Abstract
Objective
To evaluate the efficacy and safety of three different modes of non-invasive post-extubation ventilation support in preterm infants with severe respiratory distress syndrome (RDS).
Methods
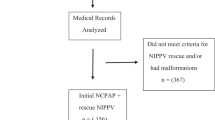
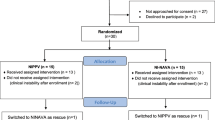
Infants diagnosed with severe RDS after extubation were randomized to receive nasal continuous positive airway pressure ventilation (NCPAP), nasal intermittent positive pressure ventilation (NIPPV), and non-invasive high-frequency oscillatory ventilation (NHFO). The clinical outcomes and complications of infants in different groups were recorded.
Results
In infants less than 32 weeks, NCPAP had a significant increase in extubation failure when compared with NIPPV and NHFO, and the gastrointestinal feeding time, the numbers of apnea, and hospitalization costs in the NCPAP group were significantly higher. The incidence of complications was also higher in the NCPAP group. There was no difference in clinical outcomes and complications in infants greater than 32 weeks.
Conclusion
For infants with severe RDS less than 32 weeks after extubation, NIPPV and NHFO are more cost-effective in comparison to NCPAP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Data availability
The datasets used during the present study are available from the corresponding author upon reasonable request.
References
Permall DL, Pasha AB, Chen XQ. Current insights in non-invasive ventilation for the treatment of neonatal respiratory disease. Ital J Pediatr. 2019;45:105.
Rocha G, Soares P, Gonçalves A, Silva AI, Almeida D, Figueiredo S, et al. Respiratory care for the ventilated neonate. Can Respir J. 2018;2018:7472964.
Azevedo A, Flor-de-Lima F, Rocha G, Rodrigues C, Guimarães H. Impact of changes in perinatal care on bronchopulmonary dysplasia: an overview of the last two decades. J Pediatr Neonat Individ Med. 2017;6:e060208.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, et al. European Consensus Guidelines on the management of respiratory distress syndrome – 2019 update. Neonatology. 2019;115:432–50.
Behnke J, Lemyre B, Czernik C, Zimmer KP, Ehrhardt H, Waitz M. Non-invasive ventilation in neonatology. Dtsch Arztebl Int. 2019;116:177–83.
Foglia EE, Ades A, Napolitano N, Lefelman J, Nadkarni V, Nishisaki A. Factors associated with adverse events during tracheal intubation in the NICU. Neonatology. 2015;108:23–29.
Cummings JJ, Polin RA, Committee on Fetus and Newborn, American Academy of Pediatrics. Noninvasive respiratory support. Pediatrics. 2016;137:e20153758
Moniz M, Silvestre C, Nunes P, Abadesso C, Matias E, Loureiro H, et al. High-frequency oscillatory ventilation in children: a 10-year experience. J Pediatr (Rio J). 2013;89:48–55.
Carvalho CG, Silveira RC, Procianoy RS. Ventilator-induced lung injury in preterm infants. Rev Bras Ter Intensiv. 2013;25:319–26.
Patel RM. Short- and long-term outcomes for extremely preterm infants. Am J Perinatol. 2016;33:318–28.
Thébaud B, Goss KN, Laughon M, Whitsett JA, Abman SH, Steinhorn RH, et al. Bronchopulmonary dysplasia. Nat Rev Dis Prim. 2019;5:78.
Williams E, Greenough A. Respiratory support of infants with congenital diaphragmatic hernia. Front Pediatr. 2021;24:9–808317.
Zhu XW, Shi Y, Shi LP, Liu L, Xue J, Ramanathan R, NHFOV Study Group. Non-invasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: study protocol for a multi-center prospective randomized controlled trial. Trials. 2018;19:319.
Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: a systematic review and meta-analysis. JAMA. 2016;316:611–24.
Goldbart AD, Gozal D. Non-invasive ventilation in preterm infants. Pediatr Pulmonol Suppl. 2004;26:158–61.
Ekhaguere O, Patel S, Kirpalani H. Nasal intermittent mandatory ventilation versus nasal continuous positive airway pressure before and after invasive ventilatory support. Clin Perinatol. 2019;46:517–36.
Chen C-Y, Chou A-K, Chen Y-L, Chou H-C, Tsao P-N, Hsieh W-S. Quality improvement of nasal continuous positive airway pressure therapy in neonatal intensive care unit. Pediatr Neonatol. 2017;58:229–35.
