Abstract
Purpose
The aim of the present study is to investigate the association of the polymorphism of two genes in CXC chemokine family, interleukin-8 (IL-8) and interferon-inducible protein 10 (IP-10), with both susceptibility and progression of DR in T2D population of northern China.
Patients and methods
A total of 1043 eligible type 2 diabetic patients from Heilongjiang of northern China were recruited for this study. They were grouped into: with diabetic retinopathy (DR, 528 cases) and without diabetic retinopathy (DNR, 515 cases). Single nucleotide polymorphism (SNP) genotyping of IL-8(-251T/A) and IP-10(-1596C/T) was performed by polymerase chain reaction. Multivariate analysis and stepwise multiple logistic progression analysis were conducted to evaluate the association between gene SNP and DR susceptibility and progression. Pooled odds ratio (OR) with 95% confidence interval (CI) was applied to assess the strength of the association among study groups.
Results
The occurring of IL-8(-251) AA genotype was correlated with susceptibility (OR: 2.286, 95% CI: 1.382–3.782, P=0.001) and progression of high-risk proliferative diabetic retinopathy (PDR) (OR: 0.354, 95% CI: 0.162–0.770, P=0.009). Reversely, T allele of IP-10 (-1596) C/T was correlated with a reduced risk of DR (OR: 0.341, 95% CI: 0.249–0.466, P<0.001). However, gene polymorphisms of IL-8–251T/A and IP-10–1596C/T were not associated with diabetic macular edema (DME)(P>0.05).
Conclusions
AA genotype of IL-8–251T/A was closely correlated to DR and high-risk proliferative diabetic retinopathy (PDR). -1596T allele of the IP-10 is a beneficial genotype for DR.
Similar content being viewed by others
Introduction
Diabetic retinopathy (DR), a serious complication of type II diabetic mellitus (T2D) with progressively retinal degeneration, ranks as the second leading cause of blindness, contributing to an overall 4.8% blindness globally.1 Although the pathogenesis of DR is not yet completely elucidated, it is widely considered that environmental and genetic factors are associated with DR incidence and progression.2, 3, 4, 5, 6 Particularly, some candidate genes related with inflammation and agiogenesis, such as VEGF, erythropoietin (EPO), and cytokines, are screened by genome-wide analysis and become major causative mechanisms. Therefore, intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) has been applied clinically. This specific therapy mitigates the severity of microvascular complications such as retinal angiogenesis and diabetic macular edema (DME).7, 8 The major weakness of this therapy accounts for the reduplicating and invasive intravitreal injection procedure, which carries potential risk of inflammation to patients.9 It is urgent and clinically demanding to emerge novel therapeutic approaches applied to DR complications.
CXC motif chemokine ligand 8 (IL-8) and interferon gamma-induced protein 10 (IP-10) are members of CXC chemokines family.10, 11, 12, 13 IL-8 is produced by numerous cell types, such as macrophages, epithelial and endothelial cells, in response to inflammatory stimulus. It exhibits a potent chemotactic activity during inflammatory process.14 Particularly, IL-8 enhances inflammation and stimulates angiogenesis by binding its receptor and inducing downstream signaling.10, 11, 12 Elevated production of IL-8 has been found in retina plasma and vitreous fluids of DR, and it may contribute to drive the progression of proliferative diabetic retinopathy (PDR).15 Some related evidence in the field has also shown that IL-8 has important roles in the pathogenesis of cancer, including angiogenesis, tumor growth, and metastasis.16, 17, 18, 19 Therefore, the screening of IL-8 as biomarker is becoming a promising aim for better understanding the pathophysiology of DR. The antimicrobial gene IP-10 will bind its receptor upon microbial invasion.13 As the consequence, it initiates and stimulates the infiltration of monocytes, natural killer and T-cell against infection. It is reported that IP-10 may inhibit angiogenesis in vivo, at least partially by antagonizing the function of IL-8.20, 21, 22 IL-8 and IP-10 are candidate biomarker genes for several complex diseases, including T2D, rheumatoid arthritis and renal failure.23, 24 It was shown that polymorphisms of IL-8–251T/A and IP-10–1596C/T were associated with age-related macular degeneration (AMD) both in vivo and in vitro.25, 26, 27, 28 Up to date, it still demands more clinical evidence for identifying biomarkers, such as IL-8 and IP-10, and evaluating the correlation of biomarkers with the susceptibility and progression of DR. Our study is to identify susceptible or beneficial single nucleotide polymorphisms (SNPs) involved in DR.
