Abstract
Background:
Feeding intolerance (FI) occurs commonly in the neonatal intensive care unit. Breast milk contains a large pool of transforming growth factor-beta (TGF-β). Few studies describe TGF-β levels in preterm milk, and the relationship to FI remains unexplored. We measured TGF-β levels in preterm breast milk to investigate a correlation with FI in preterm infants.
Methods:
Prospective observational trial of 100 mother–infant pairs, enrolling infants born below 32 wk gestation and less than 1,500 g, and mothers who planned to provide breast milk. TGF-β levels were measured using enzyme-linked immunosorbent assay. Infant charts were reviewed for outcomes.
Results:
TGF-β declined postnatally, most elevated in colostrum (P < 0.01). TGF-β2 levels were higher than TGF-β1 at all time points (P < 0.01). Colostrum TGF-β levels correlated inversely with birth weight (P < 0.01) and gestational age (P < 0.05). One-week TGF-β2 levels were reduced in growth-restricted infants with FI (P < 0.01). Of infants with necrotizing enterocolitis (NEC), TGF-β2 levels appeared to be low, but small sample size precluded meaningful statistical comparisons.
Conclusion:
TGF-β levels decline temporally in preterm milk. TGF-β1 colostrum levels correlate inversely with birth weight and gestational age. TGF-β2 may play a role in FI in growth-restricted infants. The relationship of TGF-β2 and NEC merits future investigation.
Similar content being viewed by others
Main
Survival of extremely premature neonates has improved greatly over the past several decades. As such, there is a need to provide extrauterine care for these fragile neonates in today’s modern neonatal intensive care units (NICUs). A key component of this care is provision of optimal nutrition, initially via parenteral fluids, but with the eventual goal of transitioning to full enteral feeding, preferably with maternal breast milk. Unfortunately, many of these preterm infants have intermittent feeding intolerance (FI), which may result in interruption of feeding advancement, and therefore suboptimal nutrition.
When clinicians interrupt enteral feeding advancement due to FI, the rationale often is for fear of necrotizing enterocolitis (NEC). NEC remains incompletely understood, despite a significant body of research, but even less is known about FI, despite the high incidence in premature infants. Few studies have sought to understand the epidemiology of FI, and little is known about the correlation with NEC. Despite limited literature, previous studies have used several clinical variables to define FI, including prefeeding gastric residual volume, bilious color of prefeeding gastric residual, abdominal distention, emesis, or withholding of feedings (1,2,3). Although definitions of FI may be synonymous with Bell’s stage I NEC (4), it remains unclear if these two entities are even related.
While proven strategies to reduce NEC are lacking, provision of maternal milk has been established as one preventive method, which can reduce the likelihood of NEC but does not entirely prevent it (5). Breast milk contains multiple growth factors and other bioactive substances not found in standard preterm infant formulas, and as such these factors may contribute to the protective effect of breast milk. In animal as well as human studies, several of these factors have been shown to reduce NEC incidence, including epidermal growth factor (6,7), heparin-binding EGF-like growth factor (8), erythropoietin (9), polyunsaturated fatty acids (10), and others. Although transforming growth factor-beta (TGF-β) is also known to be present in maternal milk, the relationship of this growth factor to NEC has not been fully elucidated. However, a recent animal study demonstrated a reduction in experimental NEC severity in rodents following enteral administration of TGF-β2(11).
TGF-β is an extracellular peptide involved in many cellular functions, including growth, cell differentiation, motility, and cellular death (12,13). Importantly, TGF-β also modulates inflammation, as demonstrated by the lethal phenotype of the TGF-β1 null mouse, in which pathologic specimens demonstrate excessive inflammation (14).
Although TGF-β is known to be present in both amniotic fluid and maternal milk, currently it is not present in commercial infant formulas. The concentration of TGF-β varies widely in maternal breast milk throughout lactation (15,16), with TGF-β2 levels several-fold higher than TGF-β1 levels. Nevertheless, most of the mothers in published studies gave birth to infants at term, and very limited data are available on levels in mothers of preterm infants.
