Abstract
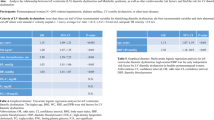
We sought to determine the predictors of primary episodes of mild diastolic dysfunction (DD) in a cohort of women aged >45 years, who had >2 echocardiography from 2009 to 2012. Patients were excluded if they had prior diagnosis of coronary artery disease, heart failure, valvular heart disease or echocardiographic evidence of DD. Mild DD was defined as: left ventricular ejection fraction>50%, E/A ratio<0.75, and E/e’⩽8. Out of the total 758 subjects (age 64.15±7.24 years), 109 (14.3%) had developed mild DD, during a mean followup period of 3 years. Independent predictors of mild DD included: age (P<0.001), history of hypertension (P=0.022), body mass index (BMI) (P<0.001), total triglycerides (TG) (P=0.016), inter ventricular septal thickness (P=0.015) and brachial-ankle pulse wave velocity (baPWV) ⩾16 m s−1 (P<0.001). E/A ratio was inversely associated with age (r=−0.337, P<0.001), baPWV (r=−0.359, P<0.001), BMI (r=−0.290, P<0.001) and TG (r=−0.255, P<0.001). The Area Under roc Curve for a linear combination of age, BMI, baPWV and TG was 0.738 (95% confidence interval: 0.683–0.804, P<0.001), which was superior to any of the variables taken alone. In summary, many middle-aged or elderly women may develop mild DD within a relatively short period of 3 years. Several subclinical abnormalities and cardiovascular parameters were determined to contribute to the onset of DD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Gaasch WH, Zile MR . Left ventricular diastolic dysfunction and diastolic heart failure. Annu Rev Med 2004; 55: 373–394.
Kawaguchi M, Hay I, Fetics B, Kass DA . Combined ventricular systolic and arterial stiffening in patients with heart failure and preserved ejection fraction: implications for systolic and diastolic reserve limitations. Circulation 2003; 107 (5): 714–720.
Tsang TS, Barnes ME, Gersh BJ, Bailey KR, Seward JB . Risks for atrial fibrillation and congestive heart failure in patients >/=65 years of age with abnormal left ventricular diastolic relaxation. Am J Cardiol 2004; 93 (1): 54–58.
Rosenberg MA, Manning WJ . Diastolic dysfunction and risk of atrial fibrillation: a mechanistic appraisal. Circulation 2012; 126 (19): 2353–2362.
Kane GC, Karon BL, Mahoney DW, Redfield MM, Roger VL, Burnett JC Jr et al. Progression of left ventricular diastolic dysfunction and risk of heart failure. JAMA 2011; 306 (8): 856–863.
Redfield MM, Jacobsen SJ, Burnett JC Jr., Mahoney DW, Bailey KR, Rodeheffer RJ . Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003; 289 (2): 194–202.
Yamashina A, Tomiyama H, Takeda K, Tsuda H, Arai T, Hirose K et al. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens Res 2002; 25 (3): 359–364.
Munakata M, Ito N, Nunokawa T, Yoshinaga K . Utility of automated brachial ankle pulse wave velocity measurements in hypertensive patients. Am J Hypertensn 2003; 16 (8): 653–657.
Otsuka T, Munakata R, Kato K, Kodani E, Ibuki C, Kusama Y et al. Oscillometric measurement of brachial artery cross-sectional area and its relationship with cardiovascular risk factors and arterial stiffness in a middle-aged male population. Hypertens Res 2013; 36 (10): 910–915.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005; 18 (12): 1440–1463.
Khouri SJ, Maly GT, Suh DD, Walsh TE . A practical approach to the echocardiographic evaluation of diastolic function. J Am Soc Echocardiogr 2004; 17 (3): 290–297.
Wan SH, Vogel MW, Chen HH . Pre-clinical diastolic dysfunction. J Am Coll Cardiol 2014; 63 (5): 407–416.
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogry 2009; 10 (2): 165–193.
Kang S, Fan HM, Li J, Fan LY, Miao AY, Bao Y et al. Relationship of arterial stiffness and early mild diastolic heart failure in general middle and aged population. Eur Heart J. 2010; 31 (22): 2799–2807.
Abhayaratna WP, Marwick TH, Smith WT, Becker NG . Characteristics of left ventricular diastolic dysfunction in the community: an echocardiographic survey. Heart 2006; 92 (9): 1259–1264.
Kankaanpaa M, Lehto HR, Parkka JP, Komu M, Viljanen A, Ferrannini E et al. Myocardial triglyceride content and epicardial fat mass in human obesity: relationship to left ventricular function and serum free fatty acid levels. J Clin Endocrinol Metab 2006; 91 (11): 4689–4695.
de las Fuentes L, Waggoner AD, Brown AL, Davila-Roman VG . Plasma triglyceride level is an independent predictor of altered left ventricular relaxation. J Am Soc Echocardiogr 2005; 18 (12): 1285–1291.
