Abstract
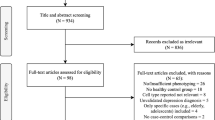
Depression has been associated with inflammatory pathophysiological mechanisms, including alterations in amount of circulating immune cells. However, no meta-analysis within the past 20 years have reevaluated the circulating immune cells in blood and cerebrospinal fluid (CSF) from patients with depression compared to healthy controls. The aim of this study was to systematically evaluate the circulating immune cells in blood and CSF from patients with unipolar depression compared to healthy controls. Databases were searched up until February 12, 2021. Data-extraction was performed by two independent reviewers. 104 studies were included in the meta-analysis using fixed and random-effects models. Patients with depression had a significantly higher overall leukocyte count (35 studies; SMD, 0.46; 95% CI: 0.31–0.60, I2 = 68%), higher neutrophil count (24 studies; SMD, 0.52; 95% CI: 0.33–0.71, I2 = 77%) and higher monocyte count (27 studies; SMD, 0.32; 95% CI: 0.11–0.53, I2 = 77%) compared to healthy controls. Leukocyte counts were higher in inpatients, indicating a relation to depression severity. Furthermore, there were significant alterations in several lymphocyte subsets, including higher natural killer cells and T cell subsets. Higher neutrophil/lymphocyte ratio (11 studies; SMD = 0.24; 95% CI: 0.06–0.42, I2 = 73%), CD4/CD8 cell-ratio (26 studies; SMD = 0.14; 95% CI: 0.01–0.28, I2 = 42%) and T helper 17/T regulatory ratio (2 studies; SMD = 1.05; 95% CI: 0.15–1.95, I2 = 86%) were found in patients compared to healthy controls. CSF white cell count was higher in patients compared to controls (3 studies; SMD = 0.20; 95% CI: 0.01–0.38, I2 = 0%). There were no data for CSF cell subsets. This study suggests that there are several blood immune cell alterations in patients with unipolar depression compared to healthy controls, both in major leukocyte subsets and more specialized immune cell subsets.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Spencer LJ, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–858.
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–17.
Gronemann FH, Jorgensen MB, Nordentoft M, Andersen PK, Osler M. Incidence of, risk factors for, and changes over time in treatment-resistant depression in Denmark: a register-based cohort study. J Clin Psychiatry. 2018;79:17m11845.
Reutfors J, Andersson TML, Brenner P, Brandt L, DiBernardo A, Li G, et al. Mortality in treatment-resistant unipolar depression: a register-based cohort study in Sweden. J Affect Disord. 2018;238:674–9.
Benros ME, Waltoft BL, Nordentoft M, Ostergaard SD, Eaton WW, Krogh J, et al. Autoimmune diseases and severe infections as risk factors for mood disorders: a nationwide study. JAMA Psychiatry. 2013;70:812–20.
Bonaccorso S, Marino V, Biondi M, Grimaldi F, Ippoliti F, Maes M. Depression induced by treatment with interferon-alpha in patients affected by hepatitis C virus. J Affect Disord. 2002;72:237–41.
Köhler OE, Benros M, Nordentoft M, Farkouh ME, Iyengar RL, Mors O, et al. Effect of anti-inflammatory treatment on depression, depressive symptoms, and adverse effects a systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry. 2014;71:1381–91.
Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21:1696–709.
Mousten IV, Sørensen NV, Christensen RHB, Benros ME. Cerebrospinal fluid biomarkers in patients with unipolar depression compared with healthy control individuals: a systematic review and meta-analysis. JAMA Psychiatry. 2022. https://doi.org/10.1001/jamapsychiatry.2022.0645.
Kohler CA, Freitas TH, Maes M, de Andrade NQ, Liu CS, Fernandes BS, et al. Peripheral cytokine and chemokine alterations in depression: a meta-analysis of 82 studies. Acta Psychiatr Scand. 2017;135:373–87.
Mazza MG, Lucchi S, Tringali AGM, Rossetti A, Botti ER, Clerici M. Neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in mood disorders: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2018;84:229–36.
Herbert TB, Cohen S. Depression and immunity: a meta-analytic review. Psychol Bull. 1993;113:472–86.
Zorrilla EP, Luborsky L, McKay JR, Rosenthal R, Houldin A, Tax A, et al. The relationship of depression and stressors to immunological assays: a meta-analytic review. Brain Behav Immun. 2001;15:199–226.
