Abstract
Aim:
Silibinin is known to exert growth inhibition and cell death together with cell cycle arrest and apoptosis in human prostate cancer cells. Whether silibinin could inhibit the invasion, motility and migration of prostate cancer cells remains largely unknown. This study was designed to evaluate this efficacy and possible mechanisms using a novel highly bone metastatic ARCaPM cell model.
Methods:
Four prostate cancer cell lines, LNCaP, PC-3, DU145, and ARCaPM, were used in this study. These cells were treated with increasing concentrations of silibinin (50, 100, and 200 μmol/L) for different periods of time. After treatment, cell viabilities of four prostate cancer cells were compared by MTT assay. Alterations of ARCaPM cell invasion, motility and migration were assessed by cell invasion, motility and wound healing assays. The changes of vimentin expression were observed by Western blotting and immunofluorescence staining, and the expression of MMP-2, MMP-9, and uPA was analyzed by reverse transcription-polymerase chain reaction (RT-PCR).
Results:
ARCaPM cells showed less sensitivity to the growth inhibition of pharmacological doses of silibinin than LNCaP, PC-3, and DU145 cells. However, silibinin exerted significant dose- and time-dependent inhibitory effects on the invasion, motility and migration of ARCaPM cells. Furthermore, the expression of vimentin and MMP-2, but not MMP-9 or uPA, was down-regulated in a dose- and time-dependent manner after treatment of silibinin.
Conclusion:
This study shows that silibinin could inhibit the invasion, motility and migration of ARCaPM cells via down-regulation of vimentin and MMP-2 and therefore may be a promising agent against prostate cancer bone metastasis.
Similar content being viewed by others
Introduction
Prostate cancer is one of the most commonly diagnosed cancers and the second leading cause of death in men in Western countries1. Surgical and hormonal therapies have shown beneficial effects for early-stage, hormone-responsive disease. However, few treatment options are available for more aggressive hormone-independent or hormone-refractory prostate cancer that is resistant to chemotherapy and radiotherapy2. Therefore, more effort must be devoted to developing novel agents that target these unique characteristics of prostate cancer. In this regard, several nontoxic phytochemicals, including silibinin, have shown promising therapeutic and preventive efficacy against prostate cancer3.
Silibinin, the major active constituent of silymarin isolated from milk thistle (Silybum marianum), has shown strong anticancer efficacy against both androgen-dependent and androgen-independent prostate cancer. This phytochemical is currently being used in a phase I/II clinical trial for treatment of prostate cancer4. Silibinin inhibited the proliferation of human prostate cancer LNCaP, PC-3, and DU145 cells in vitro, and oral silibinin suppressed the growth of PC-3 and DU145 xenografts in nude mice and transgenic adenocarcinoma of mouse prostate (TRAMP) in vivo5, 6, 7, 8, 9, 10. Extensive studies have shown the multi-targeted molecular mechanisms underlying therapeutic actions of silibinin in prostate cancer, and silibinin could target the IGF1-IGFBP3 axis and the cyclin-dependent kinase (CDK)-cyclin-CDK inhibitor axis to inhibit cell proliferation, as well as activate the caspase pathway to induce apoptosis5, 6, 7, 8, 9, 10. In addition, several recent studies have also shown the anti-metastatic activities of silibinin in prostate cancer. It has been reported that silibinin could exert inhibitory effects on the viability, motility and adhesion of PC-3 cells in vitro11, and inhibit tumor growth, progression, local invasion, and distant metastasis involving suppression of tumor angiogenesis and epithelial-mesenchymal transition in the TRAMP mouse model12. However, the mechanisms by which silibinin exerts its anti-metastatic effects are largely unknown.
