Abstract
Study design:
In vitro studies using isolated guinea pig spinal cord white matter.
Objectives:
To determine whether lack of oxygen can cause irreversible impairment of electrical impulse conduction.
Setting:
Department of Basic Medical Sciences, Purdue University, West Lafayette, Indiana, USA.
Methods:
The hypoxic injury was induced by reducing the oxygen tension of the perfused solution by 80%. Compound action potentials (CAPs) were monitored before, during, and after oxygen deprivation.
Results:
We have found that 60 min of hypoxia reduced the conduction to 30% of preinjury level and recovered to approximately 60% of the preinjury level upon reoxygenation. Larger axons appeared to be more vulnerable to oxygen deprivation. We noted a significant decrease and recovery of the depolarizing afterpotential (DAP). Likewise, there was a delay and recovery of absolute and relative refractory period. Concomitantly, the ability of axons to follow repetitive stimuli was suppressed following oxygen deprivation but recovered upon reoxygenation.
Conclusion:
Following 60 min of oxygen deprivation and 30 min of reoxygenation, mammalian spinal cord white matter can partially recover electrical impulse conduction. However, within the same period, cords gained a complete recovery of other electrical properties, such as the depression of DAP, the delaying of refractory period, and the decreased ability to respond to repetitive stimuli. Compared to previous findings when both oxygen and glucose were deprived, we conclude that glucose plays a relatively minor role during the acute stage of oxygen deprivation in mammalian spinal cord white matter.
Similar content being viewed by others
Introduction
Oxygen deprivation, or ischemia, either due to primary injury such as stroke or as a secondary consequence of trauma, can produce or exacerbate many detrimental effects to the central nervous system (CNS).1, 2, 3, 4, 5 In the case of spinal cord injury, paralysis can result from a brief episode of ischemia, such as that which results from clamping of the aorta during life-saving surgeries.1, 6, 7, 8, 9 However, more commonly, ischemia, as a result of ruptured or compressed blood vessels, is a secondary injury compounding the primary trauma.10, 11, 12 It is well established that ischemia plays a critical role in the functional and structural damage of the CNS in general and spinal cord in particular.3, 4, 12
Although it is well documented that ischemia causes cellular damage, the mechanism of how ischemia can produce such an injury at the cell and tissue level is not fully understood. More specifically, it is not clear whether the lack of oxygen is sufficient to cause short-term functional and structural deficits. Considering the challenge of separating various factors related to ischemia in in vivo studies, the role of oxygen deprivation after ischemia is likely to be more appropriately investigated in an in vitro model. In this model, the lack of oxygen and other pathological pathways secondary to oxygen deprivation can be largely separated and investigated in isolation.13
Among the many functions of the nervous system, electrical impulse conduction is the most important. Disruption of functional pathway results in paralysis, regardless of the status of the anatomical structure.14, 15 Therefore, impulse conduction has been used as an index of the functional status of the nervous system in both physiological and pathological conditions. Despite the importance of electrical impulse conduction, the detailed characteristics of the compound action potential (CAP) of spinal cord axons in response to oxygen deprivation have not been investigated in detail. This is particularly true of the characteristics of the action potential in response to repetitive stimuli during ischemia.
In addition to the lack of detailed information regarding action potential changes in response to oxygen deprivation, the method to quantify the conduction of a single compound action potential is not uniform, which inevitably causes confusion when the results of different studies are compared. For example, Waxman and his co-workers have been using the sum of the area under the curve, or CAP area, to quantify the conduction of rat optic nerves.16, 17 On the other hand, Shi, Blight and their co-workers have been using the peak amplitude of the CAP as a means to estimate the impulse conduction in guinea pig spinal cord white matter.13, 18, 19, 20 Therefore, the question arises whether the end results are similar when using these two different methods. It was a concurrent purpose of this study to investigate this matter by quantifying the conduction of the impulses using the two above-mentioned methods in the same preparation to detect any discrepancies.