For this study, we sought to determine if the TGF-β levels in maternal colostrum and mature milk correlate with FI in preterm infants as a primary outcome, with the hypothesis that higher levels would be protective against FI. In addition, we examined the incidence of FI, range for levels of TGF-β1 and β2 in these mothers of preterm infants, and several secondary outcomes, including NEC, time to full feeds, time to regain birth weight, length of hospital stay, and mortality.
Results
Demographics
A total of 100 mother–infant pairs were enrolled in this study. Of 100 preterm infants, 8 (8%) did not survive to discharge ( Table 1 ). In all, 41 infants (41%) had FI as defined above, and 5 infants (5%) had stage II–III NEC. FI occurred in 17/33 (52%) infants with a birth weight of 450–800 g, in 15/37 (41%) infants with a birth weight of 801–1,100 g, and in 9/29 (31%) infants with a birth weight of 1,101–1,500 g.
Baseline demographic variables are illustrated in Table 1 . There were no differences noted between the groups with and without FI with respect to gender, gestational age, birth weight, growth restriction, or patent ductus arteriosus. Infants with FI had significantly higher levels of colostrum TGF-β1, as well as higher levels at week 1 and month 1 that did not reach statistical significance. TGF-β2 levels did not differ by FI at any of the time points.
TGF-β Levels in Breast Milk From Mothers of Preterm Infants
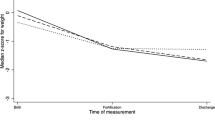
Levels of both TGF-β1 and TGF-β2 declined postnatally in milk samples, with colostrum samples being the most elevated, and 1 mo samples the lowest ( Figure 1 ; P < 0.01 for TGF-β1; P < 0.01 for TGF-β2). TGF-β2 levels were significantly higher than TGF-β1 levels at all time points (P < 0.01 for all). In addition, TGF-β1 levels correlate with TGF-β2 levels in samples at all time points ( Figure 2 and Table 2 ; P < 0.01 for all). Interestingly, increased TGF-β1 colostrum levels were significantly correlated with both decreased birth weight and decreased gestational age (r = −0.30, P < 0.01; r = −0.26, P < 0.05, respectively) ( Table 2 ).
Box plots of transforming growth factor-beta 1 (TGF-β1) (left side) and TGF-β2 (right side). TGF-β levels determined by enzyme-linked immunosorbent assay (ELISA) in expressed breast milk (EBM) collected within 48 h (colostrum), at 1 wk, and 1 mo. Levels of TGF-β1 and TGF-β2 are highest in colostrum and decline over time (P < 0.01 for both). *Significant differences from baseline (P < 0.01).
Transforming growth factor-beta 1 (TGF-β1) levels (on the x-axis) correlate with TGF-β2 levels (on the y-axis). TGF-β levels were measured by enzyme-linked immunosorbent assay (ELISA) in (a) colostrum, (b) at 1 wk and (c) 1 mo of age. Both isoforms correlated at each time point: (a) colostrum: R2 = 0.348; P < 0.01. (b) 1 wk: R2 = 0.443; P < 0.01. (c) 1 mo: R2 = 0.629; P < 0.01. TGF-β levels are shown as the natural log of pg/ml.
TGF-β Levels and Relationship to FI
FI correlated with colostrum TGF-β1, but not with any other TGF-β level. However, this relationship was no longer significant after multivariable regression. Month 1 TGF-β1 had a negative correlation with time to regaining birth weight (r = −0.23, P < 0.05) (data not shown). After multivariable adjustment, predictors for FI included growth restriction and an interaction between week 1 TGF-β2 and growth restriction ( Table 3 ). In mothers who delivered infants with intrauterine growth restriction (IUGR), milk TGF-β2 levels at 1 wk after delivery were significantly lower in those who had FI, compared with those who did not experience FI ( Figure 3 ; P < 0.01). There was no significant difference between TGF-β2 levels at 1 wk and FI within non-IUGR infants (P = 0.11). Colostrum and 1 mo samples were not different in IUGR infants, nor were TGF-β1 levels at any time point.
