Key Points
-
Diffuse high-grade gliomas (HGGs) carry a dismal prognosis in both children and adults; however, genome-wide molecular analyses have shown that the disease pathogenesis differs significantly between these age groups.
-
There are at least several distinct subgroups of paediatric diffuse HGG based on clinical features and recurrent mutations.
-
Diffuse intrinsic pontine gliomas (DIPGs) arise in the brainstem, occur almost exclusively in children and are incurable.
-
Aberrant epigenetic regulation has an important role in paediatric HGGs, with 'hotspot' K27M histone H3 mutations found in nearly 80% of DIPGs, and alternative G34R or G34V mutations found in paediatric HGGs of the cerebral hemispheres.
-
Recurrent mutations of the bone morphogenetic protein (BMP) receptor activin receptor type 1 (ACVR1; also known as ALK2) are restricted to the youngest patients with DIPG, highlighting crucial connections between development and gliomagenesis.
-
HGGs in children who are less than three years of age contain very few genomic abnormalities and recurrent gene fusions, and have a better outcome than HGGs in older children.
-
An improved understanding of the oncogenic mutations driving paediatric diffuse HGG has identified new potential therapeutic targets and shown that different strategies will be needed to combat this disease in children and adults.
Abstract
Diffuse high-grade gliomas (HGGs) of childhood are a devastating spectrum of disease with no effective cures. The two-year survival for paediatric HGG ranges from 30%, for tumours arising in the cerebral cortex, to less than 10% for diffuse intrinsic pontine gliomas (DIPGs), which arise in the brainstem. Recent genome-wide studies provided abundant evidence that unique selective pressures drive HGG in children compared to adults, identifying novel oncogenic mutations connecting tumorigenesis and chromatin regulation, as well as developmental signalling pathways. These new genetic findings give insights into disease pathogenesis and the challenges and opportunities for improving patient survival in these mostly incurable childhood brain tumours.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Ostrom, Q. T. et al. CBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in the United States in 2006–2010. Neuro Oncol. 15 (Suppl 2), ii1–ii56 (2013).
Jones, C., Perryman, L. & Hargrave, D. Paediatric and adult malignant glioma: close relatives or distant cousins? Nature Rev. Clin. Oncol. 9, 400–413 (2012).
Kramm, C. M. et al. Thalamic high-grade gliomas in children: a distinct clinical subset? Neuro Oncol. 13, 680–689 (2011).
Wolff, B. et al. Pediatric high grade glioma of the spinal cord: results of the HIT-GBM database. J. Neurooncol. 107, 139–146 (2012).
Karremann, M. et al. Cerebellar location may predict an unfavourable prognosis in paediatric high-grade glioma. Br. J. Cancer 109, 844–851 (2013).
Warren, K. E. Diffuse intrinsic pontine glioma: poised for progress. Front. Oncol. 2, 205 (2012).
Hargrave, D., Bartels, U. & Bouffet, E. Diffuse brainstem glioma in children: critical review of clinical trials. Lancet Oncol. 7, 241–248 (2006).
Roujeau, T. et al. Stereotactic biopsy of diffuse pontine lesions in children. J. Neurosurg. 107, 1–4 (2007). This paper provides evidence for the safety of routine biopsy procedures in children with DIPG.
Broniscer, A. et al. Prospective collection of tissue samples at autopsy in children with diffuse intrinsic pontine glioma. Cancer 116, 4632–4637 (2010).
Angelini, P., Hawkins, C., Laperriere, N., Bouffet, E. & Bartels, U. Post mortem examinations in diffuse intrinsic pontine glioma: challenges and chances. J. Neurooncol. 101, 75–81 (2011). References 9 and 10 report the feasibility of collecting DIPG tissue and autopsy and the quality of nucleic acids from autopsy samples for research.
Monje, M. et al. Hedgehog-responsive candidate cell of origin for diffuse intrinsic pontine glioma. Proc. Natl Acad. Sci. USA 108, 4453–4458 (2011).
Qaddoumi, I., Sultan, I. & Gajjar, A. Outcome and prognostic features in pediatric gliomas: a review of 6212 cases from the Surveillance, Epidemiology, and End Results database. Cancer 115, 5761–5770 (2009).