Methods
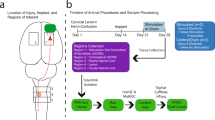
Isolation of spinal cord
Adult female Hartley guinea pigs of 350–500 g body weights were used. They were deeply anesthetized with a combination of ketamine (80 mg/kg) and xylazine (12 mg/kg). They were then perfused through the heart with oxygenated, cold, Krebs solution to remove the blood and lower core temperature. The entire vertebral column was excised rapidly and a complete laminectomy was performed. The spinal cord was removed from the vertebrae and immersed in cold Krebs solution, then immediately subdivided, first along the sagittal midline and then by cutting each half of the cord radially, to isolate the ventral white matter. Each white matter strip was subsequently incubated in fresh Krebs solution at room temperature, bubbled continuously with 95% oxygen–5% carbon dioxide (Figure 1a). The composition of Krebs solution was described in our previous publications.18, 21 The experimental procedures were approved by the Purdue University Animal Care and Use Committee (PACUC) and all efforts were made to minimize the number of animals used and their distress.
Diagram of the double sucrose recording chamber and changes of compound action potential (CAP) and compound membrane potential (or GAP potential) in response to hypoxic insult. (a) The isolated spinal cord tract is shown mounted in the apparatus. The two ends of the tract were placed in separate wells filled with isotonic (120 mM) KCl, divided from the central well by narrow channels filled with flowing isotonic (230 mM) sucrose solution. The central compartment contains physiological test media superfused continuously. Seals fashioned from coverslips are secured in place with high vacuum silicon grease at the locations shown to eliminate the exchange of the various media from one compartment to the next. Ag/AgCl electrodes for recording and stimulation are in series with socket connectors at the locations shown. Note that the central chamber is at a ground potential for recording. Action potentials were generated at the left sucrose gap, conducted through the central well, and recorded at the right gap with the use of a bridge amplifier. The tissue in the central well was maintained at 37°C throughout the recording procedure. (b) CAPs and compound membrane potential from a typical cord strip in normal Krebs, following 60 min oxygen deprivation, and 30 min recovery. For CAP profile, each symbol represents the amplitude of a CAP recorded every 30 s. Compound membrane potential were recorded every 3 s. The individual CAPs taken prior to oxygen deprivation, at the end of oxygen deprivation, and following 30 min reoxygenation are shown in the inset. The length of oxygen deprivation and reoxygenation were 60 and 30 min, respectively. Note the decrease of CAP amplitude, and the depolarization of compound membrane potential after the onset of oxygen deprivation, and the partial recovery following reoxygenation. (c) Reduction and complete recovery of oxygen tension in response to oxygen deprivation and restoration. The diagram shows an example of changes in amplitude of oxygen tension plotted against time. Note that the level of oxygen tension decreased rapidly over the course of 5 min from the oxygen deprivation. Also note the swift recovery (<5 min) of oxygen tension as a result of reperfusion
Electrophysiological recording of isolated spinal cord white matter
Recording chamber
The construction of the recording chamber is illustrated in Figure 1a. A strip of isolated spinal cord white matter, approximately 35 mm in length, was supported in the central compartment and continuously perfused with oxygenated Krebs solution (2 ml/min) by means of a peristaltic pump. Both ends of the spinal cord strip were placed across the sucrose gap channels to side compartments filled with isotonic (120 mM) potassium chloride. The sucrose gap channels were sealed using fragments of plastic coverslip and small amount of silicone grease that secured the coverslip of the channel. Isotonic sucrose solution was continuously run through the gap channels at a rate of 2 ml/min. The temperature of the solution was maintained at 37°C with an inline heater (Warner Instruments, Hamden, CT, USA). The axons were stimulated and compound action potentials (CAPs) were recorded at opposite ends of the strip of white matter by silver/silver-chloride wire electrodes positioned within the side chambers and the central bath. The central bath was connected to an instrument ground. Stimuli were delivered through a stimulus isolation unit and were usually in the form of 0.1 ms constant current unipolar pulses. Recordings were made using a bridge amplifier and Neurocorder (both from Neurodata Instruments, Delaware Water Gap, PA, USA). Subsequent analysis was performed using custom Labview® software (National Instruments, Austin, TX, USA) on a Compaq PC™. More details and description of the chamber can be found in our previous publications.18, 21
Compound action potential amplitude
For the recording of CAP amplitude, stimuli were delivered at a frequency of one stimulus for every 3 s. A supramaximal stimulus (110% of the maximal stimulus) intensity was chosen for this test. The digitized profile of each responding CAP was recorded continuously and stored in the computer for later analysis. In addition, a real time plot of CAP amplitude was also displayed during the experiment.