The propensity of prostate cancer to skeletal metastases is well recognized, and most patients who die from prostate cancer have metastatic bone disease13. The ARCaP model was established from the ascites fluid of a patient with metastatic prostate cancer and could represent a continuum of prostate cancer progression closely mimicking the pathophysiology of advanced and lethal clinic human prostate cancer bone metastasis. ARCaPM, a derivative ARCaP cell subclone, exhibited a spindle-shaped mesenchymal morphology with increased cell motility, invasion and migration in vitro. Furthermore, ARCaPM cells displayed a predilection to metastasize to various bone sites with increased incidence rates and shorter latency periods in SCID mice14. Thus, this cell model appears appropriate for screening and developing new therapeutic agents against prostate cancer bone metastasis. In this study, we evaluated the anti-metastatic activities of silibinin in prostate cancer using this unique model and explored its underlying molecular mechanisms by detecting several key molecules related to cancer invasion and metastasis, such as vimentin, matrix metalloproteinase-2 (MMP-2), matrix metalloproteinase-2 (MMP-9) and urokinase-type plasminogen activator (uPA).
Materials and methods
Cell culture and silibinin treatment
Human prostate cancer cells LNCaP, PC-3, DU145 and ARCaPM provided by Prof Leland WK Chung (Emory University School of Medicine, Atlanta, GA, USA) were maintained in RPMI 1640 or DMEM (Gibco, San Diego, CA, USA) supplemented with 10% (v/v) fetal bovine serum (FBS, Sijiqing, Hangzhou, China) at 37 °C in a humidified 5% CO2 incubator. For silibinin treatment, appropriate volumes of stock solution (0.05 mol/L in DMSO) of silibinin (both from Sigma, St Louis, MO, USA) were added to the medium to achieve the indicated concentrations (50, 100, and 200 μmol/L) and were then incubated with cells for the indicated periods of time (24, 48, 72, and 96 h).
Determination of cell viability by MTT assay
To compare the sensitivities of different prostate cancer cells to silibinin treatment, 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT, Sigma, St Louis, MO, USA) proliferation assays were performed to determine cell viability. Four prostate cancer cells were seeded at the density of 1×103 cells/well in 96-well plates for 24 h, and then fed fresh medium and treated with various doses of silibinin (50, 100, and 200 μmol/L) for 24, 48, 72, and 96 h. After the exposure period, 20 μL MTT (5 mg/mL in PBS) was added to each well for 4 h incubation at 37 °C in 5% CO2. Thereafter, the medium containing MTT was removed and 150 μL DMSO was added to solubilize the formazan crystals. The absorbance (OD) was then measured at a wavelength of 590 nm by a Microplate Autoreader (Bio-Tek Instruments, VT, USA). The growth inhibitory rate was calculated by the following formula: growth inhibitory rate=(average OD value in the control group–average OD value in the treatment group)/average OD value in the control group×100%.
Cell invasion and motility assays
For cell invasion assays15, ARCaPM cells were treated with silibinin (50, 100, and 200 μmol/L) for 24, 48, and 72 h, and then cells were harvested and their in vitro invasiveness was determined using a Transwell chamber (Corning, NY, USA). Matrigel (Sigma, St Louis, MO, USA) was diluted by serum-free medium to a final concentration of 2 mg/mL, and 8 μm pore polycarbonate membrane filters were coated with 50 μL of Matrigel. Treated cells were then seeded into the upper chamber with 5×103 cells/well in 100 μL of serum-free medium, and 1 ml medium containing 20% FBS was added to the lower chamber as a chemoattractant. After incubation for 48 h at 37 °C in 5% CO2, the Matrigel coating on the upper surface of the filter was wiped with a cotton swab. Cells that invaded to the lower surface of the filter were fixed by 4% paraformaldehyde and stained with Giemsa. Cell numbers were counted in three random fields (×100) per filter. The cell motility assay was conducted with 2.5×103 cells/well in a similar fashion in a Transwell chamber without coating Matrigel.
Wound healing assay
To determine the effect of silibinin on migration of ARCaPM cells in vitro, cells were seeded at a density of 5×105 cells in 60 mm-dishes and grew to about 90% confluence after 48 h. Medium was removed and cell monolayers were wounded by manually scraping the cells with a 1 ml plastic pipette tip. Debris was removed from the culture by washing with PBS twice, and cells were then cultured with fresh medium containing silibinin at different concentrations for 24, 48, and 72 h. Images were captured immediately after wounding and 24 h post wounding, and wound closure was monitored with a UOP DSZ500X inverted microscope (UOP Microscope, Chongqing, China). Wound sizes were verified with the scale of the images to ensure that all wounds were the same width at the beginning. The migration distance and migration inhibitory rate were calculated by the following formula: migration distance=(wound width at the beginning–wound width after treatment)/2 (μm); migration inhibitory rate=(average migration distance in the control group–average migration distance in the treatment group)/average migration distance in the control group×100%.
