Key Points
-
Lead extraction procedures are becoming common owing to the growing number of implantations in an ageing population, frequent device infections, and lead recalls and malfunctions
-
The most common indication for lead extraction is infection
-
Lead extraction procedures need to be performed at specialized centres because major complications, such as perforation or avulsion, can occur
-
Manual mechanical dilatation sheaths or those powered mechanically or that use laser energy are safe methods of extraction
-
Lead management strategies should be a multidisciplinary, collaborative effort and include appropriate implantation techniques, infection prevention, and lead selection
Abstract
Extraction of cardiovascular implantable electronic device leads is the removal of a lead that has been implanted for >1 year or that requires more than a standard stylet. The number of these procedures has greatly increased over the past few decades owing to the growing demand for primary and secondary implantations in ageing populations, and an accompanying rise in revisions for complications, infections, and lead advisory safety alerts. In this Review, we present the most common indications and techniques used for extraction. Particular consideration is given to the extraction of leads with large vegetations, recalled leads, stented leads, and those placed in the coronary sinus. We also summarize the most relevant and contemporary data on safety, efficacy, and outcomes of lead extraction.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Wilkoff, B. L. et al. Transvenous lead extraction: Heart Rhythm Society expert consensus on facilities, training, indications, and patient management: this document was endorsed by the American Heart Association (AHA). Heart Rhythm 6, 1085–1104 (2009).
Hammill, S. C. et al. Review of the registry's fourth year, incorporating lead data and pediatric ICD procedures, and use as a national performance measure. Heart Rhythm 7, 1340–1345 (2010).
Hammill, S. C. et al. Review of the ICD Registry's third year, expansion to include lead data and pediatric ICD procedures, and role for measuring performance. Heart Rhythm 6, 1397–1401 (2009).
Hammill, S. C. et al. Review of the Registry's second year, data collected, and plans to add lead and pediatric ICD procedures. Heart Rhythm 5, 1359–1363 (2008).
Hammill, S., Phurrough, S. & Brindis, R. The National ICD Registry: now and into the future. Heart Rhythm 3, 470–473 (2006).
Cabell, C. H. et al. Increasing rates of cardiac device infections among Medicare beneficiaries: 1990–1999. Am. Heart J. 147, 582–586 (2004).
Voigt, A., Shalaby, A. & Saba, S. Rising rates of cardiac rhythm management device infections in the United States: 1996 through 2003. J. Am. Coll. Cardiol. 48, 590–591 (2006).
Gould, P. A. et al. Outcome of advisory implantable cardioverter-defibrillator replacement: one-year follow-up. Heart Rhythm 5, 1675–1681 (2008).
Klug, D. et al. Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: results of a large prospective study. Circulation 116, 1349–1355 (2007).
Krahn, A. D. et al. Outcome of the Fidelis implantable cardioverter-defibrillator lead advisory: a report from the Canadian Heart Rhythm Society Device Advisory Committee. Heart Rhythm 5, 639–642 (2008).
Krahn, A. D. et al. Utilization of a national network for rapid response to the Medtronic Fidelis lead advisory: the Canadian Heart Rhythm Society Device Advisory Committee. Heart Rhythm 6, 474–477 (2009).
Poole, J. E. et al. Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures: results from the REPLACE Registry. Circulation 122, 1553–1561 (2010).
Greenspon, A. J. et al. 16-year trends in the infection burden for pacemakers and implantable cardioverter-defibrillators in the United States 1993 to 2008. J. Am. Coll. Cardiol. 58, 1001–1006 (2011).
Byrd, C. L., Wilkoff, B. L., Love, C. J., Sellers, T. D. & Reiser, C. Clinical study of the laser sheath for lead extraction: the total experience in the United States. Pacing Clin. Electrophysiol. 25, 804–808 (2002).
Byrd, C. L. et al. Intravascular extraction of problematic or infected permanent pacemaker leads: 1994–1996. U.S. Extraction Database, MED Institute. Pacing Clin. Electrophysiol. 22, 1348–1357 (1999).
Maytin, M., Jones, S. O. & Epstein, L. M. Long-term mortality after transvenous lead extraction. Circ. Arrhythm. Electrophysiol. 5, 252–257 (2012).