Lynall M-E, Turner L, Bhatti J, Cavanagh J, de Boer P, Mondelli V, et al. Peripheral blood cell-stratified subgroups of inflamed depression. Biol Psychiatry. 2020;88:185–96.
Hasselmann H, Gamradt S, Taenzer A, Nowacki J, Zain R, Patas K, et al. Pro-inflammatory monocyte phenotype and cell-specific steroid signaling alterations in unmedicated patients with major depressive disorder. Front Immunol. 2018;9:2693.
Cai L, Xu L, Wei L, Chen W. Relationship of mean platelet volume to MDD: a retrospective study. Shanghai Arch Psychiatry. 2017;29:21–29.
Euteneuer F, Dannehl K, del Rey A, Engler H, Schedlowski M, Rief W. Peripheral immune alterations in major depression: the role of subtypes and pathogenetic characteristics. Front Psychiatry. 2017;8:250.
Grosse L, Carvalho LA, Birkenhager TK, Hoogendijk WJ, Kushner SA, Drexhage HA, et al. Circulating cytotoxic T cells and natural killer cells as potential predictors for antidepressant response in melancholic depression. Restoration of T regulatory cell populations after antidepressant therapy. Psychopharmacology. 2016;;233:1679–88.
Noor Suryani MA, Siti Nor Fairus MS, Che Maraina CH, Wong KK, Mohd Nazri S, Mohd Azhar MY. Major depressive disorder patients on antidepressant treatments display higher number of regulatory T cells. Malays J Pathol. 2019;41:169–76.
Patas K, Willing A, Demiralay C, Engler JB, Lupu A, Ramien C, et al. T cell phenotype and T cell receptor repertoire in patients with major depressive disorder. Front Immunol. 2018;9:291.
Krause D, Stapf TM, Kirnich VB, Hennings A, Riemer S, Chrobok A, et al. Stability of cellular immune parameters over 12 weeks in patients with major depression or somatoform disorder and in healthy controls. Neuroimmunomodulation. 2018;25:7–17.
Becking K, Haarman BCM, Grosse L, Nolen WA, Claes S, Arolt V, et al. The circulating levels of CD4+ t helper cells are higher in bipolar disorder as compared to major depressive disorder. J Neuroimmunol. 2018;319:28–36.
Ahmetspahic D, Schwarte K, Ambrée O, Bürger C, Falcone V, Seiler K, et al. Altered B cell homeostasis in patients with major depressive disorder and normalization of CD5 surface expression on regulatory B cells in treatment responders. J Neuroimmune Pharm. 2018;13:90–99.
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 2021.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Levine S, Rabinowitz J, Faries D, Lawson A, Ascher-Svanum H. Treatment response trajectories and antipsychotic medications: examination of up to 18 months of treatment in the CATIE chronic schizophrenia trial. Schizophr Res. 2012;137:141–6.
Hedges LV. Distribution theory for Glass’s estimator of effect size and related estimators. J Educ Behav Stat. 1981;6:107–28.
Hedges LV. Estimation of effect size from a series of independent experiments. Psychol Bull. 1982;92:490–9.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. https://training.cochrane.org/: Cochrane Training; 2019.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ Br Med J. 1997;315:629.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104:240–3.
Pavon L, Sandoval-Lopez G, Eugenia Hernandez M, Loria F, Estrada I, Perez M, et al. Th2 cytokine response in Major Depressive Disorder patients before treatment. J Neuroimmunol. 2006;172:156–65.
Hattori K, Ota M, Sasayama D, Yoshida S, Matsumura R, Miyakawa T, et al. Increased cerebrospinal fluid fibrinogen in major depressive disorder. Sci Rep. 2015;5:11412.
Lynch CJ, Gunning FM, Liston C. Causes and consequences of diagnostic heterogeneity in depression: paths to discovering novel biological depression subtypes. Biol Psychiatry. 2020;88:83–94.
Köhler-Forsberg O, Buttenschøn HN, Tansey KE, Maier W, Hauser J, Dernovsek MZ, et al. Association between C-reactive protein (CRP) with depression symptom severity and specific depressive symptoms in major depression. Brain Behav Immun. 2017;62:344–50.