Western blotting analysis
After the indicated silibinin treatment, the medium was removed and ARCaPM cells were washed with cold PBS twice; then, total cellular protein lysates were prepared with RIPA buffer [50 mmol/L Tris (pH 8.0), 150 mmol/L NaCl, 0.1% SDS, 1% NP40 and 0.5% sodium deoxycholate] containing proteinase inhibitors (1% Cocktail and 1 mmol/L PMSF, both from Sigma, St Louis, MO, USA). A total of 30 μg of protein was separated by 12% SDS-PAGE and transferred to nitrocellulose membranes. The membranes were blocked at room temperature for 1 h with 5% skim milk in Tris-buffered saline with 0.1% Tween 20 (pH 7.6, TBST). Monoclonal vimentin antibody (V9, Santa Cruz, CA, USA) was applied at 1:2000 dilutions by 5% skim milk in TBST at room temperature for 1.5 h. After being washed with TBST, membranes were incubated with secondary antibodies coupled to horseradish peroxidase at room temperature for 1 h and visualized with a ECL chemiluminescent detection system (Pierce, Rockford, IL, USA). Loading differences were normalized using a monoclonal GAPDH antibody. The mean density for each band was analyzed using Glyko BandScan software (Glyko, Novato, USA).
Immunofluorescence staining
After the indicated silibinin treatment, ARCaPM cells on coverslips were washed with PBS and fixed in 4% paraformaldehyde for 20 min. Cells were permeabilized with PBS containing 0.25% Triton X-100 for 30 min and blocked with horse serum for 20 min. Cells were then incubated with a 1:1000 dilution of monoclonal vimentin antibody in PBS buffer containing 10% bovine serum overnight at 4 °C and washed and incubated with a 1:200 dilution of TRITC conjugated anti-mouse IgG. The specimens were observed under Olympus IX-50 fluorescence inverted microscope (Olympus, Tokyo, Japan).
Reverse transcription-polymerase chain reaction (RT-PCR)
After the indicated silibinin treatment, total RNA was isolated from ARCaPM cells using Trizol reagent (Invitrogen, Carlsbad, CA, USA) and quantitated by absorbance at 260 nm. The RNA (2 μg) was reverse transcribed using RevertAidTM First Strand cDNA Synthesis Kit (MBI Fermentas, St Leon-Rot, Germany) according to the manufacturer's instructions. All PCR analyses were subsequently performed with 2 μL of the cDNA reaction utilizing conditions as follows: 94 °C, 5 min, 32 cycles of 94 °C, 30 s; 58 °C, 30 s; 72 °C, 45 s. Reactions were finished with 72 °C, 7 min extension. Primers were used for MMP-2, MMP-9, uPA, and β-actin: MMP-2 (475 bp): 5′-GGCCCTGTCACTCCTGAGAT-3′ (forward) and 5′-GGCATCCAGGTTATCGGGGA-3′ (reverse); MMP-9 (482 bp): 5′-CAACATCACCTATTGGATCC-3′ (forward) and 5′-CGGGTGTAGAGTCTCTCGCT-3′ (reverse); uPA (348 bp): 5′-TTGCGGCCATCTACAGGAG-3′ (forward) and 5′-ACTGGGGATCGTTATACATC-3′ (reverse); β-actin (318 bp): 5′-ATCATGTTTGAGACCTTCAACA-3′ (forward) and 5′-CATCTCTTGCTCGAAGTCCA-3′ (reverse). PCR products were analyzed by 2% agarose gel electrophoresis and visualized using ethidium bromide staining. The mean density for each band was also analyzed using Glyko BandScan software.
Statistical analysis
All assays were repeated in triplicate in three independent experiments, and all data were expressed as means±SEM. Analysis of variance (ANOVA) for multiple comparisons was used as noted. In all cases, P<0.05 was considered significant. All statistical tests were performed with statistical analysis software (SPSS, Chicago, IL, USA).