Mean levels of week 1 transforming growth factor-beta 2 (TGF-β2) by feeding intolerance (FI) within intrauterine growth restriction (IUGR) and non-IUGR infants. TGF-β2 levels at 1 wk are significantly lower for IUGR infants with FI compared with those with no FI (P = 0.007). There is no difference in TGF-β2 levels for non-IUGR infants by FI (P = 0.11). TGF-β levels are shown as the natural log of pg/ml. The gray triangle indicates the mean for infants with FI, and the gray lines represent the standard errors. The black triangle indicates the mean for infants with no FI, and the black lines represent the standard errors.
TGF-β Levels and Relationship to NEC
In this study, only 5% of the infants developed NEC. Given the small number of babies affected with NEC, we were unable to make meaningful statistical comparisons for this study. However, some intriguing findings were noted. Many clinicians are concerned about infants who have FI subsequently developing NEC. However, in this study, the infants who developed stage II and III NEC did not have any signs of prior FI as defined by this study. In fact, of the five infants affected by NEC, three had no signs of FI at any point prior to developing NEC. For the other two, one had feedings held for just a few hours for abdominal distention and a large gastric residual, but feeds were then resumed without incident until the development of NEC 6 d later. The fifth infant had some ongoing small gastric residuals that were somewhat bilious over the first several days of feeding, but the treating physicians did not feel that cessation of feeds was necessary at any point, as the remainder of the abdominal assessment was normal, and NEC subsequently developed on day 21 of life.
Intriguingly, TGF-β2 levels were lower in both colostrum and 1 wk samples in NEC patients compared with non-NEC patients (7.9 ± 2.1 vs. 9.0 ± 1.4; 8.3 ± 2.2 vs. 8.8 ± 1.3, respectively) ( Figure 4 ). Due to the small number of infants affected by NEC, however, this did not reach statistical significance.
Mean levels of colostrum and week 1 transforming growth factor-beta 2 (TGF-β2) levels by infants with and without necrotizing enterocolitis (NEC). There are five infants with NEC so differences did not reach statistical significance (colostrum P = 0.19; 1 wk P = 0.052). TGF-β levels are shown as the natural log of pg/ml. The gray triangle indicates the mean for infants with NEC, and the gray lines represent the standard errors. The black circle indicates the mean for infants without NEC, and the black lines represent the standard errors.
We do not have specific details about TGF-β levels in milk at the time of NEC diagnosis. However, we have limited information on each subject that developed NEC. The first to develop NEC in our study did so at 2 mo of age. The mother’s colostrum TGF-β2 level was actually high (59,921 pg/ml), but given the age at diagnosis, the colostrum was likely fed to him many weeks prior. The 1 wk level was quite low at 495 pg/ml. The second infant developed NEC on day 8 of life. That mother’s colostrum TGF-β2 level was quite low at 885 pg/ml. Although she likely did not receive the 1 wk milk, that level was also very low at 1,604 pg/ml. The third infant was diagnosed with NEC on day 22 of life. It was not possible to measure that mother’s colostrum TGF-β level as the sample volume was small. The 1 wk level was elevated at 161,809 pg/ml. The fourth infant affected by NEC was diagnosed at 20 d of life. The maternal colostrum TGF-β level was very low at 658 pg/ml. The 1 wk level was fairly low as well at 3,585 pg/ml. The final infant to develop NEC did so at about 7 wk of life. That infant’s mother had a low colostrum TGF-β2 level of 1,793 pg/ml and also a low 1 wk level of 2,047 pg/ml.
Discussion
FI is a relatively common occurrence in the NICU, although few studies have sought to understand the epidemiology and contributing factors. In this study, 41% of very-low-birth-weight infants had FI, with the highest incidence seen in the smallest babies, as expected.