WHO Classification of Tumours of the Central Nervous System (eds Louis, D. N., Ohgaki, H., Wiestler, O. D. & Cavenee, W. K.) (World Health Organisation, 2007).
Phillips, H. S. et al. Molecular subclasses of high-grade glioma predict prognosis, delineate a pattern of disease progression, and resemble stages in neurogenesis. Cancer Cell 9, 157–173 (2006). This paper defines gene expression subgroups associated with survival of adult patients with HGG. The same subgroups can be identified in pHGG.
Paugh, B. S. et al. Genome-wide analyses identify recurrent amplifications of receptor tyrosine kinases and cell-cycle regulatory genes in diffuse intrinsic pontine glioma. J. Clin. Oncol. 29, 3999–4006 (2011).
Paugh, B. S. et al. Integrated molecular genetic profiling of pediatric high-grade gliomas reveals key differences with the adult disease. J. Clin. Oncol. 28, 3061–3068 (2010).
Bjerke, L. et al. Histone H3.3 mutations drive pediatric glioblastoma through upregulation of MYCN. Cancer Discov. 3, 512–519 (2013). This is the first study to evaluate the association of H3F3A G34 mutation on the genomic distribution of H3K36me3 marks.
Sturm, D. et al. Paediatric and adult glioblastoma: multiform (epi)genomic culprits emerge. Nature Rev. Cancer 14, 92–107 (2014).
Buczkowicz, P. et al. Genomic analysis of diffuse intrinsic pontine gliomas identifies three molecular subgroups and recurrent activating ACVR1 mutations. Nature Genet. 46, 451–456 (2014).
Fontebasso, A. M. et al. Recurrent somatic mutations in ACVR1 in pediatric midline high- grade astrocytoma. Nature Genet. 46, 462–466 (2014). This study analysed DIPGs, and thalamic and cortical HGGs and showed FGFR mutations in midline HGGs.
Taylor, K. R. et al. Recurrent activating ACVR1 mutations in diffuse intrinsic pontine glioma. Nature Genet. 46, 457–461 (2014).
Wu, G. et al. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nature Genet. 46, 444–450 (2014). References 19–22 reported recurrent mutations in ACVR1 , exclusively in DIPG, and they provided genome-wide data to define the somatic mutation landscape of DIPG. Reference 22 also identified NTRK fusion genes in infant gliomas, and germline mutations in DNA mismatch repair genes in paediatric HGGs with minimal CNAs.
Schwartzentruber, J. et al. Driver mutations in histone H3.3 and chromatin remodelling genes in paediatric glioblastoma. Nature 482, 226–231 (2012). This paper is the first genome-wide sequence analysis of paediatric glioblastoma.
Bax, D. A. et al. A distinct spectrum of copy number aberrations in pediatric high-grade gliomas. Clin. Cancer Res. 16, 3368–3377 (2010).
Puget, S. et al. Mesenchymal transition and PDGFRA amplification/mutation are key distinct oncogenic events in pediatric diffuse intrinsic pontine gliomas. PLoS ONE 7, e30313 (2012).
Qu, H. Q. et al. Genome-wide profiling using single-nucleotide polymorphism arrays identifies novel chromosomal imbalances in pediatric glioblastomas. Neuro Oncol. 12, 153–163 (2010).
Zarghooni, M. et al. Whole-genome profiling of pediatric diffuse intrinsic pontine gliomas highlights platelet-derived growth factor receptor α and poly (ADP-ribose) polymerase as potential therapeutic targets. J. Clin. Oncol. 28, 1337–1344 (2010).
Barrow, J. et al. Homozygous loss of ADAM3A revealed by genome-wide analysis of pediatric high-grade glioma and diffuse intrinsic pontine gliomas. Neuro Oncol. 13, 212–222 (2011).
Kyritsis, A. P., Bondy, M. L., Rao, J. S. & Sioka, C. Inherited predisposition to glioma. Neuro Oncol. 12, 104–113 (2010).
Eguchi, M. et al. Fusion of ETV6 to neurotrophin-3 receptor TRKC in acute myeloid leukemia with t(12;15)(p13;q25). Blood 93, 1355–1363 (1999).