Results
Decreased sensitivity of ARCaPM cells to growth inhibition by silibinin
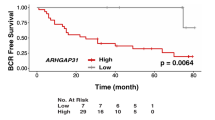
We exposed four human prostate cancer cell lines (LNCaP, PC-3, DU145, and ARCaPM) to increasing concentrations of silibinin for different time periods and compared their relative sensitivities to the growth inhibition of silibinin by MTT assay. These cells displayed marked heterogeneity in responsiveness. Consistent with the previous data5, 6, 7, silibinin significantly inhibited the cell proliferation of LNCaP, PC-3, and DU145 cells in a dose- and time-dependent manner, whereas it had a weaker inhibitory effect on the cell viability of ARCaPM cells (Figure 1). In dose-dependent experiments, the lower dose of 50 μmol/L silibinin could reduce the cell viabilities of LNCaP, PC-3, and DU145 cells by 18.5%, 26.7%, and 15.0%, respectively, whereas only 0.7% growth inhibition was observed in ARCaPM cells after 48 h of treatment. Even at a concentration as high as 200 μmol/L, only 18.5% growth inhibition was observed in ARCaPM cells, but 48.7%, 60.0%, and 73.8% in LNCaP, PC-3, and DU145 cells, respectively (Figure 1A). Similarly, in time-course experiments, 100 μmol/L silibinin treatment for 24 h led to 24.8%, 21.8%, and 27.3% growth inhibition of LNCaP, PC-3, and DU145 cells, respectively, but only 5.3% of ARCaPM cells. The growth inhibition reached its maximum at 96 h, and 100 μmol/L silibinin treatments resulted in 47.2%, 71.3%, and 41.1% growth inhibition of LNCaP, PC-3, and DU145 cells, respectively, but only 22.2% of ARCaPM cells (Figure 1B). These data indicated that highly metastatic ARCaPM cells were less sensitive to growth inhibition by silibinin than LNCaP, PC-3, and DU145 cells.
Different sensitivities of prostate cancer cell lines to growth inhibition by silibinin. After cells were treated with the indicated doses of silibinin (50, 100, and 200 μmol/L) for 24, 48, 72, and 96 h, cell viabilities were determined by MTT assay. (A) Different growth inhibition of LNCaP, PC-3, DU145, and ARCaPM cells to silibinin in a dose-dependent manner. (B) Different growth inhibition of LNCaP, PC-3, DU145, and ARCaPM cells to silibinin in a time-dependent manner. The data shown are means±SEM of three independent experiments. bP<0.05 compared with LNCaP, PC-3, and DU145 cells.
Inhibition on invasion, motility and migration of ARCaPM cells by silibinin
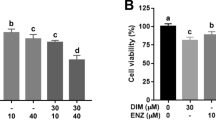
Using a Transwell chamber coated with or without Matrigel, we found that silibinin could significantly reduce the invasion and motility of ARCaPM cells (Figure 2). As low as 37% of the invasive capability and 50% of motility capability were retained after 100 μmol/L silibinin treatment for 48 h (Figure 2A). Moreover, this tremendous inhibitory effect occurred in a dose- and time-dependent manner. Different concentrations of silibinin (50, 100, and 200 μmol/L) after 48 h treatment reduced the invasion of ARCaPM by 15%, 63%, and 92% and reduced the motility by 20%, 50%, and 25% (Figure 2B). As such, 100 μmol/L silibinin for 24, 48, and 72 h reduced the invasion of ARCaPM cells by 41%, 53%, and 87.5%, respectively, and reduced the motility by 35%, 50%, and 75%, respectively (Figure 2C).
Dose- and time-dependent inhibitory effects of silibinin on the invasion and motility of ARCaPM cells. ARCaPM cells were treated with different concentrations of silibinin (50, 100, and 200 μmol/L) for 24, 48, and 72 h and then harvested and seeded into the upper chamber, either coated or uncoated with Matrigel. The number of cells that invaded or moved into the lower chamber represented the invasion and motility capabilities. (A) Invasion and motility inhibition of ARCaPM cells after 100 μmol/L silibinin treatment for 48 h (magnification×100). (B and C) Silibinin inhibited the invasion and motility of ARCaPM cells in a dose- and time-dependent manner. Data represent means±SEM of three independent experiments.