Previous studies have reported a wide variation in TGF-β breast milk levels in mothers of term infants (17), and our study confirms this finding for mothers of preterm infants. To date, the factors contributing to this variation are not well elucidated. In this cohort of lactating mothers of preterm infants, maternal breast milk TGF-β1 and TGF-β2 levels both decrease with advancing chronologic age, with colostrum containing the highest levels for both. Very few studies have sought to define the natural course for levels of TGF-β and other growth factors during lactation in preterm mothers. Castellote et al.(18), in a study of 42 lactating women, report similar findings to our study for TGF-β1 levels, but did not observe this decline for TGF-β2 levels in the milk from mothers of very preterm infants (defined as birth before 30 wk gestation in their study). Of note, our study is the largest report to date on mothers of preterm infants for whom TGF-β levels have been measured. Interestingly, the levels we report appear to be higher on average than that reported in studies of mothers of term infants. We did not have a term group for direct comparison, but we have recently analyzed a small cohort of term breast milk for TGF-β2. We found a median TGF-β2 level of 9,190 pg/ml (n = 5, range: 2,931–18,284 pg/ml) for term colostrum, which is not significantly different than the preterm results. However, mature milk had a median level of 1,880 pg/ml (n = 4, range: 444–4,245 pg/ml). This was of borderline significance (P = 0.05), but may have reached significance with a larger sample size. A separate study looking at TGF-β levels in 49 mothers of term infants reported what appears to be a lower mean TGF-β2 level in colostrum of 3,048 ± 339 pg/ml, with a range of 208–10,257 pg/ml (15).
In this group of mothers of preterm infants, we found a significant decrease in TGF-β1 colostrum levels with increasing birth weight and advancing gestational age; thus the highest levels of TGF-β1 were produced by mothers of the lowest-birth-weight and youngest infants. Although these high levels of TGF-β, particularly in colostrum, could possibly afford the preterm infant protection against excessive inflammation, emerging evidence indicates that most of the TGF-β in preterm milk exists in an inactive, latent state (19). We speculate that in utero inflammation associated with prematurity and low birth weight may trigger a counter-regulatory anti-inflammatory response that leads to increased maternal TGF-β production, but the at-risk preterm infant may not always be able to derive full advantage from milk-borne TGF-β because preterm milk is relatively deficient in the mechanisms that normally activate TGF-β in milk. Given that these infants are more susceptible to FI than the bigger and more mature full-term infants, as well as at greater risk for NEC, it is plausible that the protective effects of milk-borne TGF-β would be most evident in the smallest babies. It may be worth deciphering whether there is a feto-maternal signaling mechanism that may underlie this developmental change, and whether such signaling could be exploited for a therapeutic or preventive approach for NEC.
Evidence supports TGF-β playing a multifaceted role in the gastrointestinal tract. In animal and human studies, TGF-β has been shown to play a major role in the noninflammatory differentiation of gut macrophages (20), in establishing oral tolerance to dietary antigens (21), in stimulation of B-cell isotype switching to IgA (22), in strengthening the intestinal barrier (23), and in modulating inflammation (24,25,26,27), thus helping to maintain intestinal homeostasis.
Although little is known about the relationship of TGF-β to FI and NEC, Maheshwari et al. (11) recently demonstrated that TGF-β2 expression and bioactivity positively correlates with gestational age and that it is decreased in intestinal tissue from infants affected by NEC. This positive correlation of intestinal TGF-β with fetal maturity, together with our findings that maternal milk TGF-β levels negatively correlate with fetal maturity suggest that milk-derived TGF-β may be an evolutionarily developed protective factor to aid intestinal maturation in case of premature birth. Such protection may not be necessary once intestinal production of TGF-β becomes sufficient. Intriguingly, another milk-derived protective peptide, platelet-activating factor acetylhydrolase (PAF-AH; PLA2G7), exhibits a similar developmental pattern. Serum PAF-AH levels of neonates positively correlate with maturity (28), whereas milk PAF-AH levels, at least between 30 and 39 wk of gestation, negatively correlate with maturity (29).