We had previously found that monocyte chemoattractant protein-1 (MCP-1) 2518G/G genotype was a susceptibility gene for DR in Chinese type 2 diabetic patients, especially the high-risk PDR.29 In order to expand current clinical evidence on biomarker screening, we further investigated the significance of IL-8(-251T/A) and IP-10(-1596C/T) SNPs in type 2 diabetic retinopathy (T2DR) in northern Chinese population.
Materials and methods
Patient recruitment and sample collection
The criteria for inclusion and exclusion of participants were described in the previous study.29 Briefly, the study recruited eligible 1043 type 2 diabetic (T2D) patients, 502 for male and 541 for female, from the Department of Endocrinology in the First Affiliated Hospital of Harbin Medical University (Harbin, China) from October 2011 to April 2013. Patients with <5 year duration of type 2 diabetes were excluded from the study. Eligible age spanned from 34 to 82 years old. The protocol of this study was approved by the Institutional Review Board (IRB) of Harbin Medical University and conformed to Declaration of Helsinki. All patients submitted the written informed consent for participation prior to the start of this study.
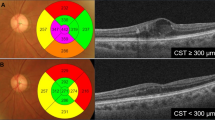
A total of 1043 eligible subjects were assigned into: with diabetic retinopathy group (DR group, 528 cases) and without retinopathy group (DNR group, 515 cases) according to the criteria as the following. Briefly, all participants were subjected to detailed investigation of family health history, blood urea, glycosylated hemoglobin, smoking and alcohol consumption hobbies, BMI and blood pressure. 3 ml blood was collected from each subject for SNP study. All patients underwent ophthalmic examination, including best-corrected visual acuity, intraocular pressure, slit lamp, and fundus examination in the Department of Ophthalmology, Harbin Medical University. Age, gender, and ethnicity were matched in the two groups. Detailed medical and ophthalmologic histories of each patient were recorded. Further examination like fundus fluorescein angiography (FFA) and optical coherence tomography (OCT) were conducted in patients whose retinopathy (microaneurysm, hemorrhage) were found. FFA was used to grade the severity of DR in a masked manner by ophthalmologists.29 OCT was used to evaluate retinal function. According to the modified Early Treatment of Diabetic Retinopathy Study Airlie House classification, DR group was graded and assigned to the following subgroups: mild non-proliferative diabetic retinopathy (NPDR), moderate NPDR, severe NPDR, and proliferative diabetic retinopathy (PDR).30
Among the DR patients, there were 76 mild NPDR patients, 79 moderate NPDR patients, 96 severe NPDR patients, and 277 PDR patients (including 169 high-risk PDR). All the DR patients were categorized into three groups according to the central macular thickness (mild ≤250 μm; 250 μm<moderate <350 μm; severe ≥350 μm). The examination of right eye was eligible to evaluate the severity of DR or diabetic macular edema (DME) for grouping. We have proven that there was no statistical significant difference between the left and right eye.29 Macular thickness was examined using OCT. Certain end-stages of retinopathy were excluded, such as Pan-Retinal Photocoagulation (PRP), atrophy of eyeball, epimacular membrane, age-related macular degeneration (AMD).
Genotyping
Peripheral leukocytes were isolated from EDTA-treated whole blood obtained from each subject, and genomic DNA was extracted with QIAamp DNA Mini Blood Kit (Qiagen, Hilden, Germany) for polymerase chain reaction (PCR) amplification of IL-8 and IP-10. DNA samples were collected in a 1.5 ml nuclease-free Eppendorf tube and stored at −20 °C until use.
The SNPs were detected by using an automated ABI PRISM 3730 DNA analyzer (Thermo Fisher Scientific, Grand Island, NY, USA). PCR was used to amplify the primer. For IL-8(-251A/T), the forward primer 5′GGCAAACCTGAGTCATCACA3′ and reverse primer 5′GGCTGGCTTATCTTCACCAT3′ were used to amplify a 306 bp fragment in a final PCR mixture of 20 μl containing 100 ng of genomic DNA and 12.5 pmol of each primer. For IP-10 (-1596C/T), the forward primer 5′GCCTTGGTACAGCACATCAG3′ and reverse primer 5′GCCAAGTCCTGCTCATCCT3′ were used to amplify a 539 bp fragment. The cycling parameters were initial denaturation at 95 °C for 2 min, followed by 30 cycles of denaturation at 95 °C for 20 s, annealing at 57 °C for 30 s and elongation at 72 °C for 40 s, and a final extension at 72 °C for 5 min.