Sohail, M. R. et al. Infective endocarditis complicating permanent pacemaker and implantable cardioverter-defibrillator infection. Mayo Clin. Proc. 83, 46–53 (2008).
Sohail, M. R. et al. Management and outcome of permanent pacemaker and implantable cardioverter-defibrillator infections. J. Am. Coll. Cardiol. 49, 1851–1859 (2007).
Tarakji, K. G. et al. Cardiac implantable electronic device infections: presentation, management, and patient outcomes. Heart Rhythm 7, 1043–1047 (2010).
Tarakji, K. G. et al. Risk factors for 1-year mortality among patients with cardiac implantable electronic device infection undergoing transvenous lead extraction: the impact of the infection type and the presence of vegetation on survival. Europace 16, 1490–1495 (2014).
Wazni, O. et al. Lead extraction in the contemporary setting: the LExICon study: an observational retrospective study of consecutive laser lead extractions. J. Am. Coll. Cardiol. 55, 579–586 (2010).
Klug, D. et al. Local symptoms at the site of pacemaker implantation indicate latent systemic infection. Heart 90, 882–886 (2004).
Noheria, A. et al. Pulmonary embolism in patients with transvenous cardiac implantable electronic device leads. Europace http://dx.doi.org/10.1093/europace/euv038 (2015).
Brunner, M. P. et al. Nomogram for predicting 30-day all-cause mortality after transvenous pacemaker and defibrillator lead extraction. Heart Rhythm 12, 2381–2386 (2015).
Le, K. Y. et al. Impact of timing of device removal on mortality in patients with cardiovascular implantable electronic device infections. Heart Rhythm 8, 1678–1685 (2011).
de Bie, M. K. et al. Cardiac device infections are associated with a significant mortality risk. Heart Rhythm 9, 494–498 (2012).
Knigina, L. et al. Treatment of patients with recurrent or persistent infection of cardiac implantable electronic devices. Europace 12, 1275–1281 (2010).
Sohail, M. R., Sultan, O. W. & Raza, S. S. Contemporary management of cardiovascular implantable electronic device infections. Expert Rev. Anti Infect. Ther. 8, 831–839 (2010).
Baddour, L. M. et al. Update on cardiovascular implantable electronic device infections and their management: a scientific statement from the American Heart Association. Circulation 121, 458–477 (2010).
Hauser, R. G. & Hayes, D. L. Increasing hazard of Sprint Fidelis implantable cardioverter-defibrillator lead failure. Heart Rhythm 6, 605–610 (2009).
Hauser, R. G., Kallinen, L. M., Almquist, A. K., Gornick, C. C. & Katsiyiannis, W. T. Early failure of a small-diameter high-voltage implantable cardioverter-defibrillator lead. Heart Rhythm 4, 892–896 (2007).
Hauser, R. G., McGriff, D. & Retel, L. K. Riata implantable cardioverter-defibrillator lead failure: analysis of explanted leads with a unique insulation defect. Heart Rhythm. 9, 472–749 (2012).
Kallinen, L. M. et al. Failure of impedance monitoring to prevent adverse clinical events caused by fracture of a recalled high-voltage implantable cardioverter-defibrillator lead. Heart Rhythm 5, 775–779 (2008).
Kleemann, T. et al. Annual rate of transvenous defibrillation lead defects in implantable cardioverter-defibrillators over a period of >10 years. Circulation 115, 2474–2480 (2007).
Hauser, R. G. Here we go again — another failure of postmarketing device surveillance. N. Engl. J. Med. 366, 873–875 (2012).
Heidbuchel, H. et al. Potential role of remote monitoring for scheduled and unscheduled evaluations of patients with an implantable defibrillator. Europace 10, 351–357 (2008).
Henrikson, C. A. The Sprint Fidelis story: where are we now? Heart Rhythm 6, 611–612 (2009).
Maytin, M. et al. Multicenter experience with extraction of the Sprint Fidelis implantable cardioverter-defibrillator lead. J. Am. Coll. Cardiol. 56, 646–650 (2010).
Neuzil, P., Taborsky, M., Holy, F. & Wallbrueck, K. Early automatic remote detection of combined lead insulation defect and ICD damage. Europace 10, 556–557 (2008).