Additionally, we also obtained similar results in a wound healing assay. Silibinin inhibited migration in vitro for ARCaPM cells (Figure 3). After treatment with 200 μmol/L silibinin for 72 h, the cells remained creviced, whereas the wounds with mock treatment healed completely (Figure 3A). This inhibitory effect was dose- and time-dependent (Figure 3B). In a quantitative analysis, different concentrations of silibinin (50, 100, and 200 μmol/L) after 24 h treatment reduced the migration of ARCaPM cells by 45%, 70.1%, and 85%, respectively. Similarly, after 72 h of treatment with 50, 100, and 200 μmol/L silibinin, 30.6%, 47.2%, and 69.4% inhibition of migration was observed in ARCaPM cells. Our results strongly suggest that pharmacological doses of silibinin could lead to significant inhibition of invasion, motility and migration of ARCaPM cells.
Dose- and time-dependent inhibitory effects of silibinin on migration of ARCaPM cells in vitro. The confluent ARCaPM monolayers were wounded by scraping and treated with silibinin (50, 100, and 200 μmol/L). Cell migration to the wound surface was monitored after 24, 48, and 72 h. A representative image is shown (magnification×100), and the average migration distances of the wound edge in three independent experiments are quantitated below the photograph data. Bar represents 200 μm.
Silibinin inhibits vimentin and MMP-2 expression in ARCaPM cells
To elucidate the possible underlying mechanisms of anti-metastatic activities of silibinin on ARCaPM cells, we detected changes in vimentin, MMP-2, MMP-9, and uPA expression by Western blotting, immunofluorescence staining and RT-PCR. As shown in Figure 4, Western blotting revealed silibinin treatment significantly decreased the expression of vimentin in a dose- and time-dependent manner when GAPDH served as a loading control (Figure 4A and 4B). Treatment with 50, 100, and 200 μmol/L of silibinin after 24 h showed 32.4%, 54.9%, and 79% decreases in vimentin protein compared with controls; 100 μmol/L silibinin treatment for 24, 48, and 72 h showed 58.6%, 74.3%, and 86.9% decreases in vimentin protein. Furthermore, we observed the similar decreasing tendency of vimentin in the cytoplasm after 100 μmol/L silibinin treatment by immunofluorescence staining (Figure 4C). In addition, 100 μmol/L silibinin treatment for 24, 48, and 72 h decreased MMP-2 mRNA by 42.3%, 34.5%, and 33.3%, but had no significant effects on MMP-9 and uPA mRNA expression when β-actin served as a loading control (Figure 4D). Together, these findings suggest that down-regulation of vimentin and MMP-2 might be involved in the inhibition of invasion, motility and migration of ARCaPM cells after silibinin treatment.
Inhibitory effects of silibinin on the expression of vimentin and MMP-2 in ARCaPM cells. (A and B) Cells were treated with the indicated doses of silibinin (50, 100, and 200 μmol/L) for 24, 48, and 72 h, and then cell lysates were subjected to SDS-PAGE followed by Western blotting. Membranes were probed for vimentin protein levels, and GAPDH served as a loading control. Quantitative results were quantitated below the gel data. (C) Cells were treated with DMSO (control) or 100 μmol/L silibinin for 24 h, and the change of vimentin expression was evaluated by immunofluorescence staining (magnification×200). (D) Cells were treated with 100 μmol/L silibinin for 24, 48, and 72 h, and then total mRNA was subjected to RT-PCR for analyzing the changes of MMP-2, MMP-9, and uPA expression. β-actin served as a loading control. Quantitative analyses are shown below the gel data. Data represent means±SEM of three independent experiments. bP<0.05 compared with control.
Discussion
In this study, utilizing a well-characterized prostate cancer cell line, we have demonstrated a novel anticancer effect of silibinin and provided possible mechanisms that are responsible for its anti-metastatic effect in vitro.