Statistical analysis
All statistical analysis was performed with SPSS version 12.0 (SPSS Inc., Chicago, IL, USA). Χ2 was used to test the allelic and genotypic associations of the SNP, and Hardy-Weinberg equilibrium of the SNPs was also applied using a Χ2 test. Odds ratio, relative risk were also calculated using the same programs. Multivariate analysis and multiple logistic regression analysis were conducted to evaluate the association of genotypes with DR. Statistical significance was established at P<0.05. Unpaired Student’s t-test was used to compare the difference between the two groups. P-value<0.05 was considered significant.
Results
The clinical lab examination did not show any difference in the study subjects between DR and DNR groups (Table 1). DR group displayed a significantly higher frequency of both IL-8–251 AA (OR: 2.286, 95% CI: 1.382–3.782, P=0.001) and the allele of IL-8–251 A (OR: 0.660, 95% CI: 0.542–0.804, P<0.001) in comparison with DNR (Table 2A). Moreover, it showed that PDR had a significantly higher frequency of IL-8–251AA (OR: 0.354, 95% CI: 0.162–0.770, P=0.009) in comparison with NPDR when stratified by the grade of DR. In addition, the frequency of IL-8(-251) A allele was significantly elevated in high-risk PDR patients (OR: 1.801, 95% CI: 1.279–2.538, P<0.001) compared with NPDR (Table 2B). Reversely, the data in Table 3A showed that the frequency of IP-10(-1596) C/T genotype (OR: 0.255, 95% CI: 0.178–0.364, P<0.001) significantly decreased in DR in comparison with that of DNR. It suggests that IP-10(-1596) C/T may be a beneficial genotype with less susceptibility to DR. Moreover, IP-10(-1596) T allele had a significantly decreased occurring probability in DR group (OR: 0.341, 95% CI: 0.249–0.466, P<0.001) compared with that of DNR group. Although SNPs of IP-10(-1596) did not show any statistically significant difference between NPDR and PDR groups, T allele of IP-10(-1596) (OR: 0.456, 95 % CI: 0.229–0.908, P<0.05; Table 3B) had a dramatically higher frequency in NPDR compared with PDR when stratified by the grade of DR. No association was found between the polymorphism of two genes, IL-8–251T/A and IP-10–1596C/T, and the susceptibility of DME (P>0.05) (Table 4A). To determine whether the association of IL-8 with DR was independent of IP-10 and clinical conditions, multiple logistic regression analyses (Table 4B) were conducted and revealed that these two genetic factors remained significant (P<0.05) when conditioning on each other and main clinical complications. It demonstrates the independent effects of IL-8(-251) or IP-10(-1596) in DR development.
Discussion
DR is a life-quality-threatened complications at late stage of T2D. Our study is aimed at finding DR-related genes and ideally foreseeing DR vulnerability and progression. Ocular inflammation and neovascularization are critical mechanisms of DR because inflammatory cytokines are found increased in the diabetic retina.31, 32, 33, 34, 35, 36 IL-8, a member of chemotactic cytokines, is produced by activated inflammatory cells, such as neutrophils and monocytes/microphages.10, 11, 12 Elevated level of IL-8 has the essential role in initiating and strengthening inflammatory cascade.6 However, IP-10, a poor neutrophil chemoattractant and activator, may exert a inhibiting inflammation function.13 It shows that IP-10 prevents IL-8–induced neovascularization in a corneal pocket model of angiogenesis and inhibits IL-8–induced endothelial chemotaxis.21, 22 The relationship between inflammation cytokines and DR progression is further established.37 Elner et al,15 previously found significantly elevated level of vitreous IL-8 in patients with PDR. And they identified IL-8 as an angiogenic stimulant that may be produced by resident cells within the eyes.38 Recently, a study in the field finds that glycated serum proteins may enhance IL-8 production.39 It suggests the essential role of IL-8 in mediating DR progression. It is rational to frame our current study, which is aimed at addressing the relationship of IL-8 gene and DR susceptibility and progression. We find that both allele and SNP of IL-8–251AA are strongly associated with susceptibility of DR and correlated with progression of high-risk PDR. Our finding suggests that IL-8 is not only a DR-related biomarker but also a critical player in mediating and driving DR progression. Anti-IL-8 may become a promising target for developing novel therapeutic approach for DR and a sensitive DR-related gene marker for prognosis prediction.
