultrasonic vocalization in rats. Brain Sci. 2021;11:344.
Meyer U. Prenatal poly(i:C) exposure and other developmental immune activation models in rodent systems. Biol Psychiatry. 2014;75:307–15.
Haida O, Al Sagheer T, Balbous A, Francheteau M, Matas E, Soria F, et al. Sex-dependent behavioral deficits and neuropathology in a maternal immune activation model of autism. Transl Psychiatry. 2019;9:124.
Bitanihirwe BK, Peleg-Raibstein D, Mouttet F, Feldon J, Meyer U. Late prenatal immune activation in mice leads to behavioral and neurochemical abnormalities relevant to the negative symptoms of schizophrenia. Neuropsychopharmacology. 2010;35:2462–78.
Zucker I, Prendergast BJ. Sex differences in pharmacokinetics predict adverse drug reactions in women. Biol Sex Differ. 2020;11:32.
Yoon S, Jeong S, Jung E, Kim KS, Jeon I, Lee Y, et al. Effect of CYP3A4 metabolism on sex differences in the pharmacokinetics and pharmacodynamics of zolpidem. Sci Rep. 2021;11:19150.
Porreca F, Dodick DW. Considering patient sex in prescribing CGRP receptor antagonists for short-term treatment of migraine. JAMA Neurol. July 2023. https://doi.org/10.1001/jamaneurol.2023.2335.
Zohar I, Weinstock M. Differential effect of prenatal stress on the expression of corticotrophin-releasing hormone and its receptors in the hypothalamus and amygdala in male and female rats. J Neuroendocrinol. 2011;23:320–8.
Liu PZ, Nusslock R. How stress gets under the skin: early life adversity and glucocorticoid receptor epigenetic regulation. Curr Genomics. 2018;19:653–64.
Chen Y, Andres AL, Frotscher M, Baram TZ. Tuning synaptic transmission in the hippocampus by stress: the CRH system. Front Cell Neurosci. 2012;6:13.
Sukhareva EV. The role of the corticotropin-releasing hormone and its receptors in the regulation of stress response. Vavilovskii Zh Genet Selektsii. 2021;25:216–23.
Hostetler CM, Ryabinin AE. The CRF system and social behavior: a review. Front Neurosci. 2013;7:92.
Magalhaes AC, Holmes KD, Dale LB, Comps-Agrar L, Lee D, Yadav PN, et al. CRF receptor 1 regulates anxiety behavior via sensitization of 5-HT2 receptor signaling. Nat Neurosci. 2010;13:622–9.
Issler O, Carter RN, Paul ED, Kelly PA, Olverman HJ, Neufeld-Cohen A, et al. Increased anxiety in corticotropin-releasing factor type 2 receptor-null mice requires recent acute stress exposure and is associated with dysregulated serotonergic activity in limbic brain areas. Biol Mood Anxiety Disord. 2014;4:1.
Pleil KE, Skelly MJ. CRF modulation of central monoaminergic function: Implications for sex differences in alcohol drinking and anxiety. Alcohol 2018;72:33–47.
Garbarino VR, Gilman TL, Daws LC, Gould GG. Extreme enhancement or depletion of serotonin transporter function and serotonin availability in autism spectrum disorder. Pharm Res. 2019;140:85–99.
Ottenhof KW, Sild M, Lévesque ML, Ruhé HG, Booij L. TPH2 polymorphisms across the spectrum of psychiatric morbidity: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2018;92:29–42.
Zech M, Lam DD, Weber S, Berutti R, Poláková K, Havránková P, et al. A unique de novo gain-of-function variant in CAMK4 associated with intellectual disability and hyperkinetic movement disorder. Cold Spring Harb Mol Case Stud. 2018;4:a003293.
Sałaciak K, Koszałka A, Żmudzka E, Pytka K. The Calcium/Calmodulin-dependent kinases II and IV as therapeutic targets in neurodegenerative and neuropsychiatric disorders. Int J Mol Sci. 2021;22:4307.
Coon H, Dunn D, Lainhart J, Miller J, Hamil C, Battaglia A, et al. Possible association between autism and variants in the brain-expressed tryptophan hydroxylase gene (TPH2). Am J Med Genet B Neuropsychiatr Genet. 2005;135B:42–6. https://doi.org/10.1002/ajmg.b.30168.
