Abstract
The predominant risk factor of metabolic syndrome is intra-abdominal fat accumulation, which is determined by waist circumference and waist–hip ratio measurements and visceral fat area (VFA) that is measured by computed tomography (CT). There is evidence that waist circumference and waist–hip ratio in the Caucasian population are associated with variations in several genes, including neurexin 3 (NRXN3), transcription factor AP-2β (TFAP2B), methionine sulfoxide reductase A (MSRA), lysophospholipase-like-1 (LYPLAL1), fat mass and obesity associated (FTO) and melanocortin 4 receptor (MC4R) genes. To investigate the relationship between VFA and subcutaneous fat area (SFA) and these genes in the recruited Japanese population, we genotyped 8 single-nucleotide polymorphisms (SNPs) in these 6 genes from 1228 subjects. Multiple regression analysis revealed that gender, age, and rs1558902 and rs1421085 genotypes (additive model) in FTO were significantly associated with body mass index (BMI; P=0.0039 and 0.0039, respectively), SFA (P=0.0027 and 0.0023, respectively) and VFA (P=0.045 and 0.040, respectively). However, SNPs in other genes, namely, NRXN3, TFAP2B, MSRA, LYPLAL1 and MC4R were not significantly associated with BMI, SFA or VFA. Our data suggest that some SNPs, which were identified in genome-wide studies in the Caucasians, also confer susceptibility to fat distribution in the Japanese subjects.
Similar content being viewed by others
Introduction
Metabolic syndrome is a common clinical phenotype that is manifested as concurrent metabolic abnormalities, including central obesity, glucose intolerance, dyslipidemia and hypertension.1 Because several other definitions also exist,2 the adequacy of this concept remains debatable. Recently, metabolic syndrome has attracted considerable interest because of increasing the number of patients. Although the pathogenesis of metabolic syndrome is not fully understood, the predominant underlying risk factor is considered to be visceral obesity due to an atherogenic diet and physical inactivity, in addition to certain genetic factors.1, 2 Adipose tissue, especially the visceral fat, secretes various adipocytokines. An increase in the adipose tissue mass leads to an alteration in the plasma adipocytokine level, resulting in dyslipidemia, hypertension and insulin resistance.3, 4 Intra-abdominal fat accumulation (central adiposity) is determined in terms of the waist circumference and waist–hip ratio measurements and visceral fat area (VFA) that is measured by computed tomography (CT).1, 5, 6 Recently, two genome-wide association studies had been conducted to identify the loci that were linked with waist circumference or waist–hip ratio.7, 8
In this study, we investigated the association of single-nucleotide polymorphisms (SNPs) in neurexin 3 (NRXN3), transcription factor AP-2β (TFAP2B), methionine sulfoxide reductase A (MSRA), lysophospholipase-like-1 (LYPLAL1), fat mass and obesity associated (FTO) and melanocortin 4 receptor (MC4R) genes with VFA and subcutaneous fat area (SFA) that were determined by CT.
Materials and methods
Study subjects
We recruited 1228 Japanese subjects from outpatient clinics after they agreed to undergo CT examinations (supine position) that were performed to determine the VFA and SFA values at the level of the umbilicus (L4–L5). Both VFA and SFA were calculated using the FatScan software program (N2system, Osaka, Japan).9 The clinical characteristics of the patients are summarized in Table 1.
All subjects provided their informed written consent, and the protocol was approved by the ethics committee of each institution and by that of RIKEN.
DNA extraction and SNP genotyping
Using Genomix (Talent Srl, Trieste, Italy), genomic DNA was extracted from blood samples collected from each subject. We constructed Invader probes (Third Wave Technologies, Madison, WI, USA) for rs1558902 and rs1421085 in FTO, rs489693 and rs17700144 in MC4R, rs1046997 in NRXN3, rs987237 in TFAP2B, rs782622 (rs545854) in MSRA and rs2605100 in LYPLAL1. The SNPs were genotyped using Invader assays as described previously.10 The success rate of this assays was >99.0%.