CAP conduction was assessed based on peak amplitude and CAP area, both were estimated using the LabView program. CAP area was measured by integrating the area under the CAP profile from the beginning to 4 ms from the onset of the CAP (Figure 2).
Measurements of CAP changes in response to oxygen deprivation and reoxygenation: peak amplitude versus CAP area. (a) A schematic diagram demonstrates two methods of measuring CAP changes, CAP amplitude and the area under the curve. Note the area under the curve was measured between the onset and 4 ms after the onset of CAP. A LabView computer program was used to integrate the shaded area denoted in the diagram. (b) Graph depicting CAP amplitude and the area under the CAP curve presented as a percentage of the preinjury value after oxygen deprivation and reoxygenation. Note that CAP could not be abolished by 60 min hypoxic insult and recovered significantly upon reoxygenation (P<0.05). Also note the lack of significance between the two different methods of quantification (P>0.05)
Depolarizing afterpotential (DAP) was measured at both 2 and 4 ms after the peak of the CAP. It has been shown that the DAP is generated within a few ms after an action potential is initiated.22, 23 The amplitude of the DAP is expressed either as percentage of the peak of the CAP amplitude or in absolute value (mV).
Activation threshold
The spinal cord CAP is a composite waveform obtained from the summation of action potentials from many different axons. Current–voltage tests, which consist of a series of stimuli with increasing intensity, can gradually stimulate axons of different thresholds to fire action potentials. Axons with different diameters have different thresholds to fire an action potential in response to a stimulation.24, 25 The larger diameter axons will be activated first due to the lower threshold. This test was used to detect changes in activation threshold (probability) before and after ischemic insult. The test protocol was programmed in the software and was performed by the computer automatically. The stimulus intensities ranged from 0.015 to 2.0 mA. Each cord strip was stimulated at the same current steps at pre-oxygen deprivation, the end of oxygen deprivation, and the end of reoxygenation. At each stimulus intensity level, five stimuli were repeated and an average value was used. Throughout the test, the stimulus at each intensity was always delivered at a frequency of one stimulus every 3 s. The current–voltage tests have been described repeatedly in our previous publications, we refer the interested reader to these reports.13, 18, 20, 21
Refractory period
The refractory period was examined by stimulating the cord with a series of dual pulses with various interstimuli intervals, ranging from 0.5 to 13 ms. A supramaximal stimulus (110% of the maximal stimulus) intensity was chosen for the refractory test. The amplitude of the first responding action potential remained the same for each pair of stimuli. The period immediately after the first stimulus when no action potential could be elicited was defined as the absolute refractory period. The time when the second responding CAP was the same height as the first one was defined as the relative refractory period. For the analysis, the amplitude of the second CAP was expressed as a percentage of the first one.
The ability to follow train stimuli in response to oxygen deprivation
A supramaximal stimulus intensity (110% of the maximal stimulus) was chosen for this test. The train of repetitive stimuli was delivered to the spinal cord in the chamber at both 500 and 1000 Hz for 50 and 100 ms. The last CAP was expressed as a percentage of the first peak.