The anti-proliferative effect of silibinin has been well documented in the androgen-dependent and androgen-independent prostate cancer LNCaP, 22Rv1, PC-3, and DU145 cell lines, and studies have shown that silibinin could inhibit the growth of prostate cancer by inducing cell cycle arrest or caspase-dependent apoptosis5, 6, 7. In agreement with previous studies, we also observed strong inhibitory effects of silibinin on LNCaP, PC-3, and DU145 cell proliferation, whereas ARCaPM cells showed a much weaker response to the anti-proliferative effect of silibinin. As a derivative subclone from androgen-repressed prostate cancer, Xu et al have demonstrated that ARCaPM cells exhibited an aggressive mesenchymal phenotype, which was fast-growing and more resistant to chemotherapeutic drugs, such as doxorubicin, etoposide and paclitaxel14. Here, we revealed that ARCaPM cells showed stronger resistance to growth inhibition following silibinin treatment.
Several studies have silibinin might represent a potential anti-metastatic agent inhibiting cancer cell invasion and motility, and this efficacy has been demonstrated in A549 lung cancer cells, SCC-4 tongue cancer cells, osteosarcoma MG-63 cells and MCF-7 breast cancer cells16, 17, 18, 19, 20. Recently, it has been reported that silibinin exerts inhibitory effects by silibinin on viability, migration and adhesion of androgen-independent PC-3 cells, such that α2β1-integrin may be the target11. Singh et al also found that silibinin treatment inhibited prostate tumor growth, progression, local invasion and distant metastasis using the TRAMP mouse model12. Here, we are the first to show that pharmacological doses of silibinin may exert inhibitory effects on the invasion, motility and migration of ARCaPM cells in a dose- and time-dependent manner.
To investigate the molecular effects of silibinin treatment on ARCaPM cells, we further analyzed the alterations of several molecules related to cancer invasion and metastasis, such as vimentin, MMP-2, MMP-9, and uPA. Vimentin is a mammalian structural cytoskeletal protein constituting type III mesenchymal filaments, and its elevated and aberrant expression correlates well with up-regulated cell invasion or migration both in the embryo and in malignancy21. Several studies have shown that vimentin could affect the invasion and motility of prostate cancer cells and is a promising marker for predicting aggressive and metastatic prostate cancer22, 23. Consistent with their highly metastatic features, ARCaPM cells display higher expression of vimentin and other mesenchymal markers14. Here, it was demonstrated that silibinin markedly decreased vimentin protein expression in a dose- and time-dependent manner. Similar results were reported in Singh's findings, which revealed anti-metastatic activities of silibinin in TRAMP mice together with a concomitant strong decrease in the level of vimentin12.
In addition, we found silibinin significantly suppressed MMP-2 expression, but not MMP-9 or uPA in ARCaPM cells. MMPs are known proteolytic enzymes that degrade the extracellular matrix and basement membrane of cells, and MMP-2 and MMP-9 are the most vital enzymes for degradation24, 25. Therefore, they are considered major factors in tumor invasion and metastasis. uPA, which is an upstream enzyme of MMPs, might activate a series of protein degradation reactions to regulate or activate MMPs26. A series of studies demonstrated that silibinin could inhibit invasion and motility of A549 cells and SCC-4 cells by down-regulating MMP-2 and uPA and up-regulating tissue inhibitor of metalloproteinase-2 (TIMP-2) and PAI-1 expressions16, 17. Moreover, in A549 lung cancer cells, silibinin inhibited MMP-2 and uPA expression through reducing ERK1/2 and Akt phosphorylation18. In human osteosarcoma MG-63 cells, silibinin inhibited uPA and MMP-2 expressions, IL-6-induced ERK1/2 and c-Jun phosphorylation, and cell invasiveness19. In addition, silibinin also reduced PMA-induced invasion of MCF-7 breast cancer cells through the specific inhibition of AP-1-dependent MMP-9 gene expression20. In our studies, we observed a suppression effect of silibinin on MMP-2 expression, but not MMP-9 or uPA in ARCaPM cells. Thus, it is possible that silibinin could suppress prostate cancer invasion and metastasis through the inhibition of vimentin and MMP-2 expression.