Statistical analysis
Differences in the quantitative clinical data between case and control groups were tested by the Mann–Whitney U-test. Differences in the quantities of clinical data between the different genotypes were assessed by the Kruskal–Wallis test. We coded genotypes as 0, 1 or 2 depending on the number of copies of the risk alleles. Multiple linear regression analysis was performed to test the independent effect of risk alleles on body mass index (BMI), VFA or SFA by considering the effects of other variables (age and gender), which were assumed to be independent of the effect of the SNPs. The significance of the association between an independent variable and dependent variable was determined using a t-test. Hardy–Weinberg equilibrium was assessed using the χ2-test.11
Results
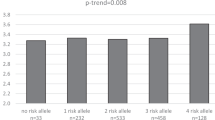
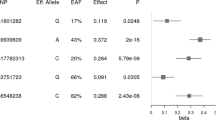
BMI, VFA and SFA are known to be affected by gender, and an association between rs2605100 in LYPLAL1 and the waist–hip ratio has been reported only in women.7 Therefore, we first compared the anthropometric parameters (BMI, VFA and SFA) among the different genotypes in the men and women. One SNP—rs10146997 in NRXN3—was found to be monomorphic, as reported in the HapMap database. Two SNPs (rs1558902 and rs1421085) in FTO were significantly associated with BMI in women (Table 2). The association of rs489693 and rs17700144 in MC4R with BMI has been reported in the Caucasian population;7, 8 however, such association was not observed in our study. The SNPs in TFAP2B, MSRA and LYPLAL1 were not associated with BMI, which is a finding consistent with that of Lindgren et al.7 No SNPs in the five genes were associated with VFA in either men or women (Table 3). Although rs489693 was marginally associated with VFA in men, the risk allele was different from that reported in the Caucasian population.7 Two SNPs (rs1558902 and rs1421085) in FTO were significantly associated with SFA both in men (P=0.034 and 0.040, respectively) and women (P=0.010 and 0.0083, respectively) (Table 4). SNPs in other genes were not significantly associated with SFA. All SNPs were found to exhibit Hardy–Weinberg equilibrium (P>0.10).
Next, we attempted to perform multiple linear regression analysis by using BMI, VFA and SFA as the dependent variables, and with age, gender or genotype as an explanatory variable. We transformed genotypes to 0, 1 or 2 depending on the number of copies of the risk alleles. The A-allele of rs1558902 and the C-allele of rs1421085 in FTO were significantly associated with increases in BMI (P=0.0039 and 0.0039, respectively), VFA (P=0.045 and 0.040, respectively) and SFA (P=0.0027 and 0.0023, respectively) even after age and gender were included in the model (Supplementary Tables 1, 2, and 3). Multiple linear regression analysis showed that the SNPs of other genes were not significantly associated with BMI, VFA and SFA.
We also conducted power analysis of linear regression (additive model) with a significance level of 0.05, considering the effect size of the parameters. For rs1558902, the estimated effect sizes per allele (regression coefficients) for VFA and SFA were 5.8 and 14.4 cm2, respectively (Supplementary Tables 2 and 3). The power of our statistical test was calculated on the basis of these estimated effect sizes and by performing 10 000 simulations. When the allele frequency was assumed to be 0.2, the power was estimated to be 0.32 for VFA and 0.81 for SFA; however, when the allele frequency was assumed to be 0.1, the respective powers were estimated to be 0.20 and 0.56.
Discussion
The most important risk factor for metabolic syndrome is visceral fat obesity. According to the criteria released by the Japanese Committee for the Diagnostic Criteria of Metabolic Syndrome in April 2005,5 metabolic syndrome is defined by the presence of two or more abnormalities (dyslipidemia, impaired glucose tolerance or diabetes and hypertension), in addition to visceral fat obesity. The cutoff points for visceral fat obesity (waist circumference, 85 cm in men and 90 cm in women) are based on the cutoff point for VFA (100 cm2) that is determined by CT.5, 6 Visceral fat mass measurement by CT is more precise than that derived from BMI or waist circumference measurements. Furthermore, for predicting metabolic risk-factor clustering, VFA is superior to waist circumference or BMI.12 Therefore, we examined the association of VFA and SFA with the SNPs related to waist circumference and waist–hip ratio, and identified in a genome-wide study.7, 8 We found that the SNPs in FTO were significantly associated with BMI, as we have previously reported.13 We also found that these SNPs were associated with VFA and SFA; however, the association between these SNPs and VFA was marginal because VFA was not significantly different among the genotypes in men. We did not find any association between other SNPs and BMI, VFA or SFA. These findings may be due to the low power of this study. Therefore, further studies with more subjects should be conducted to conclude that SNPs in genes other than FTO are not associated with VFA or SFA.