Hypoxic insult and reoxygenation
Once a stable CAP and membrane potential were obtained, the normal Krebs solution was switched to a Krebs bubbled with 95% N2–5% CO2 gas mixture. This treatment reduces O2 tension by approximately 80%.13 Reoxygenation was accomplished by switching back to perfusion of the cord with normal Krebs media, well oxygenated as described in the Methods section.
Statistical treatment
Throughout the paper, Student's t-test was used to compare electrophysiological measurements between different groups. Statistical significance was attributed to values P<0.05. Averages were expressed as mean±standard error.
Results
The basic characteristics of CAPs recorded from isolated guinea pig spinal cords by using the double-sucrose gap recording chamber have been described previously.18, 21 Briefly, after a period of ∼30 min of stabilization in the recording chamber, the amplitude of the CAP plateaued. The spinal cord strips were then exposed to a period of oxygen deprivation (60 min) followed by 30 min of reoxygenation. The CAP was monitored continuously. A series of tests designed to examine the property of the CAP conduction were performed before oxygen deprivation, at the end of 60 min oxygen deprivation, and at the end of 30 min reoxygenation.
Changes in CAP conduction measured by peak amplitude and area
We first exposed the white matter strips to a 60 min period of oxygen deprivation which resulted in a significant reduction of peak amplitude and CAP area (Figures 1 and 2). Specifically, oxygen deprivation reduced the CAP amplitude to 30±5.3% of the pre-oxygen deprivation level, a significant reduction (P<0.005). The cord strip then regained 63±5.9% of CAP amplitude following 30 min of reoxygenation, a value that is significantly improved from that of oxygen deprivation (P<0.0001), yet still significantly lower than pre-oxygen deprivation levels (Figure 2; P<0.01). When the conduction was quantified using CAP area, the basic pattern remained the same. The CAP area reduced to 27±4.7% of the pre-oxygen deprivation level following 60 min of oxygen deprivation and recovered to 53.5±6.7% of the pre-oxygen deprivation level following reoxygenation. There is no significant difference between the percentage of decrements in CAP amplitude and area (Figure 2; P>0.05).
A profile of changes in CAP amplitude following a typical oxygen deprivation and reoxygenation is shown in Figure 1b. The individual CAP waveform in the inset represents the potential at pre-oxygen deprivation, the end of oxygen deprivation, and the end of reoxygenation respectively. No appreciable difference is seen in the overall shape of the single action potentials in the above-mentioned stages. In addition to the changes of amplitude in response to oxygen deprivation, the membrane potential changes are also displayed in Figure 1b. In this example, along with the reduction of CAP amplitude, there was also a parallel membrane depolarization and partial repolarization of the axonal membrane potential during the oxygen deprivation and reoxygenation period. In two out of 17 cords tested in the current study, we extended the reoxygenation period to 60 min and a full recovery of conduction was achieved (102 and 97%, respectively).
Changes in DAP
In addition to peak amplitude, we have also measured the DAP at both 2 and 4 ms after the peak of the action potential (Figure 3). In Figure 3a and b, CAPs of pre-oxygen deprivation, oxygen deprivation and reoxygenation normalized to the prehypoxic level and superimposed are shown. It is obvious that the DAP, measured at both time points, was noticeably decreased following oxygen deprivation and recovered subsequent to reoxygenation. Specifically, the DAP at the first point (2 ms after the peak of CAP) at pre-oxygen deprivation level was 8.5±1.2% of the peak amplitude. This value was reduced to 4.3±0.9% of the peak amplitude following oxygen deprivation and recovered to 9.8±0.9%. Although the normalized height of the DAP during oxygen deprivation was significantly lower than the levels of pre-oxygen deprivation and after reoxygenation (P<0.005), there is no difference between pre-oxygen deprivation and post reoxygenation (Figure 3c, P>0.05). Similar results were obtained when the DAP at the second time point (4 ms after the peak of the action potential) was quantified and compared. Specifically, the DAP at the pre-oxygen deprivation level of 5.8±0.7% was reduced to 1.6±0.5% and recovered to 6.5±0.9% following reoxygenation. Again, while the DAP at the end of oxygen deprivation was significantly lower than both pre-oxygen deprivation and post reoxygenation levels (P<0.01), no significant difference was detected between pre-oxygen deprivation and post reoxygenation level (P<0.05).