Although good glycemic control is considered to be a mainstay in preventing vision loss caused by DR, some cases with inadequate glycemic control are surprisingly exempted from developing DR.40, 41 It suggests that genetic variation and predisposition may contribute to the variable progression and distinct prognosis to DR among T2D patients. We find that T allele of IP-10(-1596C/T) is protective factor to DR, supplies a genetic evidence for assessing the risk of DR. However, the finding that SNPs of IP-10(-1596) did not show any significant difference between NPDR and PDR groups implies the unique role of IP-10 as protective biomarker for DR. It suggests that IP-10(-1596C/T) is a promising biomarker but may not be a dominant player in determining DR progression. Our findings shed the lights on genetic susceptibility biomarkers screening, and IP-10 may also become a promising therapeutic target.
One of the limitations of our study is lacking the laboratory quantitation on animal model to further clarify current observation. In addition, an increased sample-size and long-term follow-up study would be necessary to confirm the association between these polymorphisms and DR. We expect to expand our observations about the IL-8 and IP-10 from other ethnic populations, which may help to further interpret the roles of these polymorphisms of IL-8 and IP-10 in mediating the progression of DR.
In conclusion, we examine the polymorphisms of IL-8–251T/A and IP-10–1596C/T in T2DR patients of northern China and find that that the IL-8–251 AA genotype and A allele were at a higher frequency for DR compared with DNR. However, T allele of IP-10–1596C/T had a lower frequency for DR compared with DNR, revealing a protective role of IP-10 in DR.

References
Resnikoff S, Pascolini D, Etya'ale D, Kocur I, Pararajasegaram R, Pokharel GP et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82: 844–851.
Petrovič D . Candidate genes for proliferative diabetic retinopathy. Biomed Res Int 2013; 2013: 540416.
Agardh E, Lundstig A, Perfilyev A, Volkov P, Freiburghaus T, Lindholm E et al. Genome-wide analysis of DNA methylation in subjects with type 1 diabetes identifies epigenetic modifications associated with proliferative diabetic retinopathy. BMC Med 2015; 13: 182.
Petrovic MG, Kruzliak P, Petrovic D . The rs6060566 of the reactive oxygen species modulator 1 (Romo-1) gene affects Romo-1 expression and the development of diabetic retinopathy in Caucasians with type 2 diabetes. Acta Ophthalmol 2015; 93 (8): e654–e657.
Abhary S, Hewitt AW, Burdon KP, Craig JE . A systematic meta-analysis of genetic association studies for diabetic retinopathy. Diabetes 2009; 58 (9): 2137–2147.
Petrovič MG, Korošec P, Košnik M, Hawlina M . Association of preoperative vitreous IL-8 and VEGF levels with visual acuity after vitrectomy in proliferative diabetic retinopathy. Acta Ophthalmol 2010; 88 (8): e311–e316.
Austeng D, Morken TS, Bolme S, Follestad T, Halsteinli V . Nurse-administered intravitreal injections of anti-VEGF: study protocol for noninferiority randomized controlled trial of safety, cost and patient satisfaction. BMC Ophthalmol 2016; 16 (1): 169.
Ach T, Hoeh AE, Ruppenstein M, Kretz FT, Dithmar S . Intravitreal bevacizumab in vascular pigment epithelium detachment as a result of subfoveal occult choroidal neovascularization in age-related macular degeneration. Retina 2010; 30 (9): 1420–1425.
Fine HF, Despotidis GD, Prenner JL . Ocular inflammation associated with antivascular endothelial growth factor treatment. Curr Opin Ophthalmol 2015; 26 (3): 184–187.
Hull J, Ackerman H, Isles K, Usen S, Pinder M, Thomson A et al. Unusual haplotypic structure of IL8, a susceptibility locus for a common respiratory virus. Am J Hum Genet 2001; 69: 413–419.