Although this evidence is still emerging, recent studies have found a relationship between maternal breast milk TGF-β levels and infant allergy and atopy. In a recent meta-analysis by Oddy and Rosales (30), the authors review several of these studies, concluding that TGF-β in human breast milk appears to afford some protection against development of atopy and eczema. Rigotti et al. (31) reported that TGF-β levels were significantly lower in the breast milk of allergic mothers compared with nonallergic mothers. Furthermore, infants of the allergic mothers were themselves allergic 46% of the time, vs. none of the infants whose mothers did not have allergies. A separate study looked at a group of infants at high risk for the development of atopy, and found that in those infants who developed atopy earlier (i.e., during breastfeeding), maternal colostrum TGF-β levels were significantly lower (32). Finally, Oddy et al. (33) compared breast milk TGF-β dose (using levels and duration of breastfeeding) with development of wheeze by 1 y of age, and found a significant linear relationship, with highest dose of maternal breast milk TGF-β correlating with lowest incidence of wheezing in infants by 1 y.
Given the expected entero-protective role for TGF-β, we expected to find a decreased incidence of FI being associated with high maternal milk TGF-β levels. Surprisingly, we found that TGF-β1 colostrum levels were actually significantly higher in the FI group than the non-FI group, but this relationship was no longer significant after multivariable adjustment. We did not observe a difference in any other TGF-β isoform at any of the three time points when comparing those infants with FI and those without, even when controlling for birth weight or gestational age. Our study was limited to only 41 infants with FI. Perhaps a larger study would have enough power to detect a difference with regard to FI and maternal breast milk TGF-β levels. Of interest, we recently published a separate study in which we report that although there is indeed a large pool of TGF-β in preterm breast milk, the majority is latent, and preterm infants may be deficient in their ability to activate TGF-β to the bioactive form (19).
Intriguingly, although only five infants in our study developed NEC, most of the mothers of these infants had low TGF-β2 levels in colostrum and 1 wk milk samples. This observation merits future study to further explore the potential protective effect of TGF-β2 in maternal breast milk.
With respect to our secondary outcomes, we found that infants with FI took more time to reach full enteral feedings, consistent with our expectations. We did not find any other significant differences with the exception of 1 mo TGF-β1 levels and time to regain birth weight. However, as preterm infants generally regain birth weight prior to 1 mo of age, this finding is likely due to chance, and is not clinically meaningful.
Interestingly, we did find a difference in TGF-β2 levels in growth-restricted infants. Unfortunately, we were limited by the small number of babies in this subgroup of our cohort, which limits the power of this finding. However, the neonatal literature suggests that growth restriction in preterm infants contributes to an increased risk of NEC (34,35). In our cohort of preterm infants, low milk-borne TGF-β2 levels were strongly associated with FI within the subgroup of growth-restricted infants. One plausible explanation could relate to endogenous TGF-β production and TGF-β receptor expression in the preterm intestine. The gestational age for the IUGR group of infants was more than 2 wk older than the normally grown group of infants (mean 29.5 wk IUGR vs. 27.2 wk normally grown, P < 0.01). Animal studies suggest that endogenous TGF-β production is low in the preterm porcine intestine, and that TGF-β receptor density is developmentally regulated as well (36). However, this study also indicated that responsiveness of the receptor in the preterm gut may be less than the more mature intestinal receptor. Similarly, TGF-β levels in the human intestine are positively correlated with GA (11), yet there is no information to date on levels in growth-restricted infants. We speculate that growth restriction may alter the normal developmental process for TGF-β and its receptor; thus maternal breast-milk-derived TGF-β plays a greater role in FI. Interestingly, epidermal growth factor (6) levels are also lower in the breast milk of mothers who delivered preterm infants with growth restriction, compared with normally grown counterparts, although FI was not evaluated in that study (37).
Our study does have several limitations. We did not use a contemporaneous control term group for comparison. We did, however, analyze a small sample of term breast milk following our study, as reported above. In addition, our study was not powered to detect a difference in TGF-β levels for infants with and without NEC, but based on the TGF-β values we found in the breast milk samples of mothers whose infants developed NEC, this may be an area for future research.