Changes in DAP following hypoxic insult and reoxygenation. (a) Typical CAP examples of pre-oxygen deprivation, following 60 min oxygen deprivation, and 30 min reoxygenation were superimposed to compare the relative amplitude of depolarizing afterpotential (DAP). The CAP was normalized to the pre-oxygen deprivation level. The rectangle circumscribes the region shown in (b) at a higher magnification. (b) The relative amplitude of the DAP was compared for pre-oxygen deprivation, oxygen deprivation, and reoxygenation. Note the reduced level of the DAP as a result of oxygen deprivation and the recovery following reoxygenation. Quantitative measurements of the DAP in (c) were made at both 2 and 4 ms following the peak of the CAP. (c) Mean DAP of pre-oxygen deprivation, oxygen deprivation, and reperfused cords at 2 and 4 ms following the CAP peak. It is clear that following 60 min of oxygen deprivation, the amplitude of the DAP at these two time points post CAP peak are significantly lower than pre-anoxia (P<0.01). The DAP fully recovered upon reoxygenation (P<0.01). There is no significant difference of the DAP between pre-oxygen deprivation and after reoxygenation (P>0.05)
In order to detect the role of other processes contributing to the amplitude of DAP but independent of CAP amplitude, we have also conducted the analysis of DAP without its normalization to CAP amplitude. In the case of DAP measured at 2 ms after the peak of CAP, the value is 0.37±0.058 mV at pre-oxygen deprivation, 0.17±0.038 mV following oxygen deprivation, and 0.45±0.066 mV after reoxygenation. The amplitude of DAP during oxygen deprivation was significantly lower than the levels of pre-oxygen deprivation and after reoxygenation (P<0.01). There is no difference between pre-oxygen deprivation and post reoxygenation (P>0.05). The amplitudes of DAP measured at 4 ms after the peak of CAP are 0.25±0.35, 0.066±0.022, and 0.26±0.032 mV at pre-oxygen deprivation, following oxygen deprivation, and after reoxygenation, respectively. Again, the amplitude of DAP (4 ms following CAP) during oxygen deprivation was significantly lower than the levels of pre-oxygen deprivation and after reoxygenation (P<0.005). There is no difference between pre-oxygen deprivation and post reoxygenation (P>0.05).
Changes in activation threshold
To detect any changes in activation threshold for the CAP, we performed a current–voltage test.20 The spinal cord CAPs were recorded during increasing stimulus intensities before oxygen deprivation, at the end of oxygen deprivation, and at the end of reoxygenation. The amplitude of responding CAP was plotted in the graph in two combinations and compared (Figure 4). In Figure 4a, the responding CAP of pre-oxygen deprivation (X-axis) was plotted against that at the end of oxygen deprivation for each stimulus level. The trend of the data indicates that the larger diameter axons were less likely to be activated following oxygen deprivation (N=7). For example, at a stimulus intensity of approximately 0.08 mA (Figure 4a), almost half of the maximal amplitude was achieved in prehypoxic conditions while only 10% of maximal amplitude was reached in hypoxic conditions. Interestingly, when the responding CAPs at the end of reoxygenation (X-axis) were plotted against that of pre-oxygen deprivation, little difference in the activation threshold existed in these two conditions (Figure 4b, N=7), indicating a complete recovery upon reoxygenation.