SNPs in FTO were associated with SFA and VFA. Therefore, some of the SNPs, which were identified by genome-wide association studies in the Caucasian population, were also found to confer susceptibility to body fat distribution in the Japanese subjects. On the other hand, rs10146997 in NRXN3 was found to be monomorphic in our subjects, and we could not find associations between SNPs in MC4R, TFAP2B, MSRA or LYPLAL1 and VFA or SFA. Thus, there is a possibility that genetic susceptibility to body fat distribution is likely to differ among various ethnic groups.
rs1558902 and rs1421085 in FTO were in linkage disequilibrium with rs9939609, which is associated with obesity and type II diabetes.14, 15, 16 Concentrations of circulating adipocytokines are affected by the accumulation of adipose tissue, especially visceral adipose tissue. Therefore, rs1558902 and rs1421085 probably affect subcutaneous and visceral fat accumulation, leading to the development of type II diabetes by altered adipocytokine secretion. The precise mechanism of how FTO affects adipose tissue accumulation is not clear yet; however, there is evidence that FTO is involved in the development of obesity. FTO is ubiquitously expressed, and a strong expression is observed in the arcuate, paraventricular, dorsomedial and ventromedial nuclei, which are critical energy-regulation sites.16, 17, 18 FTO also exists in the nucleus and is reported to be a member of the Fe(II) and 2-oxoglutarate-dependent oxygenase superfamily.17, 19 FTO-deficient and dominant-negative mutant FTO mice have shown reduced fat mass and increased energy expenditure.20, 21 These reports indicate that FTO has an important role in energy homeostasis by regulating energy expenditure. Although the effects of the SNPs rs1558902 and rs1421085 on gene expression need to be elucidated, variations in FTO probably affect subcutaneous and visceral fat accumulation.
In summary, we showed that rs1558902 and rs1421085 in FTO may be associated with SFA and VFA in the Japanese population. In our study, rs489693 and rs17700144 in MC4R, rs1046997 in NRXN3, rs987237 in TFAP2B, rs782622 (rs545854) in MSRA and rs2605100 in LYPLAL1 were not associated with SFA or VFA.
References
Carr, D. B., Utzschneider, K. M., Hull, R. L., Kodama, K., Retzlaff, B. M., Brunzell, J. D. et al. Intra-abdominal fat is a major determinant of the National Cholesterol Education Program Adult Treatment Panel III criteria for the metabolic syndrome. Diabetes 53, 2087–2094 (2004).
Pollex, R. L. & Hegele, R. A. Genetic determinants of the metabolic syndrome. Nat. Clin. Pract. Cardiovasc. Med. 3, 482–489 (2006).
Matsuzawa, Y. Therapy insight: adipokines in metabolic syndrome and related cardiovascular disease. Nat. Clin. Pract. Cardiovasc. Med. 3, 35–42 (2006).
Hotta, K., Funahashi, T., Bodkin, N. L., Ortmeyer, H. K., Arita, Y., Hansen, B.C. et al. Circulating concentrations of the adipocyte protein adiponectin are decreased in parallel with reduced insulin sensitivity during the progression to type 2 diabetes in rhesus monkeys. Diabetes 50, 1126–1133 (2001).
Arai, H., Yamamoto, A., Matsuzawa, Y., Saito, Y., Yamada, N., Oikawa, S. et al. Prevalence of metabolic syndrome in the general Japanese population in 2000. J. Atheroscler. Thromb. 13, 202–208 (2006).
Mastuzawa, Y. Metabolic syndrome-definition and diagnostic criteria in Japan. J. Atheroscler. Thromb. 12, 301 (2005).
Lindgren, C. M., Heid, I. M., Randall, J. C., Lamina, C., Steinthorsdottir, V., Qi, L. et al. Genome-wide association scan meta-analysis identifies three Loci influencing adiposity and fat distribution. PLoS Genet. 5, e1000508 (2009).
Heard-Costa, N. L., Zillikens, M. C., Monda, K. L., Johansson, A., Harris, T. B., Fu, M. et al. NRXN3 is a novel locus for waist circumference: a genome-wide association study from the CHARGE Consortium. PLoS Genet. 5, e1000539 (2009).