Lannon, C. L. & Sorensen, P. H. ETV6-NTRK3: a chimeric protein tyrosine kinase with transformation activity in multiple cell lineages. Semin. Cancer Biol. 15, 215–223 (2005).
Li, Z. et al. ETV6-NTRK3 fusion oncogene initiates breast cancer from committed mammary progenitors via activation of AP1 complex. Cancer Cell 12, 542–558 (2007).
Knezevich, S. R. et al. ETV6-NTRK3 gene fusions and trisomy 11 establish a histogenetic link between mesoblastic nephroma and congenital fibrosarcoma. Cancer Res. 58, 5046–5048 (1998).
Butti, M. G. et al. A sequence analysis of the genomic regions involved in the rearrangements between TPM3 and NTRK1 genes producing TRK oncogenes in papillary thyroid carcinomas. Genomics 28, 15–24 (1995).
Zhang, J. et al. Whole-genome sequencing identifies genetic alterations in pediatric low-grade gliomas. Nature Genet. 45, 602–612 (2013).
Jones, D. T. et al. Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. Nature Genet. 45, 927–932 (2013).
Frattini, V. et al. The integrated landscape of driver genomic alterations in glioblastoma. Nature Genet. 45, 1141–1149 (2013).
The Cancer Genome Atlas Research Network. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455, 1061–1068 (2008).
Parsons, D. W. et al. An integrated genomic analysis of human glioblastoma multiforme. Science 321, 1807–1812 (2008). References 38 and 39 are the first reports of the almost universal involvement of mutations in the RTK–RAS–PI3K, p53 and RB signalling pathways in adult glioblastoma. Reference 38 used selective sequencing of candidate genes. Reference 39 was the first whole-exome analysis of glioblastoma, and identified IDH1 mutations, thus providing molecular evidence for distinct aetiologies between primary and secondary glioblastomas.
Schiffman, J. D. et al. Oncogenic BRAF mutation with CDKN2A inactivation is characteristic of a subset of pediatric malignant astrocytomas. Cancer Res. 70, 512–519 (2010). This is the first identification of BRAFV600E mutations in pHGGs.
Nicolaides, T. P. et al. Targeted therapy for BRAFV600E malignant astrocytoma. Clin. Cancer Res. 17, 7595–7604 (2011).
Bautista, F. et al. Vemurafenib in pediatric patients with BRAFV600E mutated high-grade gliomas. Pediatr. Blood Cancer 61, 1101–1103 (2014).
Huillard, E. et al. Cooperative interactions of BRAFV600E kinase and CDKN2A locus deficiency in pediatric malignant astrocytoma as a basis for rational therapy. Proc. Natl Acad. Sci. USA 109, 8710–8715 (2012).
Schindler, G. et al. Analysis of BRAF V600E mutation in 1,320 nervous system tumors reveals high mutation frequencies in pleomorphic xanthoastrocytoma, ganglioglioma and extra-cerebellar pilocytic astrocytoma. Acta Neuropathol. 121, 397–405 (2011).
Paugh, B. S. et al. Novel oncogenic PDGFRA mutations in pediatric high-grade gliomas. Cancer Res. 73, 6219–6229 (2013).
Snuderl, M. et al. Mosaic amplification of multiple receptor tyrosine kinase genes in glioblastoma. Cancer Cell 20, 810–817 (2011).
Szerlip, N. J. et al. Intratumoral heterogeneity of receptor tyrosine kinases EGFR and PDGFRA amplification in glioblastoma defines subpopulations with distinct growth factor response. Proc. Natl Acad. Sci. USA 109, 3041–3046 (2012).
Little, S. E. et al. Receptor tyrosine kinase genes amplified in glioblastoma exhibit a mutual exclusivity in variable proportions reflective of individual tumor heterogeneity. Cancer Res. 72, 1614–1620 (2012).
Barton, K. L. et al. PD-0332991, a CDK4/6 inhibitor, significantly prolongs survival in a genetically engineered mouse model of brainstem glioma. PLoS ONE 8, e77639 (2013).
