Abstract
Purpose
To assess the relationship between decision quality and mental health outcomes for women and their important others (IO) 3 months following periviable birth.
Method
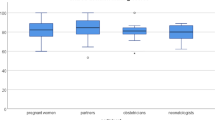
Mental health outcomes were assessed prior to delivery and at 3 months postpartum using depression (PHQ-9), anxiety (GAD-7), and post-traumatic stress disorder (PTSD) (IES-22) scales. Decision quality was measured in terms of Decisional Conflict, Control, Regret, and Satisfaction with Decision. Descriptive analyses and linear regression modeling were conducted using SAS version 9.4.
Result
We recruited 30 eligible women and 16 IOs. Participants had mild anxiety and depression, and symptoms of PTSD were among bereaved parents. Participants with lower decision control had higher levels of depression (women: p = 0.014; IOs: p = 0.059) and anxiety (women: p = 0.053; IOs: p = 0.032). Depression was also associated with higher decisional regret (women: p = 0.073; IOs: p = 0.023).
Conclusion
Our findings suggest that decision quality is associated with mental health outcomes for families who experience periviable delivery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ, et al. Between-hospital variation in treatment and outcomes in extremely preterm infants. New Engl J Med. 2015;372:1801–11.
Clements KM, Barfield WD, Ayadi MF, Wilber N. Preterm birth-associated cost of early intervention services: an analysis by gestational age. Pediatrics. 2007;119:e866.
Gilbert WM, Nesbitt TS, Danielsen B. The cost of prematurity: quantification by gestational age and birth weight. Obstet Gynecol. 2003;102:488–92.
Petrou S, Mehta Z, Hockley C, Cook-Mozaffari P, Henderson J, Goldacre M. The Impact of preterm birth on hospital inpatient admissions and costs during the first 5 years of life. Pediatrics . 2003;112:1290.
Hintz SR, Kendrick DE, Wilson-Costello DE, Das A, Bell EF, Vohr BR, et al. Early-childhood neurodevelopmental outcomes are not improving for infants born at <25 weeks’ gestational age. Pediatrics . 2011;127:62.
Barry MJ, Edgman-Levitan S. Shared decision making—the pinnacle of patient-centered care. New Engl J Med. 2012;366:780–1.
Dupont-Thibodeau A, Barrington KJ, Farlow B, Janvier A. End-of-life decisions for extremely low-gestational-age infants: why simple rules for complicated decisions should be avoided. Semin Perinatol. 2014;38:31–37.
Elwyn G, Frosch D, Rollnick S. Dual equipoise shared decision making: definitions for decision and behaviour support interventions. Implement Sci. 2009;4:75.
Garcia-Retamero R, Galesic MDoc. what would you do if you were me? On self-other discrepancies in medical decision making. J Exp Psychol Appl. 2012;18:38–51.
Mendel R, Hamann J, Traut-Mattausch E, Buhner M, Kissling W, Frey D. ‘What would you do if you were me, doctor?’: randomised trial of psychiatrists’ personal v. professional perspectives on treatment recommendations. Br J Psychiatry. 2010;197:441–7.
Youngblut JM, Brooten D, Cantwell GP, del Moral T, Totapally B. Parent health and functioning 13 months after infant or child NICU/PICU death. Pediatrics . 2013;132:e1295–e1301.
Guest G, Bunce A, Johnson L. How many interviews are enough?: An experiment with data saturation and variability. Field Methods. 2006;18:59–82.
Legare F, Kearing S, Clay K, Gagnon S, D’Amours D, Rousseau M, et al. Are you SURE?: Assessing patient decisional conflict with a 4-item screening test. Can Fam physician. 2010;56:e308–314.
Brehaut JC, O’Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E, et al. Validation of a decision regret scale. Med Decis Making. 2003;23:281–92.
Stalmeier PF, Roosmalen MS, Verhoef LC, Hoekstra-Weebers JE, Oosterwijk JC, Moog U, et al. The decision evaluation scales. Patient Educ Couns. 2005;57:286–93.