Yoshizumi, T., Nakamura, T., Yamane, M., Islam, A. H., Menju, M., Yamasaki, K. et al. Abdominal fat: standardized technique for measurement at CT. Radiology 211, 283–286 (1999).
Ohnishi, Y., Tanaka, T., Ozaki, K., Yamada, R., Suzuki, H. & Nakamura, Y. A high-throughput SNP typing system for genome-wide association studies. J. Hum. Genet. 46, 471–477 (2001).
Nielsen, D. M., Ehm, M. G. & Weir, B. S. Detecting marker-disease association by testing for Hardy-Weinberg disequilibrium at a marker locus. Am. J. Hum. Genet. 63, 1531–1540 (1998).
Matsushita, Y., Nakagawa, T., Yamamoto, S., Takahashi, Y., Yokoyama, T., Noda, M. et al. Associations of visceral and subcutaneous fat areas with the prevalence of metabolic risk factor clustering in 6292 Japanese individuals: the Hitachi Health Study. Diabetes Care (in press).
Hotta, K., Nakata, Y., Matsuo, T., Kamohara, S., Kotani, K., Komatsu, R. et al. Variations in the FTO gene are associated with severe obesity in the Japanese. J Hum. Genet. 53, 546–553 (2008).
Frayling, T. M., Timpson, N. J., Weedon, M. N., Zeggini, E., Freathy, R. M., Lindgren, C. M. et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316, 889–894 (2007).
Scott, L. J., Mohlke, K. L., Bonnycastle, L. L., Willer, C. J., Li, Y., Duren, W. L. et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science 316, 1341–1345 (2007).
Scuteri, A., Sanna, S., Chen, W. M., Uda, M., Albai, G., Strait, J. et al. Genome-wide association scan shows genetic variants in the FTO gene are associated with obesity-related traits. PLoS Genet. 3, e115 (2007).
Gerken, T., Girard, C. A., Tung, Y. C., Webby, C. J., Saudek, V., Hewitson, K. S. et al. The obesity-associated FTO gene encodes a 2-oxoglutarate-dependent nucleic acid demethylase. Science 318, 1469–1472 (2007).
Lein, E. S., Hawrylycz, M. J., Ao, N., Ayres, M., Bensinger, A., Bernard, A. et al. Genome-wide atlas of gene expression in the adult mouse brain. Nature 445, 168–176 (2007).
Jia, G., Yang, C. G., Yang, S., Jian, X., Yi, C., Zhou, Z. et al. Oxidative demethylation of 3-methylthymine and 3-methyluracil in single-stranded DNA and RNA by mouse and human FTO. FEBS Lett 582, 3313–3319 (2008).
Fischer, J., Koch, L., Emmerling, C., Vierkotten, J., Peters, T., Brüning, J. C. et al. Inactivation of the Fto gene protects from obesity. Nature 458, 894–898 (2009).
Church, C., Lee, S., Bagg, E. A., McTaggart, J. S., Deacon, R., Gerken, T. et al. A mouse model for the metabolic effects of the human fat mass and obesity associated FTO gene. PLoS Genet. 5, e1000599 (2009).
Acknowledgements
We express our appreciation to Ms Ritsuko Kusano for her contribution to our study. This work was supported by a grant from the Grants-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (21591186) and by the Mitsui Life Science Social Welfare Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Hotta, K., Nakamura, M., Nakamura, T. et al. Polymorphisms in NRXN3, TFAP2B, MSRA, LYPLAL1, FTO and MC4R and their effect on visceral fat area in the Japanese population. J Hum Genet 55, 738–742 (2010). https://doi.org/10.1038/jhg.2010.99
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2010.99
Keywords
This article is cited by
-
Unique genetic variants of lean nonalcoholic fatty liver disease: a retrospective cohort study
BMC Endocrine Disorders (2023)
-
Association of FTO common variant (rs9939609) with body fat in Turkish individuals
Lipids in Health and Disease (2019)
-
Genome-wide association studies suggest sex-specific loci associated with abdominal and visceral fat
International Journal of Obesity (2016)
-
Genetic variations in the CYP17A1 and NT5C2 genes are associated with a reduction in visceral and subcutaneous fat areas in Japanese women
Journal of Human Genetics (2012)
-
Association between type 2 diabetes genetic susceptibility loci and visceral and subcutaneous fat area as determined by computed tomography
Journal of Human Genetics (2012)