Gaasch WH, Zile MR . Left ventricular structural remodeling in health and disease: with special emphasis on volume, mass, and geometry. J Am Coll Cardiol 2011; 58 (17): 1733–1740.
Kitzman DW, Scholz DG, Hagen PT, Ilstrup DM, Edwards WD . Age-related changes in normal human hearts during the first 10 decades of life. Part II (Maturity): a quantitative anatomic study of 765 specimens from subjects 20 to 99 years old. Mayo Clin Proc 1988; 63 (2): 137–146.
Grossman C, Grossman A, Koren-Morag N, Azaria B, Goldstein L, Grossman E . Interventricular septum thickness predicts future systolic hypertension in young healthy pilots. Hypertens Res 2008; 31 (1): 15–20.
Libhaber CD, Woodiwiss AJ, Booysen HL, Maseko MJ, Majane OH, Sareli P et al. Differential relationships of systolic and diastolic blood pressure with components of left ventricular diastolic dysfunction. J Hypertens 2014; 32 (4): 912–920.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D et al. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27 (21): 2588–2605.
Sugawara J, Hayashi K, Yokoi T, Cortez-Cooper MY, DeVan AE, Anton MA et al. Brachial-ankle pulse wave velocity: an index of central arterial stiffness? J Hum Hypertens 2005; 19 (5): 401–406.
van Sloten TT, Schram MT, van den Hurk K, Dekker JM, Nijpels G, Henry RM et al. Local stiffness of the carotid and femoral artery is associated with incident cardiovascular events and all-cause mortality: the Hoorn study. J Am Coll Cardiol 2014; 63 (17): 1739–1747.
Mottram PM, Haluska BA, Leano R, Carlier S, Case C, Marwick TH . Relation of arterial stiffness to diastolic dysfunction in hypertensive heart disease. Heart 2005; 91 (12): 1551–1556.
Venskutonyte L, Jarnert C, Ryden L, Kjellstrom B . Longitudinal development of left ventricular diastolic function in patients with type 2 diabetes. Diabetes Care 2014; 37 (11): 3092–3097.
Da Ros R, Assaloni R, Ceriello A . The preventive anti-oxidant action of thiazolidinediones: a new therapeutic prospect in diabetes and insulin resistance. Diabet Med 2004; 21 (11): 1249–1252.
Poirier P, Bogaty P, Garneau C, Marois L, Dumesnil JG . Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care 2001; 24 (1): 5–10.
Gjesdal O, Bluemke DA, Lima JA . Cardiac remodeling at the population level—risk factors, screening, and outcomes. Nat Rev Cardiol 2011; 8 (12): 673–685.
Dupont S, Maizel J, Mentaverri R, Chillon JM, Six I, Giummelly P et al. The onset of left ventricular diastolic dysfunction in SHR rats is not related to hypertrophy or hypertension. Am J Physiol Heart Circ Physiol 2012; 302 (7): H1524–H1532.
Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C et al. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation 2008; 118 (25): 2679–2686.
de Koning L, Merchant AT, Pogue J, Anand SS . Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur Heart J 2007; 28 (7): 850–856.
Acknowledgements
The study was carried out as a collaborative study supported by the residents’ Committee of Lujiazui Community, Shanghai; Center of Cardiology, Department of Ultrasonography and Department of Clinical Laboratory in Shanghai East Hospital. The authors express their sincere gratitude to all the staffs in this survey for their important contribution. Funding sources: The study was funded by scientific and technological development and innovation fund of government of Pudong New Area, Shanghai; Shanghai Municipal Commission of Health and Family Planning (No. 201440312); the Nature Science Foundation of China (No. 81001252, 81170325); Shanghai Municipal Health Bureau, China (No. 201440312).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Journal of Human Hypertension website
Supplementary information
Rights and permissions
About this article
Cite this article
Wu, J., Yu, S., Wo, D. et al. Risks and predictors of mild diastolic dysfunction among middle-aged and aged women: a population-based cohort study. J Hum Hypertens 30, 335–340 (2016). https://doi.org/10.1038/jhh.2015.85
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhh.2015.85
This article is cited by
-
Adverse cardiovascular and metabolic perturbations among older women: ‘fat-craving’ hearts
Clinical Research in Cardiology (2023)
-
Application of 123I-MIBG myocardial maximum standardized uptake value to characterize cardiac function in patients with pheochromocytoma: comparison with echocardiography
Japanese Journal of Radiology (2023)