Brunner, M. P. et al. Transvenous extraction of implantable cardioverter-defibrillator leads under advisory — a comparison of Riata, Sprint Fidelis, and non-recalled implantable cardioverter-defibrillator leads. Heart Rhythm 10, 1444–1450 (2013).
El-Chami, M. F. et al. Outcomes of Sprint Fidelis and Riata lead extraction: data from 2 high-volume centers. Heart Rhythm 12, 1216–1220 (2015).
Ellenbogen, K. A., Wood, M. A. & Swerdlow, C. D. The Sprint Fidelis lead fracture story: what do we really know and where do we go from here? Heart Rhythm 5, 1380–1381 (2008).
Farwell, D., Green, M. S., Lemery, R., Gollob, M. H. & Birnie, D. H. Accelerating risk of Fidelis lead fracture. Heart Rhythm 5, 1375–1379 (2008).
Epstein, A. E. et al. Performance of the St. Jude Medical Riata leads. Heart Rhythm 6, 204–209 (2009).
Henrikson, C. A. The Riata story — where are we now? Heart Rhythm. 9, 750–751 (2012).
Schmutz, M. et al. Prevalence of asymptomatic and electrically undetectable intracardiac inside-out abrasion in silicon-coated Riata® and Riata® ST implantable cardioverter-defibrillator leads. Int. J. Cardiol. 167, 254–257 (2013).
Zeitler, E. P. et al. Cable externalization and electrical failure of the Riata family of implantable cardioverter-defibrillator leads: a systematic review and meta-analysis. Heart Rhythm 12, 1233–1240 (2015).
Maytin, M. et al. Multicenter experience with extraction of the Riata/Riata ST ICD lead. Heart Rhythm 11, 1613–1618 (2014).
Bongiorni, M. G. et al. Transvenous extraction profile of Riata leads: procedural outcomes and technical complexity of mechanical removal. Heart Rhythm 12, 580–587 (2015).
Richardson, T. D. et al. Comparative outcomes of transvenous extraction of sprint fidelis and riata defibrillator leads: a single center experience. J. Cardiovasc. Electrophysiol. 25, 36–42 (2014).
Grazia Bongiorni, M. et al. Management of malfunctioning and recalled pacemaker and defibrillator leads: results of the European Heart Rhythm Association survey. Europace 16, 1674–1678 (2014).
Love, C. J. Update on indications, techniques, and complications of cardiac implantable device lead extraction. Curr. Treat. Options Cardiovasc. Med. 14, 565–570 (2012).
Worley, S. J., Gohn, D. C. & Pulliam, R. W. Over the wire lead extraction and focused force venoplasty to regain venous access in a totally occluded subclavian vein. J. Interv. Card. Electrophysiol. 23, 135–137 (2008).
Maytin, M., Epstein, L. M. & Henrikson, C. A. Lead extraction is preferred for lead revisions and system upgrades: when less is more. Circ. Arrhythm. Electrophysiol. 3, 413–424 (2010).
Borek, P. P. & Wilkoff, B. L. Pacemaker and ICD leads: strategies for long-term management. J. Interv. Card. Electrophysiol. 23, 59–72 (2008).
Bracke, F. A. Yes we can! But should we? Lead extraction for superfluous pacemaker and implanted cardioverter-defibrillator leads. Europace 11, 546–547 (2009).
Korley, V. J., Hallet, N., Daoust, M. & Epstein, L. M. A novel indication for transvenous lead extraction: upgrading implantable cardioverter defibrillator systems. J. Interv. Card. Electrophysiol. 4, 523–528 (2000).
Bracke, F. A., van Gelder, L. M., Sreeram, N. & Meijer, A. Exchange of pacing or defibrillator leads following laser sheath extraction of non-functional leads in patients with ipsilateral obstructed venous access. Heart 83, E12 (2000).
Levine, P. A. Should lead explantation be the practice standard when a lead needs to be replaced? Pacing Clin. Electrophysiol. 23, 421–422 (2000).
Gula, L. J. et al. Central venous occlusion is not an obstacle to device upgrade with the assistance of laser extraction. Pacing Clin. Electrophysiol. 28, 661–666 (2005).