Conclusions
To our knowledge, this study is the largest report of preterm maternal breast milk TGF-β levels to date. Maternal breast milk TGF-β levels decrease with advancing chronologic age for both isoforms, and colostrum level correlates inversely with birth weight and gestational age for TGF-β1. Although TGF-β does not protect preterm infants from FI, certain subgroups of infants, such as those with IUGR, may benefit from higher levels of TGF-β2. This subgroup, in particular, merits further study, as growth-restricted infants are at higher risk for FI and have previously been shown to be at higher risk for NEC. While few infants in our study developed NEC, their mothers’ breast milk TGF-β2 levels were often low, and future study is warranted to further evaluate this observation.
Methods
Study Design
We conducted a prospective analysis on mothers and babies admitted to our infant special care unit, at NorthShore University HealthSystem (previously Evanston Northwestern Healthcare), in Evanston, IL, between October 2008 and September 2010. Mother–infant pairs were eligible for enrollment if delivery occurred between 23 0/7 and 31 6/7 wk, the infant’s birth weight was less than 1,500 g, and the mother intended to provide expressed breast milk (EBM) for her infant. Mother–infant pairs were excluded from enrollment if the infant had a known gastrointestinal anomaly or had experienced birth asphyxia, as these infants would be at higher risk for NEC. The NorthShore University HealthSystem (formerly Evanston Northwestern Healthcare) Institutional Review Board approved this study, and signed informed consent was obtained from each mother before study entry.
Collection of Data
Infant charts were reviewed daily and demographic and outcome information was collected. The primary outcome of FI was defined as prefeeding gastric residuals of greater than 30% of the prior feed’s volume, bilious residuals, emesis, and/or abdominal distention considered significant enough by the managing physician to require cessation of feeds for at least 12 h, with normal radiograph findings or mild dilation of the bowel loops. One infant was not able to be categorized as he had a complicated spontaneous bowel perforation that precluded feeding for many weeks. IUGR was defined as a birth weight below the 10th percentile for gestational age. NEC was diagnosed based on clinical criteria along with radiographic evidence according to the criteria of Bell et al. (4).
TGF-β in Colostrum and Mature Milk
Once consent was obtained, we prospectively collected samples of EBM. These samples were obtained at three time points: the first was obtained within the first 48 h (colostrum), the second at 6–7 d of life (1 wk), and the third at 30–31 d of life (1 mo). These samples were then stored at −80 °C for batched analysis using an ELISA assay to measure TGF-β1 and TGF-β2 levels as described below.
Prior to detection of TGF-β levels with ELISA, colostrum and milk samples were centrifuged at 10,000g for 10 min in order to separate fat. Samples from the aqueous phase were then activated with 1 N HCl, and neutralized with 1.2 N NaOH/0.5 M N-2-hydroxyethylpiperazine-N9-2-ethanesulfonic acid. Samples were then diluted in calibrator diluent when indicated. Using a commercial quantitative sandwich enzyme immunoassay technique (R&D Systems, Minneapolis, MN), levels of TGF-β1 and TGF-β2 were measured according to the manufacturer’s instructions.
Statistical Analysis
Infant characteristics, TGF-β levels, and outcomes were compared between FI and no FI patients. Categorical variables were analyzed using chi-square and Fisher’s exact tests. Continuous variables were analyzed using t-tests or Wilcoxon–Mann–Whitney (nonparametric) tests. Variables with distributions that deviated from normality were reported by median and interquartile range (Q1, Q3) rather than conventional mean ± SD statistics. Since TGF-β levels were not normally distributed, box plots are presented to display their distributions and they were log transformed for the purpose of analyses. Differences across time points for TGF-βs were calculated using one-way repeated measures ANOVA. Correlations between TGF-β levels and characteristics were computed using Pearson and Spearman correlation coefficients. TGF-β level changes over time were not significant, so two levels were chosen for inclusion in a multivariable model to predict FI. Colostrum TGF-β1 and week 1 TGF-β2, as well as infant characteristics, and significant interactions, were included in a multivariable logistic regression model using generalized estimating equations. Statistical significance was established at an α level of 0.05. All statistical analyses were performed using SAS 9.3 statistical software (SAS Inc., Cary, NC).
