Abstract
Aim
Bacterial keratitis results in corneal scarring and subsequent visual impairment. The long-term evolution of corneal scars has not been well described. In this case series, we identified patients who had improvement in corneal scarring and visual acuity from a clinical trial for bacterial keratitis.
Methods
We searched the records of the Steroids for Corneal Ulcers Trial (SCUT) for patients who had improvement in vision between the 3-month and 12-month visits and reviewed their clinical photographs.
Results
Of the 500 patients enrolled in SCUT, five patients with large central corneal scars due to bacterial keratitis are presented. All experienced improvement in rigid contact lens–corrected visual acuity from months 3 to 12. All patients also had marked improvement in corneal opacity during the same time period. None of the patients opted to have penetrating keratoplasty.
Conclusions
Corneal scars may continue to improve even many months after a bacterial corneal ulcer has healed. The corneal remodeling can be accompanied by considerable improvement in visual acuity, such that corneal transplantation may not be necessary.
Similar content being viewed by others
Introduction
Infectious keratitis is a significant cause of visual impairment worldwide, and many affected patients ultimately undergo surgical intervention.1, 2 The Steroids for Corneal Ulcers Trial (SCUT; clinicaltrials.gov #NCT00324168) investigated the safety and efficacy of corticosteroids in the treatment of bacterial corneal ulcers.3 In SCUT, visual acuity was assessed at 3 and 12 months after a patient presented with a corneal ulcer. We noticed that the corneal scars of some patients continued to resolve even after 3 months, which was often accompanied by improvement in vision. Here, we present a case series demonstrating that improvements in corneal scarring and visual acuity can continue even months after finishing treatment.
Methods
The SCUT trial was approved by the University of California, San Francisco Committee on Human Research and the Aravind Institutional Review Board.
The methodology and results of the SCUT trial have been reported previously.3, 4 Briefly, patients with culture-confirmed bacterial corneal ulcers were randomized to one of two treatment arms: topical antibiotic and prednisolone phosphate, 1%, or topical antibiotic and placebo. Best spectacle–corrected visual acuity was assessed at enrollment, months 3, and 12, and rigid contact lens–corrected visual acuity was assessed at months 3 and 12. Certified refractionists performed all visual acuity testing using a tumbling E chart. For this report, we identified patients with large central scars who had visual acuity improvement from months 3 to 12 and examined their clinical photographs.
Case reports
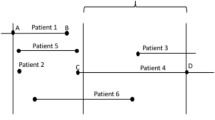
In SCUT, 404 of 500 subjects had visual acuity measured at months 3 and 12; of these, 127 had large scars (≥4 mm, measured as the geometric mean of the two longest perpendicular diameters) obscuring the entrance pupil at enrollment. Of these, 14 subjects had at least four lines of improvement in best contact lens–corrected visual acuity from months 3 to 12, of which 7 had a 12-month contact lens visual acuity better than logMAR 0.5 (20/63). Five of these study subjects had photographs at all time points and are presented here.
Serial corneal photographs of the five subjects at enrollment, 3, and 12 months are shown in Figure 1. At enrollment, each of the participants had a large central infiltrate and best spectacle–corrected visual acuity of counting fingers or worse. Corneal cultures were performed in all the study subjects and grew Streptococcus pneumoniae for subjects 1–4 and Pseudomonas aeruginosa for subject 5. All subjects were initially treated with moxifloxacin. Subjects 1 and 2 were treated with placebo eyedrops, and subjects 3–5 with prednisolone phosphate, 1% eyedrops. Each responded to topical therapy but developed a large corneal scar by 3 months after enrollment. Nonetheless, visual acuity improved markedly from enrollment to the 3-month visit (Table 1). Although the size of the corneal scars in these subjects generally did not change between the 3- and 12-month visits, the scars became markedly less dense during this follow-up period (Figure 1), and visual acuity continued to improve (Table 1). Rigid contact lenses improved vision in four of the five subjects at 3 months and in all the five subjects at 12 months (Table 1).
Discussion
In this case series, we demonstrate that a small fraction of severe corneal scars resulting from bacterial keratitis will show improvement in the density of opacity over time, with concurrent improvement in vision. None of the five patients in this series required corneal transplantation by 12 months after enrollment, which might not have been expected given the examination at 3 months.
Several mechanisms account for decreased vision following corneal scarring, including reduced corneal transparency, irregular astigmatism, and light scatter. However, various populations of myofibroblasts and fibroblasts are active during corneal stromal wound healing and may even restore corneal transparency.5 In this study, the serial photographs demonstrate that visual acuity impairment due to occlusion can improve over time, even long after the corneal ulcer has healed. In addition, if irregular astigmatism is estimated as the difference between spectacle corrected and contact lens corrected visual acuity, then four of the five patients in this series had smaller amounts of irregular astigmatism at the 12-month visit compared with the 3-month visit. Therefore, both scar opacity and irregular astigmatism may improve after the first 3 months following a large, central corneal ulcer.
The chief limitation of this case series is that the observations represent a minority of bacterial ulcer patients and therefore may not be generalizable to all corneal ulcers. However, the series does demonstrate that at least some corneal ulcer scars—even large centrally located scars—will continue to improve many months after the initial infection. It may be prudent to delay corneal transplantation in patients with good vision in the contralateral eye, as surgical visual rehabilitation may not ultimately be necessary. Further follow up of the SCUT study participants will provide additional insight regarding longer-term visual acuity outcomes and corneal scar remodeling.

References
Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP et al. Global data on visual impairment in the year 2002. Bull World Health Organ 2004; 82: 844–851.
Gopinathan U, Sharma S, Garg P, Rao GN . Review of epidemiological features, microbiological diagnosis and treatment outcome of microbial keratitis: experience of over a decade. Indian J Ophthalmol 2009; 57: 273–279.
Srinivasan M, Mascarenhas J, Rajaraman R, Ravindran M, Lalitha P, Glidden DV et al. Corticosteroids for bacterial keratitis: the Steroids for Corneal Ulcers Trial (SCUT). Arch Ophthalmol 2012; 130: 143–150.
Srinivasan M, Mascarenhas J, Rajaraman R, Ravindran M, Lalitha P, Glidden DV et al. The steroids for corneal ulcers trial: study design and baseline characteristics. Arch Ophthalmol 2012; 130: 151–157.
Hassell JR, Birk DE . The molecular basis of corneal transparency. Exp Eye Res 2010; 91: 326–335.
Acknowledgements
The trial was funded by National Eye Institute Grant U10 EY015114 (TML). Support was also provided by National Eye Institute Grants K23 EY017897 (NRA) and K23 EY019071 (JDK), and career development awards from Research to Prevent Blindness (NRA and JDK).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
McClintic, S., Srinivasan, M., Mascarenhas, J. et al. Improvement in corneal scarring following bacterial keratitis. Eye 27, 443–446 (2013). https://doi.org/10.1038/eye.2012.270
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2012.270
Keywords
This article is cited by
-
Sustained release of decorin to the surface of the eye enables scarless corneal regeneration
npj Regenerative Medicine (2018)