Matsushima K, Oppenheim JJ . Interleukin 8 and MCAF: novel inflammatory cytokines inducible by IL 1 and TNF. Cytokine 1989; 1: 2–13.
Baggiolini M, Walz A, Kunkel SL . Neutrophil-activating peptide-1/interleukin 8, a novel cytokine that activates neutrophils. J Clin Invest 1989; 84: 1045–1049.
Farber JM . Mig and IP-10: CXC chemokines that target lymphocytes. J Leukocyte Biol 1997; 62: 246–257.
Mukaida N, Harada A, Matsushima K . Interleukin-8 (IL-8) and monocyte chemotactic and activating factor (MCAF/MCP-1), chemokines essentially involved in inflammatory and immune reactions. Cytokine Growth Factor Rev 1998; 9: 9–23.
Elner SG, Elner VM, Jaffe GJ, Stuart A, Kunkel SL, Strieter RM . Cytokines in proliferative diabetic retinopathy and proliferative vitreoretinopathy. Curr Eye Res 1995; 14: 1045–1053.
Wang Y, Yang J, Gao Y, Du Y, Bao L, Niu W et al. Regulatory effect of e2, IL-6 and IL-8 on the growth of epithelial ovarian cancer cells. Cell Mol Immunol 2005; 2: 365–372.
Mizukami Y, Jo WS, Duerr EM, Gala M, Li J, Zhang X et al. Induction of interleukin-8 preserves the angiogenic response in HIF-1alpha-deficient colon cancer cells. Nat Med 2005; 11: 992–997.
Boldrini L, Gisfredi S, Ursino S, Lucchi M, Mussi A, Basolo F et al. Interleukin-8 in nonsmall cell lung carcinoma: relation with angiogenic pattern and p53 alterations. Lung Cancer 2005; 50: 309–317.
ZhangW Stoehlmacher J, Park DJ, Yang D, Borchard E, Gil J et al. Gene polymorphisms of epidermal growth factor receptor and its downstream effector, interleukin-8, predict oxaliplatin efficacy in patients with advanced colorectal cancer. Clin Colorectal Cancer 2005; 5: 124–131.
Itoh Y, Joh T, Tanida S, Sasakia Makoto, Kataokaa Hiromi, Itoha K et al. IL-8 promotes cell proliferation and migration through metalloproteinase-cleavage proHBEGF in human colon carcinoma cells. Cytokine 2005; 29: 275–282.
Angiolillo AL, Sgadari C, Taub DD, Liao F, Farber JM, Maheshwari S et al. Human interferon-inducible protein 10 is a potent inhibitor of angiogenesis in vivo. J Exp Med 1995; 182: 1301–1314.
Strieter RM, Kunkel SL, Arenberg DA, Burdick MD, Polverini PJ . Interferon ginducible protein 10 (IP-10), a member of the C-X-C chemokine family, is an inhibitor of angiogenesis. Biochem Biophys Res Commun 1995; 210: 51–57.
Ahluwalia TS, Khullar M, Ahuja M, Kohli HS, Bhansali A, Mohan V et al. Common variants of inflammatory cytokine genes are associated with risk of nephropathy in type 2 diabetes among Asian Indians. PLoS One 2009; 4: e5168.
Ruster C, Wolf G . The role of chemokines and chemokine receptors in diabetic nephropathy. Front Biosci 2008; 13: 944–955.
Hull J, Thomson A, Kwiatkowski D . Association of respiratory syncytial virus bronchiolitis with the interleukin 8 gene region in UK families. Thorax 2000; 55: 1023–1027.
Taguchi A, Ohmiya N, Shirai K, Mabuchi N, Itoh A, Hirooka Y et al. Interleukin-8 promoter polymorphism increases the risk of atrophic gastritis and gastric cancer in Japan. Cancer Epidemiol Biomarkers Prev 2005; 14: 2487–2493.
Ohyauchi M, Imatani A, Yonechi M, Asano N, Miura A, Iijima K et al. The polymorphism interleukin 8 –251 A/T influences the susceptibility of Helicobacter pylori related gastric diseases in the Japanese population. Gut 2005; 54: 330–335.