Statement of Financial Support
All phases of this study were supported by the Gerber Foundation. A.M. is supported by National Institutes of Health (NIH, Bethesda, MD, USA) grant R01HD059142. The remaining authors have no financial disclosures.
Disclosure
The authors have no conflict of interest to disclose.
References
Mihatsch WA, von Schoenaich P, Fahnenstich H, et al. The significance of gastric residuals in the early enteral feeding advancement of extremely low birth weight infants. Pediatrics 2002;109:457–9.
Lucchini R, Bizzarri B, Giampietro S, De Curtis M . Feeding intolerance in preterm infants. How to understand the warning signs. J Matern Fetal Neonatal Med 2011;24:Suppl 1:72–4.
Moore TA, Wilson ME, Schmid KK, Anderson-Berry A, French JA, Berger AM . Relations between feeding intolerance and stress biomarkers in preterm infants. J Pediatr Gastroenterol Nutr 2013;57:356–62.
Bell MJ, Ternberg JL, Feigin RD, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg 1978;187:1–7.
Lucas A, Cole TJ . Breast milk and neonatal necrotising enterocolitis. Lancet 1990;336:1519–23.
Siegfried MR, Ma XL, Lefer AM . Splanchnic vascular endothelial dysfunction in rat endotoxemia: role of superoxide radicals. Eur J Pharmacol 1992;212:171–6.
Dvorak B, Halpern MD, Holubec H, et al. Epidermal growth factor reduces the development of necrotizing enterocolitis in a neonatal rat model. Am J Physiol Gastrointest Liver Physiol 2002;282:G156–64.
Feng J, El-Assal ON, Besner GE . Heparin-binding epidermal growth factor-like growth factor reduces intestinal apoptosis in neonatal rats with necrotizing enterocolitis. J Pediatr Surg 2006;41:742–7; discussion 742–7.
Ledbetter DJ, Juul SE . Erythropoietin and the incidence of necrotizing enterocolitis in infants with very low birth weight. J Pediatr Surg 2000;35:178–81; discussion 182.
Lu J, Jilling T, Li D, Caplan MS . Polyunsaturated fatty acid supplementation alters proinflammatory gene expression and reduces the incidence of necrotizing enterocolitis in a neonatal rat model. Pediatr Res 2007;61:427–32.
Maheshwari A, Kelly DR, Nicola T, et al. TGF-β2 suppresses macrophage cytokine production and mucosal inflammatory responses in the developing intestine. Gastroenterology 2011;140:242–53.
Massagué J . The transforming growth factor-beta family. Annu Rev Cell Biol 1990;6:597–641.
Blobe GC, Schiemann WP, Lodish HF . Role of transforming growth factor beta in human disease. N Engl J Med 2000;342:1350–8.
Kulkarni AB, Huh CG, Becker D, et al. Transforming growth factor beta 1 null mutation in mice causes excessive inflammatory response and early death. Proc Natl Acad Sci USA 1993;90:770–4.
Hawkes JS, Bryan DL, James MJ, Gibson RA . Cytokines (IL-1beta, IL-6, TNF-alpha, TGF-beta1, and TGF-beta2) and prostaglandin E2 in human milk during the first three months postpartum. Pediatr Res 1999;46:194–9.
Böttcher MF, Jenmalm MC, Garofalo RP, Björkstén B . Cytokines in breast milk from allergic and nonallergic mothers. Pediatr Res 2000;47:157–62.
Agarwal S, Karmaus W, Davis S, Gangur V . Immune markers in breast milk and fetal and maternal body fluids: a systematic review of perinatal concentrations. J Hum Lact 2011;27:171–86.
Castellote C, Casillas R, Ramírez-Santana C, et al. Premature delivery influences the immunological composition of colostrum and transitional and mature human milk. J Nutr 2011;141:1181–7.
Namachivayam K, Blanco CL, Frost BL, et al. Preterm human milk contains a large pool of latent TGF-β, which can be activated by exogenous neuraminidase. Am J Physiol Gastrointest Liver Physiol 2013;304:G1055–65.