Yang SY, Yoo HJ, Cho IH, Park M, Kim SA. Association with tryptophan hydroxylase 2 gene polymorphisms and autism spectrum disorders in Korean families. Neurosci Res. 2012;73:333–6. https://doi.org/10.1016/j.neures.2012.05.012.
Browne CA, O’Brien FE, Connor TJ, Dinan TG, Cryan JF. Differential lipopolysaccharide-induced immune alterations in the hippocampus of two mouse strains: effects of stress. Neuroscience. 2012;225:237–48. https://doi.org/10.1016/j.neuroscience.2012.08.031.
Van den Hove DL, Leibold NK, Strackx E, Martinez-Claros M, Lesch KP, Steinbusch HW, et al. Prenatal stress and subsequent exposure to chronic mild stress in rats; interdependent effects on emotional behavior and the serotonergic system. Eur Neuropsychopharmacol. 2014;24:595–607. https://doi.org/10.1016/j.euroneuro.2013.09.006.
Hanswijk SI, Spoelder M, Shan L, Verheij MMM, Muilwijk OG, Li W, et al. Gestational factors throughout fetal neurodevelopment: the serotonin link. Int J Mol Sci. 2020;21:5850. https://doi.org/10.3390/ijms21165850.
Fiorentino A, Sharp SI, McQuillin A. Association of rare variation in the glutamate receptor gene SLC1A2 with susceptibility to bipolar disorder and schizophrenia. Eur J Hum Genet. 2015;23:1200–6.
Sellgren CM, Imbeault S, Larsson MK, Oliveros A, Nilsson IAK, Codeluppi S, et al. GRK3 deficiency elicits brain immune activation and psychosis. Mol Psychiatry. 2021;26:6820–32.
Huang G, Chen S, Chen X, Zheng J, Xu Z, Doostparast Torshizi A, et al. Uncovering the functional link between SHANK3 deletions and deficiency in neurodevelopment using iPSC-derived human neurons. Front Neuroanat. 2019;13:23.
White PC. 11beta-hydroxysteroid dehydrogenase and its role in the syndrome of apparent mineralocorticoid excess. Am J Med Sci. 2001;322:308–15. https://doi.org/10.1097/00000441-200112000-00003.
Funder JW. Apparent mineralocorticoid excess. J Steroid Biochem Mol Biol. 2017;165:151–3. https://doi.org/10.1016/j.jsbmb.2016.03.010.zz.
Funding
This project was funded by NIMH under Award Numbers R15MH114035 (to ACK), and R01MH120066 (to MLS), and the Massachusetts College of Pharmacy and Health Sciences (MCPHS) Center for Research and Discovery (to LG). The authors wish to thank Holly DeRosa, Ada Cheng, and Arianna Smith for their technical assistance during earlier phases of this research. The authors would also like to thank the MCPHS Schools of Pharmacy and Arts & Sciences for their continual support, and Azenta Life Sciences where the RNA-seq was performed. The content is solely the responsibility of the authors and does not necessarily represent the official views of any of the financial supporters.
Author information
Authors and Affiliations
Contributions
JM, LG, & MAS ran the experiments; JM, MAS, MLS, & ACK analyzed and interpreted the data; JM and ACK wrote the manuscript; ACK, designed and supervised the study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: In response to a Comment/Letter to the Editor submitted by Karadag et al., (2024), Figures 2B and 2C have been revised to show a “ND” or non-detectable indicator for experimental groups, where the data values fell below the range of the assay, rather than the sensitivity. The associated Figure 2 caption, the results section of the manuscript, and Supplemental Results Table 2 have been revised accordingly. These revisions, based on Karadag’s recommendations, do not change the study findings or conclusions. The data validate that LPS induced an inflammatory response.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Martz, J., Shelton, M.A., Geist, L. et al. Sex differences in offspring risk and resilience following 11β-hydroxylase antagonism in a rodent model of maternal immune activation. Neuropsychopharmacol. (2023). https://doi.org/10.1038/s41386-023-01771-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41386-023-01771-5
This article is cited by
-
Does steroid increase LPS-induced sickness behaviors?
Neuropsychopharmacology (2024)