In conclusion, here we are the first to demonstrate a novel mechanism by which silibinin acts as an anti-metastatic agent via inhibiting invasion, motility and migration in novel, highly bone metastatic ARCaPM cells by down-regulating the vimentin and MMP-2 expression. Furthermore, we will use nude mice to verify the in vivo anti-metastatic effects of silibinin in human prostate cancer and explore additional molecular mechanisms of silibinin on prostate cancer bone metastasis.
Author contribution
Kai-jie WU, Jin ZENG, and Da-lin HE designed this research; Kai-jie WU, Guo-dong ZHU, Lin-lin ZHANG, and Dong ZHANG performed this research, Lei LI, Jin-hai FAN, and Xin-yang WANG contributed new analytical tools and reagents; Kai-jie WU and Jin ZENG analyzed data, wrote and revised the paper.
References
Landis SH, Murray T, Bolden S, Wingo PA . Cancer statistics, 1999. CA Cancer J Clin 1999; 49: 8–31.
Feldman BJ, Feldman D . The development of androgen-independent prostate cancer. Nat Rev Cancer 2001; 1: 34–45.
Surh YJ . Cancer chemoprevention with dietary phytochemicals. Nat Rev Cancer 2003; 3: 768–80.
Singh RP, Agarwal R . Prostate cancer prevention by Silibinin. Curr Cancer Drug Targets 2004; 4: 1–11.
Tyagi A, Agarwal C, Agarwal R . Inhibition of retinoblastoma protein (Rb) phosphorylation at serine sites and an increase in Rb-E2F complex formation by silibinin in androgen-dependent human prostate carcinoma LNCaP cells: role in prostate cancer prevention. Mol Cancer Ther 2002; 1: 525–32.
Deep G, Singh RP, Agarwal C, Kroll DJ, Agarwal R . Silymarin and silibinin cause G1 and G2-M cell cycle arrest via distinct circuitries in human prostate cancer PC-3 cells: a comparison of flavanone silibinin with flavanolignan mixture silymarin. Oncogene 2006; 25: 1053–69.
Zi X, Grasso AW, Kung HJ, Agarwal R . A flavonoid antioxidant, silymarin, inhibits activation of erbB1 signaling and induces cyclin-dependent kinase inhibitors, G1 arrest, and anticarcinogenic effects in human prostate carcinoma DU145 cells. Cancer Res 1998; 58: 1920–9.
Singh RP, Deep G, Blouin MJ, Pollak MN, Agarwal R . Silibinin suppresses in vivo growth of human prostate carcinoma PC-3 tumor xenograft. Carcinogenesis 2007; 28: 2567–74.
Singh RP, Dhanalakshmi S, Tyagi AK, Chan DC, Agarwal C, Agarwal R . Dietary feeding of silibinin inhibits advance human prostate carcinoma growth in athymic nude mice and increases plasma insulin-like growth factor-binding protein-3 levels. Cancer Res 2002; 62: 3063–9.
Raina K, Blouin MJ, Singh RP, Majeed N, Deep G, Varghese L, et al. Dietary feeding of silibinin inhibits prostate tumor growth and progression in transgenic adenocarcinoma of the mouse prostate model. Cancer Res 2007; 67: 11083–91.
Mokhtari MJ, Motamed N, Shokrgozar MA . Evaluation of silibinin on the viability, migration and adhesion of the human prostate adenocarcinoma (PC-3) cell line. Cell Biol Int 2008; 32: 888–92.
Singh RP, Raina K, Sharma G, Agarwal R . Silibinin inhibits established prostate tumor growth, progression, invasion, and metastasis and suppresses tumor angiogenesis and epithelial-mesenchymal transition in transgenic adenocarcinoma of the mouse prostate model mice. Clin Cancer Res 2008; 14: 7773–80.
Boring CC, Squires TS, Tong T, Montgomery S . Cancer statistics, 1994. CA Cancer J Clin 1994; 44: 7–26.
Xu J, Wang R, Xie ZH, Odero-Marah V, Pathak S, Multani A, et al. Microenvironment in promoting epithelial to mesenchymal transition and increased bone and adrenal gland metastasis. Prostate 2006; 66: 1664–73.