Sørensen NV, Orlovska-Waast S, Jeppesen R, Klein-Petersen AW, Christensen RHB, Benros ME. Neuroinflammatory biomarkers in cerebrospinal fluid from 106 patients with recent-onset depression compared with 106 individually matched healthy control subjects. Biol Psychiatry. 2022. https://doi.org/10.1016/j.biopsych.2022.04.002.
Cattane N, Vernon AC, Borsini A, Scassellati C, Endres D, Capuron L, et al. Preclinical animal models of mental illnesses to translate findings from the bench to the bedside: Molecular brain mechanisms and peripheral biomarkers associated to early life stress or immune challenges. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol. 2022;58:55–79.
Bollen J, Trick L, Llewellyn D, Dickens C. The effects of acute inflammation on cognitive functioning and emotional processing in humans: a systematic review of experimental studies. J Psychosom Res. 2017;94:47–55.
Baumeister D, Akhtar R, Ciufolini S, Pariante CM, Mondelli V. Childhood trauma and adulthood inflammation: a meta-analysis of peripheral C-reactive protein, interleukin-6 and tumour necrosis factor-α. Mol Psychiatry. 2016;21:642–9.
Häfner S, Emeny RT, Lacruz ME, Baumert J, Herder C, Koenig W, et al. Association between social isolation and inflammatory markers in depressed and non-depressed individuals: results from the MONICA/KORA study. Brain Behav Immun. 2011;25:1701–7.
Brown SJ, Huang X-F, Newell KA. The kynurenine pathway in major depression: what we know and where to next. Neurosci Biobehav Rev. 2021;127:917–27.
Moncrieff J, Cooper RE, Stockmann T, Amendola S, Hengartner MP, Horowitz MA. The serotonin theory of depression: a systematic umbrella review of the evidence. Mol Psychiatry. 2022. https://doi.org/10.1038/s41380-022-01661-0. Online ahead of print.
Costa-Ferro ZSM, do Prado-Lima PAS, Onsten GA, Oliveira GN, Brito GC, Ghilardi IM, et al. Bone marrow mononuclear cell transplant prevents rat depression and modulates inflammatory and neurogenic molecules. Prog Neuropsychopharmacol Biol Psychiatry. 2022;113:110455.
Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017;60:1–12.
Eyre HA, Lavretsky H, Kartika J, Qassim A, Baune BT. Modulatory effects of antidepressant classes on the innate and adaptive immune system in depression. Pharmacopsychiatry. 2016;49:85–96.
Bauer ME. Stress, glucocorticoids and ageing of the immune system. Stress. 2005;8:69–83.
Johannsen NM, Priest EL, Dixit VD, Earnest CP, Blair SN, Church TS. Association of white blood cell subfraction concentration with fitness and fatness. Br J Sports Med. 2010;44:588–93.
Mehta H, Nazzal K, Sadikot RT. Cigarette smoking and innate immunity. Inflamm Res J Eur Histamine Res Soc. 2008;57:497–503.
Funding
This study was funded by grants from The Lundbeck Foundation (grant number R268–2016–3925 and R277–2018–1411). The funding agencies had no impact on the study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
MEB, SOW and BHF designed the study and systematic literature search. BHF conducted the screening of titles and abstracts. BHF and SOW did full text screening independently. BHF extracted all data. Data was validated by either NVS or SOW. TBB and NØ helped categorize immune cells. RHC made the statistical analysis plan and conducted the statistical analyses. All authors contributed to data interpretation. RHC, NVS and BHF conducted figures and tables. NVS drafted the manuscript including preparation of the supplementary. All authors contributed to the editing of the manuscript and all authors have read and accepted the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sørensen, N.V., Frandsen, B.H., Orlovska-Waast, S. et al. Immune cell composition in unipolar depression: a comprehensive systematic review and meta-analysis. Mol Psychiatry 28, 391–401 (2023). https://doi.org/10.1038/s41380-022-01905-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41380-022-01905-z
This article is cited by
-
Bayesian network-based Mendelian randomization for variant prioritization and phenotypic causal inference
Human Genetics (2024)
-
Identification of mitophagy-related biomarkers and immune infiltration in major depressive disorder
BMC Genomics (2023)
-
Natur und Immunmechanismen psychischer Erkrankungen
Der Nervenarzt (2023)