Deng G, Zhou G, Zhang R, Zhai Y, Zhao W, Yan Z et al. Regulatory polymorphisms in the promoter of CXCLl0 gene and disease progression in male hepatitis B virus carriers. Gastroenterology 2008; 2134: 716–726.
Dong L, Lv XY, Wang BJ, Wang YQ, Mu H, Feng ZL et al. Association of monocyte chemoattractant protein-1 (MCP-1)2518A/G polymorphism with proliferative diabetic retinopathy in northern Chinese type 2 diabetes. Graefes Arch Clin Exp Ophthalmol 2014; 252 (12): 1921–1926.
Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 1991; 98: 766–785.
Carmeliet P . Angiogenesis in health and disease. Nat Med 2003; 9: 653–660.
Calcutt NA, Cooper ME, Kern TS, Schmidt AM . Therapies for hyperglycaemia-induced diabetic complications: from animal models to clinical trials. Nat Rev Drug Discov 2009; 8: 417–429.
Brucklacher RM, Patel KM, Van Guilder HD, Bixler Georgina V, Barber Alistair J, Antonetti David A et al. Whole genome assessment of the retinal response to diabetes reveals a progressive neurovascular inflammatory response. BMC Med Genomics 2008; 1: 26.
Gubitosi-Klug RA, Talahalli R, Du Y, Nadler JL, Kern TS . 5-Lipoxygenase, but not 12/15-lioxygenase, contributes to degeneration of retinal capillaries in a mouse model of diabetic retinopathy. Diabetes 2008; 57: 1387–1393.
Krady JK, Basu A, Allen CM, Xu Y, LaNoue KF, Gardner TW et al. Minocycline reduces proinflammatory cytokine expression, microglial activation, and caspase-3 activation in a rodent model of diabetic retinopathy. Diabetes 2005; 54: 1559–1565.
Miyamoto K, Khosrof S, Bursell SE, Rohan R, Murata T, Clermont AC et al. Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proc Natl Acad Sci 1996; 96: 10836–10841.
Van Beijnum JR, Buurman WA, Griffioen AW . Convergence and amplification of toll-like receptor (TLR) and receptor for advanced glycation end products (RAGE) signaling pathways via high mobility group B1 (HMGB1). Angiogenesis 2008; 11: 91–99.
Elner VM, Strieter RM, Elner SG, Baggiolini M, Lindley I, Kunkel SL . Neutrophil chemotactic factor (IL-8) gene expression by cytokine treated retinal pigment epithelial cells. Am J Pathol 1990; 236: 745–750.
Bian ZM, Elner SG, Strieter RM, Glass MB, Lukacs NW, Kunkel SL et al. Glycated serum albumin induces chemokine gene expression in human retinal pigment epithelial cells. J Leukocyte Biol 1996; 60: 405–414.
The Diabetes Control and Complications Trial Research Group. The absence of a glycemic threshold for the development of long-term complications: the perspective of the Diabetes Control and Complications Trial. Diabetes 1996; 45: 1289–1298.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998; 352: 837–853.
Acknowledgements
NSFC (Grant No. 81201184), Heilongjiang Province Scientific Research Foundation (Grant No. LC2012C24), Foundation for the New Century Talents by the Educational Committee of Heilongjiang Province (Grant No. 1251–NCET–011). Support Program for Changjiang Scholars candidate (Grant No. 2014CJHB006), doctoral program of higher education research fund (Grant No. 20132307110027).
Author contributions
LD, JB, XJ, YZ carried out the experiment, data analysis and manuscript preparation. M-MY, DL and HZ were involved in experimental design, sample collection, grant and ethics applications, and manuscript preparation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Dong, L., Bai, J., Jiang, X. et al. The gene polymorphisms of IL-8(-251T/A) and IP-10(-1596C/T) are associated with susceptibility and progression of type 2 diabetic retinopathy in northern Chinese population. Eye 31, 601–607 (2017). https://doi.org/10.1038/eye.2016.287
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2016.287
This article is cited by
-
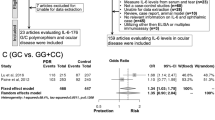
Association between diabetic retinopathy and polymorphisms of cytokine genes: a systematic review and meta-analysis
International Ophthalmology (2022)
-
Dynamic networks of P300-related process
Cognitive Neurodynamics (2022)
-
The role of inflammation in diabetic eye disease
Seminars in Immunopathology (2019)