Attiga FA, Fernandez PM, Weeraratna AT, Manyak MJ, Patierno SR . Inhibitors of prostaglandin synthesis inhibit human prostate tumor cell invasiveness and reduce the release of matrix metalloproteinases. Cancer Res 2000; 60: 4629–37.
Chu SC, Chiou HL, Chen PN, Yang SF, Hsieh YS . Silibinin inhibits the invasion of human lung cancer cells via decreased productions of urokinase-plasminogen activator and matrix metalloproteinase-2. Mol Carcinogen 2004; 40: 143–9.
Chen PN, Hsieh YS, Chiang CL, Chiou HL, Yang SF, Chu SC . Silibinin inhibits invasion of oral cancer cells by suppressing the MAPK pathway. J Dent Res 2006; 85: 220–5.
Chen PN, Hsieh YS, Chiou HL, Chu SC . Silibinin inhibits cell invasion through inactivation of both PI3K-Akt and MAPK signaling pathways. Chem-Biol Interact 2005; 156: 141–50.
Hsieh YS, Chu SC, Yang SF, Chen PN, Liu YC, Lu KH . Silibinin suppresses human osteosarcoma MG-63 cell invasion by inhibiting the ERK-dependent c-Jun/AP-1 induction of MMP-2. Carcinogenesis 2007; 28: 977–87.
Lee SO, Jeong YJ, Im HG, Kim CH, Chang YC, Lee IS . Silibinin suppresses PMA-induced MMP-9 expression by blocking the AP-1 activation via MAPK signaling pathways in MCF-7 human breast carcinoma cells. Biochem Biophys Res Commun 2007; 354: 165–71.
Kokkinos MI, Wafai R, Wong MK, Newgreen DF, Thompson EW, Waltham M . Vimentin and epithelial to mesenchymal transition in human breast cancer: observations in vitro and in vivo. Cells Tissues Organs 2007; 185: 191–203.
Zhao Y, Yan Q, Long X, Chen X, Wang Y . Vimentin affects the mobility and invasiveness of prostate cancer cells. Cell Biochem Funct 2008; 26: 571–7.
Lang SH, Hyde C, Reid IN, Hitchcock IS, Hart CA, Bryden AA, et al. Enhanced expression of Vimentin in motile prostate cancer cell lines and in poorly differentiated and metastatic prostate carcinoma. Prostate 2002; 52: 253–63.
Nelson AR, Fingleton B, Rothenberg ML, Matrisian LM . Matrix metalloproteinases: biologic activity and clinical implications. J Clin Oncol 2000; 18: 1135–49.
Chambers AF, Matrisian LM . Changing views of the role of matrix metalloproteinases in metastasis. J Natl Cancer Inst 1997; 89: 1260–70.
Lijnen HR . Matrix metalloproteinases and cellular fibrinolytic activity. Biochemistry 2002; 67: 92–8.
Acknowledgements
This project is supported in part by the National 863 project of China (No 2006AA020705). We thank Prof Jin-tang DONG (Emory University School of Medicine, Atlanta, GA, USA) and Jer-Tsong HSIEH (University of Texas Southwestern Medical Center, Dallas, TX, USA) for their helpful discussion and support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, Kj., Zeng, J., Zhu, Gd. et al. Silibinin inhibits prostate cancer invasion, motility and migration by suppressing vimentin and MMP-2 expression. Acta Pharmacol Sin 30, 1162–1168 (2009). https://doi.org/10.1038/aps.2009.94
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.94
Keywords
This article is cited by
-
Pharmacoproteomic analysis reveals that metapristone (RU486 metabolite) intervenes E-cadherin and vimentin to realize cancer metastasis chemoprevention
Scientific Reports (2016)
-
Real-time analysis of epithelial-mesenchymal transition using fluorescent single-domain antibodies
Scientific Reports (2015)
-
Prostatakarzinomprophylaxe durch Nahrungsergänzungsmittel
Der Urologe (2014)
-
The role of epithelial plasticity in prostate cancer dissemination and treatment resistance
Cancer and Metastasis Reviews (2014)
-
Discovery and identification of PIM-1 kinase inhibitors through a hybrid screening approach
Molecular Diversity (2014)