Abstract
Objective
To assess whether combining glucose shape and 2-h glucose concentration during an oral glucose tolerance test (OGTT) may help identifying normal glucose tolerant obese children/adolescents with an impaired glucose tolerant (IGT)-like metabolic profile in term of insulin sensitivity (Matsuda index) and β-cell function (disposition index: DI).
Subjects, methods, and main outcome measure
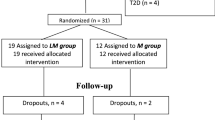
In total, 654 non-diabetic obese children/adolescents underwent a 2 h OGTT. The whole population was classified according to 2-hour plasma glucose ( < 100, 100–119, 120–139, 140–200 mg/dL) and glucose shape (monophasic or biphasic). Monophasic morphology was characterized by an increase in OGTT glucose concentration followed by a decline of at least 4.5 mg/dL, a biphasic response was defined as a decrease in glucose after an initial increase, followed by a second increase of ≥ 4.5 mg/dL. A subset of 69 participants had also a prolonged OGTT to estimate β-cell function in “biphasic” versus “monophasic” patients.
Results
Matsuda index and DI decreased across 2-h glucose categories (both p < 0.001) and were lower in monophasic compared with biphasic children, independently of 2-h glucose category (both p < 0.001, both p for glucose category×shape interaction > 0.05). Normal glucose tolerant children with 2-h glucose of 120–139 mg/dl and monophasic glucose shape did not differ from IGT children, as regards Matsuda index and DI (both p > 0.05). Among children undergoing a prolonged OGTT, those with a monophasic glucose shape had worse β-cell function, modeled as proportional control, than those with a biphasic shape (p = 0.031).
Conclusions
A monophasic OGTT glucose shape is associated with unfavorable glucose metabolism independently of 2-h glucose concentration. Children combining monophasic shape and normal-high 2-h glucose have an IGT-like glucose metabolism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Morandi A, Maschio M, Marigliano M, Miraglia Del Giudice E, Moro B, Peverelli P, et al. Screening for impaired glucose tolerance in obese children and adolescents: a validation and implementation study. Pediatr Obes. 2014;9:17–25.
Körner A, Wiegand S, Hungele A, Tuschy S, Otto KP, l’Allemand-Jander D, et al. Longitudinal multicenter analysis on the course of glucose metabolism in obese children. Int J Obes (Lond). 2013;37:931–6.
Weiss R, Taksali SE, Tamborlane WV, Burgert TS, Savoye M, Caprio S. Predictors of changes in glucose tolerance status in obese youth. Diabetes Care. 2005;28:902–9.
Yeckel CW, Taksali SE, Dziura J, Weiss R, Burgert TS, Sherwin RS, et al. The normal glucose tolerance continuum in obese youth: evidence for impairment in beta-cell function independent of insulin resistance. J Clin Endocrinol Metab. 2005;90:747–54.
Burns SF, Bacha F, Lee SJ, Tfayli H, Gungor N, Arslanian SA. Declining β-cell function relative to insulin sensitivity with escalating OGTT 2-h glucose concentrations in the nondiabetic through the diabetic range in overweight youth. Diabetes Care. 2011;34:2033–40.
Giannini C, Weiss R, Cali A, Bonadonna R, Santoro N, Pierpont B, et al. Evidence for early defects in insulin sensitivity and secretion before the onset of glucose dysregulation in obese youths: a longitudinal study. Diabetes. 2012;61:606–14.
Tschritter O, Fritsche A, Shirkavand F, Machicao F, Häring H, Stumvoll M. Assessing the shape of the glucose curve during an oral glucose tolerance test. Diabetes Care. 2003;26:1026–33.
Nolfe G, Spreghini MR, Sforza RW, Morino G, Manco M. Beyond the morphology of the glucose curve following an oral glucose tolerance test in obese youth. Eur J Endocrinol. 2012;166:107–14.
Kim JY, Coletta DK, Mandarino LJ, Shaibi GQ. Glucose response curve and type 2 diabetes risk in Latino adolescents. Diabetes Care. 2012;35:1925–30.
Kim JY, Michaliszyn SF, Nasr A, Lee S, Tfayli H, Hannon T, et al. The shape of the glucose response curve during an oral glucose tolerance test heralds biomarkers of type 2 diabetes risk in obese youth. Diabetes Care. 2016;39:1431–9.
Abdul-Ghani MA, Lyssenko V, Tuomi T, Defronzo RA, Groop L. The shape of plasma glucose concentration curve during OGTT predicts future risk of type 2 diabetes. Diabetes Metab Res Rev. 2010;26:280–6.
De Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–7.
American Diabetes Association. Classification and diagnosis of diabetes. Diabetes Care. 2017;40:S11–S24.
Harrington DM, Staiano AE, Broyles ST, Gupta AK, Katzmarzyk PT. Waist circumference measurement site does not affect relationships with visceral adiposity and cardiometabolic risk factors in children. Pediatr Obes. 2013;8:199–206.
Maffeis C, Banzato C, Talamini G. Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr. 2008;152:207–13.
Phillips DI, Clark PM, Hales CN, Osmond C. Understanding oral glucose tolerance: comparison of glucose or insulin measurements during the oral glucose tolerance test with specific measurements of insulin resistance and insulin secretion. Diabet Med. 1994;11:286–92.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Yeckel CW, Weiss R, Dziura J, Taksali SE, Dufour S, Burgert TS, et al. Validation of insulin sensitivity indices from oral glucose tolerance test parameters in obese children and adolescent. J Clin Endocrinol Metab. 2004;89:1096–101.
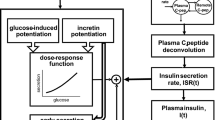
Bonadonna RC, Heise T, Arbet-Engels C, Kapitza C, Avogaro A, Grimsby J, et al. Piragliatin (RO4389620), a novel glucokinase activator, lowers plasma glucose both in the postabsorptive state and after a glucose challenge in patients with type 2 diabetes mellitus: a mechanistic study. J Clin Endocrinol Metab. 2010;95:5028e36.
Bonetti S, Trombetta M, Boselli ML, Turrini F, Malerba G, Trabetti E, et al. Variants of GCKR affect both beta-cell and kidney function in patients with newly diagnosed type 2 diabetes: the Verona newly diagnosed type 2 diabetes study 2. Diabetes Care. 2011;34:1205e10.
Navalesi R, Pilo A, Ferrannini E. Kinetic analysis of plasma insulin disappearance in nonketotic diabetic patients and in normal subjects. A tracer study with 125I-insulin. J Clin Invest. 1978;61:197–208.
Michaliszyn SF, Mari A, Lee S, Bacha F, Tfayli H, Farchoukh L, et al. β-cell function, incretin effect, and incretin hormones in obese youth along the span of glucose tolerance from normal to prediabetes to type 2 iabetes. Diabetes. 2014;63:3846–55.
Kay JP, Alemzadeh R, Langley G, D’Angelo L, Smith P, Holshouser S. Beneficial effects of metformin in normoglycemic morbidly obese adolescents. Metabolism. 2001;50:1457–61.
Reinehr T, Wabitsch M, Kleber M, de Sousa G, Denzer C, Toschke AM. Parental diabetes, pubertal stage, and extreme obesity are the main risk factors for prediabetes in children and adolescents: a simple risk score to identify children at risk for prediabetes. Pediatr Diabetes. 2009;10:395–400.
Goran MI, Gower BA. Longitudinal study on pubertal insulin resistance. Diabetes. 2001;50:2444–50.
Libman IM, Barinas-Mitchell E, Bartucci A, Robertson R, Arslanian S. Reproducibility of the oral glucose tolerance test in overweight children. J Clin Endocrinol Metab. 2008;93:4231–7.
Acknowledgements
We are sincerely indebted to the children and adolescents who participated in the study and to their families. We thank the dedicated staff of the Pediatric Diabetes and Metabolic Disorders Unit of the University Hospital in Verona for their support during the clinical study. Supported by grants (FURMAF2015, FURMAF2016) from the University of Verona to CM and by grants from University of Parma to RCB.
Author information
Authors and Affiliations
Contributions
FO, CZ, and AM researched and analyzed data and wrote the manuscript. MC researched data and discussed the manuscript. MLB carried out mathematical modeling of the data. EF researched data. RCB developed the mathematical models, supervised mathematical modeling, edited the manuscript, and provided substantial contribution to the overall discussion. CM designed the study, researched data, co-wrote, and edited the manuscript. CM is the guarantor of this work and, as such, had full access to all the data in the study and take responsibility for the integrity and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Olivieri, F., Zusi, C., Morandi, A. et al. “IGT-like” status in normoglucose tolerant obese children and adolescents: the additive role of glucose profile morphology and 2-hours glucose concentration during the oral glucose tolerance test. Int J Obes 43, 1363–1369 (2019). https://doi.org/10.1038/s41366-018-0297-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-018-0297-5