Wu, G. et al. Somatic histone H3 alterations in pediatric diffuse intrinsic pontine gliomas and non-brainstem glioblastomas. Nature Genet. 44, 251–253 (2012). References 23 and 50 report the co-discovery of the first histone mutations in human cancer, and the identification of histone H3 mutations in paediatric glioblastoma. Reference 50 was the first to report histone H3 mutations in DIPG, with the frequency of mutation providing strong evidence for distinct pathogenesis of DIPG.
Yuen, B. T. & Knoepfler, P. S. Histone h3.3 mutations: a variant path to cancer. Cancer Cell 24, 567–574 (2013).
Maze, I., Noh, K. M., Soshnev, A. A. & Allis, C. D. Every amino acid matters: essential contributions of histone variants to mammalian development and disease. Nature Rev. Genet. 15, 259–271 (2014).
Elsaesser, S. J., Goldberg, A. D. & Allis, C. D. New functions for an old variant: no substitute for histone H3.3. Curr. Opin. Genet. Dev. 20, 110–117 (2010).
Skene, P. J. & Henikoff, S. Histone variants in pluripotency and disease. Development 140, 2513–2524 (2013).
Khuong-Quang, D. A. et al. K27M mutation in histone H3.3 defines clinically and biologically distinct subgroups of pediatric diffuse intrinsic pontine gliomas. Acta Neuropathol. 124, 439–447 (2012).
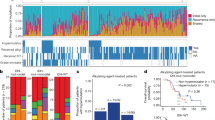
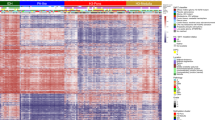
Sturm, D. et al. Hotspot mutations in H3F3A and IDH1 define distinct epigenetic and biological subgroups of glioblastoma. Cancer Cell 22, 425–437 (2012). This study identified the association of genome-wide DNA methylation signatures with histone H3 mutation status and corresponding transcriptional regulation of developmentally associated genes.
Fontebasso, A. M. et al. Mutations in SETD2 and genes affecting histone H3K36 methylation target hemispheric high-grade gliomas. Acta Neuropathol. 125, 659–669 (2013).
Aihara, K. et al. H3F3A K27M mutations in thalamic gliomas from young adult patients. Neuro Oncol. 16, 140–146 (2014).
Broniscer, A. et al. Clinical and molecular characteristics of malignant transformation of low-grade glioma in children. J. Clin. Oncol. 25, 682–689 (2007).
Cantone, I. & Fisher, A. G. Epigenetic programming and reprogramming during development. Nature Struct. Mol. Biol. 20, 282–289 (2013).
Li, M., Liu, G. H. & Izpisua Belmonte, J. C. Navigating the epigenetic landscape of pluripotent stem cells. Nature Rev. Mol. Cell Biol. 13, 524–535 (2012).
Hirabayashi, Y. & Gotoh, Y. Epigenetic control of neural precursor cell fate during development. Nature Rev. Neurosci. 11, 377–388 (2010).
Jenuwein, T. & Allis, C. D. Translating the histone code. Science 293, 1074–1080 (2001).
Plass, C. et al. Mutations in regulators of the epigenome and their connections to global chromatin patterns in cancer. Nature Rev. Genet. 14, 765–780 (2013).
Margueron, R. & Reinberg, D. The Polycomb complex PRC2 and its mark in life. Nature 469, 343–349 (2011).
Lewis, P. W. et al. Inhibition of PRC2 activity by a gain-of-function H3 mutation found in pediatric glioblastoma. Science 340, 857–861 (2013). This is the first mechanistic demonstration of the dominant ability of histone H3K27M mutation to inhibit PRC2 activity, resulting in dominant loss of H3K27me3.
Venneti, S. et al. Evaluation of histone 3 lysine 27 trimethylation (H3K27me3) and enhancer of Zest 2 (EZH2) in pediatric glial and glioneuronal tumors shows decreased H3K27me3 in H3F3A K27M mutant glioblastomas. Brain Pathol. 23, 558–564 (2013).
Bender, S. et al. Reduced H3K27me3 and DNA hypomethylation are major drivers of gene expression in K27M mutant pediatric high-grade gliomas. Cancer Cell 24, 660–672 (2013).
Chan, K. M. et al. The histone H3.3K27M mutation in pediatric glioma reprograms H3K27 methylation and gene expression. Genes Dev. 27, 985–990 (2013).