Suga, C., Hayes, D. L., Hyberger, L. K. & Lloyd, M. A. Is there an adverse outcome from abandoned pacing leads? J. Interv. Card. Electrophysiol. 4, 493–499 (2000).
Furman, S., Behrens, M., Andrews, C. & Klementowicz, P. Retained pacemaker leads. J. Thorac Cardiovasc. Surg. 94, 770–772 (1987).
Bohm, A. et al. Complications due to abandoned noninfected pacemaker leads. Pacing Clin. Electrophysiol. 24, 1721–1724 (2001).
de Cock, C. C., Vinkers, M., Van Campe, L. C., Verhorst, P. M. & Visser, C. A. Long-term outcome of patients with multiple (> or = 3) noninfected transvenous leads: a clinical and echocardiographic study. Pacing Clin. Electrophysiol. 23, 423–426 (2000).
Wollmann, C. G. et al. Incidence of complications in patients with implantable cardioverter/defibrillator who receive additional transvenous pace/sense leads. Pacing Clin. Electrophysiol. 28, 795–800 (2005).
Glikson, M. et al. Do abandoned leads pose risk to implantable cardioverter-defibrillator patients? Heart Rhythm 6, 65–68 (2009).
Huang, X. M. et al. Extraction of superfluous device leads: a comparison with removal of infected leads. Heart Rhythm 12, 1177–1182 (2015).
Huang, T. Y. & Baba, N. Cardiac pathology of transvenous pacemakers. Am. Heart J. 83, 469–474 (1972).
Rennert, R. C. et al. A histological and mechanical analysis of the cardiac lead-tissue interface: implications for lead extraction. Acta Biomater. 10, 2200–2208 (2014).
Epstein, A. E., Kay, G. N., Plumb, V. J., Dailey, S. M. & Anderson, P. G. Gross and microscopic pathological changes associated with nonthoracotomy implantable defibrillator leads. Circulation 98, 1517–1524 (1998).
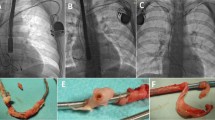
Bongiorni, M. G. et al. Usefulness of mechanical transvenous dilation and location of areas of adherence in patients undergoing coronary sinus lead extraction. Europace 9, 69–73 (2007).
Bongiorni, M. G. et al. Safety and efficacy of internal transjugular approach for transvenous extraction of implantable cardioverter defibrillator leads. Europace 16, 1356–1362 (2014).
Smith, H. J. et al. Five-years experience with intravascular lead extraction. Pacing Clin. Electrophysiol. 17, 2016–2020 (1994).
Segreti, L. et al. Major predictors of fibrous adherences in transvenous implantable cardioverter-defibrillator lead extraction. Heart Rhythm 11, 2196–2201 (2014).
Brunner, M. P. et al. Outcomes of patients requiring emergent surgical or endovascular intervention for catastrophic complications during transvenous lead extraction. Heart Rhythm 11, 419–425 (2014).
Patel, N. et al. Vacuum assisted vegetation extraction for the management of large lead vegetations. J. Card. Surg. 28, 321–324 (2013).
Vaccarino, G. N. et al. Pacemaker endocarditis: approach for lead extraction in endocarditis with large vegetations. Rev. Bras. Cir. Cardiovasc. 24, 570–573 (2009).
Ruttmann, E. et al. Transvenous pacemaker lead removal is safe and effective even in large vegetations: an analysis of 53 cases of pacemaker lead endocarditis. Pacing Clin. Electrophysiol. 29, 231–236 (2006).
Wilkoff, B. L. et al. Improved extraction of ePTFE and medical adhesive modified defibrillation leads from the coronary sinus and great cardiac vein. Pacing Clin. Electrophysiol. 28, 205–211 (2005).
Malecka, B., Kutarski, A. & Grabowski, M. Is the transvenous extraction of cardioverter-defibrillator leads more hazardous than that of pacemaker leads? Kardiol. Pol. 68, 884–890 (2010).
Saad, E. B. et al. Nonthoracotomy implantable defibrillator lead extraction: results and comparison with extraction of pacemaker leads. Pacing Clin. Electrophysiol. 26, 1944–1950 (2003).