Friedman CA, Menchaca RC, Baker MC, Rivas CK, Laberge RN, Rios EH, et al. Bubble nasal CPAP, early surfactant treatment, and rapid extubation are associated with decreased incidence of bronchopulmonary dysplasia in very-low-birth-weight newborns: efficacy and safety considerations. Respir Care. 2013;58:1134–42.
Verder H, Bohlin K, Kamper J, Lindwall R, Jonsson B. Nasal CPAP and surfactant for treatment of respiratory distress syndrome and prevention of bronchopulmonary dysplasia. Acta Pediatr. 2009;98:1400–8.
DeMauro SB, Millar D, Kirpalani H. Noninvasive respiratory support for neonates. Curr Opin Pediatr. 2014;26:157–62.
Alexiou S, Panitch HB. Physiology of non-invasive respiratory support. Semin Fetal Neonatal Med. 2016;21:174–80.
Mazmanyan P, Mellor K, Dore CJ, Modi N. A randomised controlled trial of flow driver and bubble continuous positive airway pressure in preterm infants in a resource-limited setting. Arch Dis Child Fetal Neonatal Ed. 2016;101:F16–20.
Owen LS, Manley BJ. Nasal intermittent positive pressure ventilation in preterm infants: equipment, evidence, and synchronization. Semin Fetal Neonatal Med. 2016;21:146–53.
Dumpa V, Katz K, Northrup V, Bhandari V. SNIPPV vs NIPPV: does synchronizafion matter? J Perinatol. 2012;32:438–42.
Owen LS, Morley CJ, Dawson JA, Davis PG. Effects of non-synchronised nasal intermittent positive pressure ventilation on spontaneous breathing in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2011;96:422–8.
Meneses J, Bhandari V, Alves JG, Herrmann D. Noninvasive ventilation for respiratory distress syndrome: a randomized controlled trial. Pediatries. 2011;127:300–7.
Ullrich TL, Czernik C, Buhrer C, Schmalisch G, Fischer HS. Nasal high-frequency oscillatory ventilation impairs heated humidification: a neonatal bench study. Pediatr Pulmonol. 2017;52:1455–60.
Fischer HS, Bohlin K, Buhrer C, Schmalisch G, Cremer M, Reiss I, et al. Nasal high-frequency oscillation ventilation in neonates: a survey in five European countries. Eur J Pediatr. 2015;174:465–71.
Mukerji A, Singh B, Helou SE, Fusch C, Dunn M, Belik J, et al. Use of noninvasive high-frequency ventilation in the neonatal intensive care unit: a retrospective review. Am J Perinatol. 2015;30:171–6.
Kugelman A, Durand M. A comprehensive approach to the prevention of bronehopulmonary dysplasia. Pediatr Pulmonol. 2011;46:1153–65.
Hossein A, Ghafari V, Nakhshab M. Nasal intermittent mandatory ventilation (NIMV) versus nasal continuous positive airway pressure (nCPAP) in weaning from mechanical ventilation in preterm infants. J Mazand Univ Med Sci. 2011;84:113–20.
Wang CH, Shi LP, Ma XL, Lin HJ, Xu YP, Du LZ. [Use of noninvasive high-frequency oscillatory ventilation in very low birth weight infants]. Zhonghua Er Ke Za Zhi. 2017;55:177–81.
Malakian A, Bashirnezhadkhabaz S, Aramesh MR, Dehdashtian M. Noninvasive high-frequency oscillatory ventilation versus nasal continuous positive airway pressure in preterm infants with respiratory distress syndrome: a randomized controlled trial. J Matern Fetal Neonatal Med. 2020;33:2601–7.
Davis PG, Henderson-Smart DJ. Nasal continuous positive airways pressure immediately after extubation for preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2003;2:CD000143.
Buzzella B, Claure N, D’Ugard C, Bancalari E. A randomized controlled trial of two nasal continuous positive airway pressure levels after extubation in preterm infants. J Pediatr. 2014;164:46–51.
Author information
Authors and Affiliations
Contributions
GY is the guarantor of the entire study. GY designed this study and defined the intellectual content. HL and ZW did the clinical research and collected the data. GY, HL, and XC analyzed the data. XC did the literature research. GY drafted and revised the paper. All authors have read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Affiliated Hospital of Nanchang University and the guardians of all newborns read and signed the informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yuan, G., Liu, H., Wu, Z. et al. Evaluation of three non-invasive ventilation modes after extubation in the treatment of preterm infants with severe respiratory distress syndrome. J Perinatol 42, 1238–1243 (2022). https://doi.org/10.1038/s41372-022-01461-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-022-01461-y
This article is cited by
-
Peri-extubation settings in preterm neonates: a systematic review and meta-analysis
Journal of Perinatology (2024)