Wagner, E. J. & Carpenter, P. B. Understanding the language of Lys36 methylation at histone H3. Nature Rev. Mol. Cell Biol. 13, 115–126 (2012).
Swartling, F. J. et al. Distinct neural stem cell populations give rise to disparate brain tumors in response to N-MYC. Cancer Cell 21, 601–613 (2012).
Barone, G., Anderson, J., Pearson, A. D., Petrie, K. & Chesler, L. New strategies in neuroblastoma: therapeutic targeting of MYCN and ALK. Clin. Cancer Res. 19, 5814–5821 (2013).
Di Lorenzo, A. & Bedford, M. T. Histone arginine methylation. FEBS Lett. 585, 2024–2031 (2011).
Behjati, S. et al. Distinct H3F3A and H3F3B driver mutations define chondroblastoma and giant cell tumor of bone. Nature Genet. 45, 1479–1482 (2013). This study identified high-frequency hotspot histone H3 mutations in rare tumour types, expanding the spectrum of mutations and cancer associated with histone H3 mutation.
Johnson, R. A. et al. Cross-species genomics matches driver mutations and cell compartments to model ependymoma. Nature 466, 632–636 (2010).
Gibson, P. et al. Subtypes of medulloblastoma have distinct developmental origins. Nature 468, 1095–1099 (2010).
Szenker, E., Ray-Gallet, D. & Almouzni, G. The double face of the histone variant H3.3. Cell Res. 21, 421–434 (2011).
Killela, P. J. et al. TERT promoter mutations occur frequently in gliomas and a subset of tumors derived from cells with low rates of self-renewal. Proc. Natl Acad. Sci. USA 110, 6021–6026 (2013).
Yan, H. et al. IDH1 and IDH2 mutations in gliomas. N. Engl. J. Med. 360, 765–773 (2009).
Brennan, C. W. et al. The somatic genomic landscape of glioblastoma. Cell 155, 462–477 (2013).
Hojfeldt, J. W., Agger, K. & Helin, K. Histone lysine demethylases as targets for anticancer therapy. Nature Rev. Drug Discov. 12, 917–930 (2013).
Shore, E. M. et al. A recurrent mutation in the BMP type I receptor ACVR1 causes inherited and sporadic fibrodysplasia ossificans progressiva. Nature Genet. 38, 525–527 (2006). This study identified germline ACVR1 mutations in patients with fibrodysplasia ossificans progressiva.
Kaplan, F. S., Lounev, V. Y., Wang, H., Pignolo, R. J. & Shore, E. M. Fibrodysplasia ossificans progressiva: a blueprint for metamorphosis. Ann. NY Acad. Sci. 1237, 5–10 (2011).
Chaikuad, A. et al. Structure of the bone morphogenetic protein receptor ALK2 and implications for fibrodysplasia ossificans progressiva. J. Biol. Chem. 287, 36990–36998 (2012).
Bagarova, J. et al. Constitutively active ALK2 receptor mutants require type II receptor cooperation. Mol. Cell. Biol. 33, 2413–2424 (2013).
Shen, Q. et al. The fibrodysplasia ossificans progressiva R206H ACVR1 mutation activates BMP-independent chondrogenesis and zebrafish embryo ventralization. J. Clin. Invest. 119, 3462–3472 (2009).
Gomes, W. A., Mehler, M. F. & Kessler, J. A. Transgenic overexpression of BMP4 increases astroglial and decreases oligodendroglial lineage commitment. Dev. Biol. 255, 164–177 (2003).
Kan, L. et al. Substance P signaling mediates BMP-dependent heterotopic ossification. J. Cell Biochem. 112, 2759–2772 (2011).
Lee, J. et al. Epigenetic-mediated dysfunction of the bone morphogenetic protein pathway inhibits differentiation of glioblastoma-initiating cells. Cancer Cell 13, 69–80 (2008).
Piccirillo, S. G. et al. Bone morphogenetic proteins inhibit the tumorigenic potential of human brain tumour-initiating cells. Nature 444, 761–765 (2006).
Zhao, H., Ayrault, O., Zindy, F., Kim, J. H. & Roussel, M. F. Post-transcriptional down-regulation of Atoh1/Math1 by bone morphogenic proteins suppresses medulloblastoma development. Genes Dev. 22, 722–727 (2008).