Holmes-Rovner M, Kroll J, Schmitt N, Rovner DR, Breer ML, Rothert ML, et al. Patient satisfaction with health care decisions: the satisfaction with decision scale. Med Decis Making. 1996;16:58–64.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092–7.
Beck JG, Grant DM, Read JP, Clapp JD, Coffey SF, Miller LM, et al. The impact of event scale-revised: psychometric properties in a sample of motor vehicle accident survivors. J Anxiety Disord. 2008;22:187–98.
Kuster PA, Badr LK, Chang BL, Wuerker AK, Benjamin AE. Factors influencing health promoting activities of mothers caring for ventilator-assisted children. J Pediatr Nurs. 2004;19:276–87.
Thyen U, Terres NM, Yazdgerdi SR, Perrin JM. Impact of long-term care of children assisted by technology on maternal health. J Dev Behav Pediatr. 1998;19:273–82.
Callahan JL, Borja SE. Psychological outcomes and measurement of maternal posttraumatic stress disorder during the perinatal period. J Perinat Neonatal Nurs. 2008;22:49–59.
Pierrehumbert B, Nicole A, Muller-Nix C, Forcada-Guex M, Ansermet F. Parental post-traumatic reactions after premature birth: implications for sleeping and eating problems in the infant. Arch Dis Child Fetal Neonatal Ed. 2003;88:F400–F404.
Treyvaud K, Lee KJ, Doyle LW, Anderson PJ. Very preterm birth influences parental mental health and family outcomes seven years after birth. J Pediatr. 2014;164:515–21.
Spittle AJ, Treyvaud K, Doyle LW, Roberts G, Lee KJ, Inder TE, et al. Early emergence of behavior and social-emotional problems in very preterm infants. J Am Acad Child Adolesc Psychiatry. 2009;48:909–18.
van der Pal SM, Maguire CM, Bruil J, Le Cessie S, Wit JM, Walther FJ, et al. Health-related quality of life of very pre-term infants’ behaviour at 1 and 2 years of age and parental stress following basic developmental care. Br J Dev Psychol. 2008;26:103–15.
Roque ATF, Lasiuk GC, Radunz V, Hegadoren K. Scoping review of the mental health of parents of infants in the NICU. J Obstet Gynecol Neonatal Nurs. 2017;46:576–87.
Pace CC, Spittle AJ, Molesworth CM, Lee KJ, Northam EA, Cheong JL, et al. Evolution of depression and anxiety symptoms in parents of very preterm infants during the newborn period. JAMA Pediatr. 2016;170:863–70.
Placencia FX, McCullough LB. Biopsychosocial risks of parental care for high-risk neonates: implications for evidence-based parental counseling. J Perinatol. 2012;32:381–6.
Jotzo M, Poets CF. Helping parents cope with the trauma of premature birth: an evaluation of a trauma-preventive psychological intervention. Pediatrics. 2005;115:915–9.
Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118:e1414–1427.
Funding
This study was funding by the National Institutes of Health R21 Exploratory/Developmental Research Grant (HD089032-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tucker Edmonds, B., Laitano, T., Hoffman, S.M. et al. The impact of decision quality on mental health following periviable delivery. J Perinatol 39, 1595–1601 (2019). https://doi.org/10.1038/s41372-019-0403-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0403-0
This article is cited by
-
Context of a neonatal death affects parental perception of end-of-life care, anxiety and depression in the first year of bereavement
BMC Palliative Care (2023)
-
The patient/physician relationship in a post-Roe world: a neonatologist viewpoint
Journal of Perinatology (2023)
-
Decision-making in imminent extreme premature births: perceived shared decision-making, parental decisional conflict and decision regret
Journal of Perinatology (2021)
-
Diverse perspectives on death, disability, and quality of life: an exploratory study of racial differences in periviable decision-making
Journal of Perinatology (2021)