Epstein, L. M. et al. Superior vena cava defibrillator coils make transvenous lead extraction more challenging and riskier. J. Am. Coll. Cardiol. 61, 987–989 (2013).
Di Cori, A. et al. Transvenous extraction performance of expanded polytetrafluoroethylene covered ICD leads in comparison to traditional ICD leads in humans. Pacing Clin. Electrophysiol. 33, 1376–1381 (2010).
Hackler, J. W. et al. Effectiveness of implantable cardioverter-defibrillator lead coil treatments in facilitating ease of extraction. Heart Rhythm 7, 890–897 (2010).
di Cori, A. et al. Large, single-center experience in transvenous coronary sinus lead extraction: procedural outcomes and predictors for mechanical dilatation. Pacing Clin. Electrophysiol. 35, 215–222 (2012).
Moynahan, M., Duggirala, H., Dwyer, D. & Fellman, M. FDA approved the Medtronic model 4195 Attain Starfix coronary sinus lead. Heart Rhythm 7, e3–e4 (2010).
Baranowski, B., Yerkey, M., Dresing, T. & Wilkoff, B. L. Fibrotic tissue growth into the extendable lobes of an active fixation coronary sinus lead can complicate extraction. Pacing Clin. Electrophysiol. 34, e64–e65 (2011).
Cronin, E. M. et al. Active fixation mechanism complicates coronary sinus lead extraction and limits subsequent reimplantation targets. J. Interv. Card. Electrophysiol. 36, 81–86 (2013).
Maytin, M. et al. Multicenter experience with transvenous lead extraction of active fixation coronary sinus leads. Pacing Clin. Electrophysiol. 35, 641–647 (2012).
Bontempi, L. et al. Extraction of a coronary sinus lead: always so easy? J. Cardiovasc. Med. (Hagerstown) http://dx.doi.org/10.2459/JCM.0000000000000018 (2014).
Kypta, A., Honig, S. & Steinwender, C. Removal of a chronically implanted active-fixation coronary sinus pacing lead using the Cook Evolution© lead extraction sheath. Europace 16, 625 (2014).
Lisy, M. et al. Coronary sinus lead extraction in CRT patients with CIED-related infection: risks, implications and outcomes. Minerva Cardioangiol. 63, 91–98 (2015).
Tyers, G. F., Clark, J., Wang, Y., Mills, P. & Bashir, J. Coronary sinus lead extraction. Pacing Clin. Electrophysiol. 26, 524–526 (2003).
Baranowski, B. et al. Percutaneous extraction of stented device leads. Heart Rhythm 9, 723–727 (2012).
Bongiorni, M. G. et al. Transvenous removal of pacing and implantable cardiac defibrillating leads using single sheath mechanical dilatation and multiple venous approaches: high success rate and safety in more than 2000 leads. Eur. Heart J. 29, 2886–2893 (2008).
Author information
Authors and Affiliations
Contributions
Both authors researched data for the article, discussed its content, and wrote, reviewed, and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
O.W. and B.L.W. have received honoraria from Spectranetics.
Rights and permissions
About this article
Cite this article
Wazni, O., Wilkoff, B. Considerations for cardiac device lead extraction. Nat Rev Cardiol 13, 221–229 (2016). https://doi.org/10.1038/nrcardio.2015.207
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2015.207
This article is cited by
-
Stepwise transvenous lead extraction due to pacemaker pocket infection following lactational mastitis complicated with breast abscess
International Breastfeeding Journal (2024)
-
Antegrade approach for peripheral intravascular lithotripsy pretreatment to facilitate laser lead extraction
Journal of Interventional Cardiac Electrophysiology (2023)
-
Negative-pressure wound therapy (NPWT) for the treatment of pacemaker pocket infection in patients unable or unwilling to undergo CIED extraction
Journal of Interventional Cardiac Electrophysiology (2021)
-
Comparing the safety of subcutaneous versus transvenous ICDs: a meta-analysis
Journal of Interventional Cardiac Electrophysiology (2021)
-
Effect of Applied Potential on Fatigue Life of Electropolished Nitinol Wires
Shape Memory and Superelasticity (2017)