Smythies LE, Sellers M, Clements RH, et al. Human intestinal macrophages display profound inflammatory anergy despite avid phagocytic and bacteriocidal activity. J Clin Invest 2005;115:66–75.
Ando T, Hatsushika K, Wako M, et al. Orally administered TGF-beta is biologically active in the intestinal mucosa and enhances oral tolerance. J Allergy Clin Immunol 2007;120:916–23.
van Vlasselaer P, Punnonen J, de Vries JE . Transforming growth factor-beta directs IgA switching in human B cells. J Immunol 1992;148:2062–7.
Hering NA, Andres S, Fromm A, et al. Transforming growth factor-β, a whey protein component, strengthens the intestinal barrier by upregulating claudin-4 in HT-29/B6 cells. J Nutr 2011;141:783–9.
Schiffrin EJ, El Yousfi M, Faure M, et al. Milk casein-based diet containing TGF-beta controls the inflammatory reaction in the HLA-B27 transgenic rat model. JPEN J Parenter Enteral Nutr 2005;29:Suppl 4:S141–8; discussion S149–50, S184–8.
Penttila IA, Flesch IE, McCue AL, et al. Maternal milk regulation of cell infiltration and interleukin 18 in the intestine of suckling rat pups. Gut 2003;52:1579–86.
Ozawa T, Miyata M, Nishimura M, et al. Transforming growth factor-beta activity in commercially available pasteurized cow milk provides protection against inflammation in mice. J Nutr 2009;139:69–75.
Oz HS, Ray M, Chen TS, McClain CJ . Efficacy of a transforming growth factor beta 2 containing nutritional support formula in a murine model of inflammatory bowel disease. J Am Coll Nutr 2004;23:220–6.
Caplan M, Hsueh W, Kelly A, Donovan M . Serum PAF acetylhydrolase increases during neonatal maturation. Prostaglandins 1990;39:705–14.
Moya FR, Eguchi H, Zhao B, et al. Platelet-activating factor acetylhydrolase in term and preterm human milk: a preliminary report. J Pediatr Gastroenterol Nutr 1994;19:236–9.
Oddy WH, Rosales F . A systematic review of the importance of milk TGF-beta on immunological outcomes in the infant and young child. Pediatr Allergy Immunol 2010;21(1 Pt 1):47–59.
Rigotti E, Piacentini GL, Ress M, Pigozzi R, Boner AL, Peroni DG . Transforming growth factor-beta and interleukin-10 in breast milk and development of atopic diseases in infants. Clin Exp Allergy 2006;36:614–8.
Kalliomäki M, Ouwehand A, Arvilommi H, Kero P, Isolauri E . Transforming growth factor-beta in breast milk: a potential regulator of atopic disease at an early age. J Allergy Clin Immunol 1999;104:1251–7.
Oddy WH, Halonen M, Martinez FD, et al. TGF-beta in human milk is associated with wheeze in infancy. J Allergy Clin Immunol 2003;112:723–8.
Aucott SW, Donohue PK, Northington FJ . Increased morbidity in severe early intrauterine growth restriction. J Perinatol 2004;24:435–40.
Garite TJ, Clark R, Thorp JA . Intrauterine growth restriction increases morbidity and mortality among premature neonates. Am J Obstet Gynecol 2004;191:481–7.
Sangild PT, Mei J, Fowden AL, Xu RJ . The prenatal porcine intestine has low transforming growth factor-beta ligand and receptor density and shows reduced trophic response to enteral diets. Am J Physiol 2009;296:R1053–62.
Oslislo A, Czuba Z, Sławska H, Kaźmierczak W, Król W . Decreased human milk concentration of epidermal growth factor after preterm delivery of intrauterine growth-restricted newborns. J Pediatr Gastroenterol Nutr 2007;44:464–7.
Acknowledgements
We thank I. Sue Wolf, RNC-NIC, for her efforts in coordinating this research study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frost, B., Jilling, T., Lapin, B. et al. Maternal breast milk transforming growth factor-beta and feeding intolerance in preterm infants. Pediatr Res 76, 386–393 (2014). https://doi.org/10.1038/pr.2014.96
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2014.96