Vogelstein, B. et al. Cancer genome landscapes. Science 339, 1546–1558 (2013).
Ballester, L. Y. et al. Morphologic characteristics and immunohistochemical profile of diffuse intrinsic pontine gliomas. Am. J. Surg. Pathol. 37, 1357–1364 (2013).
Schumacher, M., Schulte-Monting, J., Stoeter, P., Warmuth-Metz, M. & Solymosi, L. Magnetic resonance imaging compared with biopsy in the diagnosis of brainstem diseases of childhood: a multicenter review. J. Neurosurg. 106, 111–119 (2007).
Albright, A. L. et al. Magnetic resonance scans should replace biopsies for the diagnosis of diffuse brain stem gliomas: a report from the Children's Cancer Group. Neurosurgery 33, 1026–1030 (1993).
Baker, J. N. et al. Bereaved parents' intentions and suggestions about research autopsies in children with lethal brain tumors. J. Pediatr. 163, 581–586 (2013).
Geoerger, B. et al. Innovative Therapies for Children with Cancer pediatric phase I study of erlotinib in brainstem glioma and relapsing/refractory brain tumors. Neuro Oncol. 13, 109–118 (2011).
Walker, D. A. et al. A multi-disciplinary consensus statement concerning surgical approaches to low-grade, high-grade astrocytomas and diffuse intrinsic pontine gliomas in childhood (CPN Paris 2011) using the Delphi method. Neuro Oncol. 15, 462–468 (2013).
Chalhoub, N. & Baker, S. J. PTEN and the PI3-kinase pathway in cancer. Annu. Rev. Pathol. 4, 127–150 (2009).
Acknowledgements
The recent progress in defining genetic abnormalities in diffuse intrinsic pontine glioma (DIPG) was only possible owing to the altruistic tissue donation by patients and families through autopsy or biopsy. The authors thank D. Ellison for helpful comments. C.J. acknowledges support from the National Health Service funding to the National Institute of Health Research Biomedical Research Centres and support from the Cancer Research UK Genomics Initiative, and S.J.B. acknowledges support from the US National Institutes of Health (P01CA096832) and the American Lebanese and Syrian Associated Charities (ALSAC).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Pons
-
The portion of the brainstem between the midbrain and the medulla oblongata.
- Supratentorial
-
Pertaining to brain regions above the tentorium cerebelli, which separates the cerebellum from the occipital and temporal lobes of the cerebral cortex.
- Stereotactic
-
A system of three-dimensional coordinates that is used in surgery to locate a precise position.
- Chromothripsis
-
Local chromosome shattering in which complex rearrangements with multiple interconnecting breakpoints correspond to genomic segments of oscillating copy number states.
- Exophytic
-
Growing outward beyond the surface from which it originates.
- Pilocytic astrocytomas
-
Low-grade (grade I) astrocytomas, which are the most common primary brain tumour of childhood.
- Ganglionic eminences
-
Transient structures in the embryonic telencephalon that guide tangential cell migration.
Rights and permissions
About this article
Cite this article
Jones, C., Baker, S. Unique genetic and epigenetic mechanisms driving paediatric diffuse high-grade glioma. Nat Rev Cancer 14, 651–661 (2014). https://doi.org/10.1038/nrc3811
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrc3811
This article is cited by
-
Spatially controlled construction of assembloids using bioprinting
Nature Communications (2023)
-
Histone H3-wild type diffuse midline gliomas with H3K27me3 loss are a distinct entity with exclusive EGFR or ACVR1 mutation and differential methylation of homeobox genes
Scientific Reports (2023)
-
Amplification of the PLAG-family genes—PLAGL1 and PLAGL2—is a key feature of the novel tumor type CNS embryonal tumor with PLAGL amplification
Acta Neuropathologica (2023)
-
CRISPR screening of E3 ubiquitin ligases reveals Ring Finger Protein 185 as a novel tumor suppressor in glioblastoma repressed by promoter hypermethylation and miR-587
Journal of Translational Medicine (2022)
-
The Epigenetic Regulation of OLIG2 by Histone Demethylase KDM6B in Glioma Cells
Journal of Molecular Neuroscience (2022)