The changes of activation threshold in response to oxygen deprivation. Average amplitudes of CAP at prehypoxic period (N=8) were plotted against CAP amplitude at the end of hypoxic period (N=8) (a) and reoxygenation period (N=8) (b). Each data point was expressed as a percentage of the maximal response at pre-oxygen deprivation, the end of oxygen deprivation, and the end of reoxygenation, respectively. The trend of the data in (a) indicate that there is a delay in the activation profile after oxygen deprivation, or larger diameter axons (or lower threshold) were less likely to be activated after oxygen deprivation. This suggests that the large diameter axons were more affected by oxygen deprivation. In contrast, the linear relation is apparent in (b), indicating that there is little difference in the stimulus thresholds profile of the spinal cord strips between prehypoxic period and reoxygenation period
Changes in responsiveness to dual and multiple stimuli
Next, we evaluated the changes in the refractory period of the cords in response to oxygen deprivation insult. Figure 5a shows the relationship between the interstimulus interval and the amplitude of the two elicited CAPs. The amplitude of the second CAP was plotted against the log of the interstimulus interval revealing the expected sigmoidal relationship (Figure 5b). Oxygen deprivation increased the absolute refractory period from 0.75±0.03 to 1.3±0.03 ms (N=8, P<0.0001), and relative refractory period from 5.13±0.14 to 6.13±0.35 ms (N=8, P<0.0001). Absolute refractory period recovered completely upon reoxygenation (0.713±0.035 ms). Relative refractory period following reoxygenation was reduced to a value (3.63±0.183 ms) that is significantly shorter than at the end of the oxygen deprivation period (P<0.0001).
Refractory period changes determined by twin pulse stimuli. (a) Superimposed, 20 individual recordings of CAP from a spinal cord strip in response to twin stimuli with different interstimulus intervals. The first CAP shows consistent amplitude across all interstimulus intervals due to constant stimulus intensity. From left to right, the amplitude of the second CAP of each recording increases as the stimulus interval progresses through the relative refractory period. (b) The amplitude of the second CAP is plotted as a percentage of the first CAP against the log of the interstimulus interval for eight spinal cord strips pre-oxygen deprivation (◊), oxygen deprivation (○), reoxygenation (□). Note that the relative refractory period response is sigmoidal, and that the % of CAP is reduced as a result of oxygen deprivation and recovered following reoxygenation. (c) Bar graph showing the changes of absolute and relative refractory period as a result of oxygen deprivation and their reversal upon reoxygenation (*P<0.001, N=8)
Changes in the ability to follow repetitive stimuli were also tested in response to hypoxic insult and following reoxygenation (Figure 6). Figure 6a shows an example of responses to the train stimuli administrated to the white matter strip. Figure 6b displays the average amplitude of the last CAPs in response to a train stimuli of 500 Hz/50 ms, 500 Hz/100 ms, 1000 Hz/50 ms, and 1000 Hz/100 ms (N=7 for each average). Within these four groups, oxygen deprivation reduced the responsiveness of cords and reoxygenation induces a recovery with a value that is higher than the pre-oxygen deprivation level. Statistical analysis revealed that the significant difference was detected only in the comparison between the value during oxygen deprivation and the value at the end of reoxygenation for the four groups (P<0.05).
Response of spinal cord strips to train stimuli at frequencies of 500 and 1000 Hz. (a) This graph shows a series of compound action potentials (CAPs) from an uninjured cord strip in response to a train stimuli of 1000 Hz and 50 ms duration. (b) Bar graph showing the pre-oxygen deprivation, oxygen deprivation, and post-reoxygenation responses to 500 and 1000 Hz stimuli at 50 and 100 ms duration. The data were averaged from the last CAPs of the responses of cord strips to train stimuli. Statistical difference (Student's t-test) was observed between oxygen deprivation and post reoxygenation in all four groups indicated in this figure: 500 Hz/50 ms, 500 Hz/100 ms, 1000 Hz/50 ms, and 1000 Hz/100 ms (P<0.05, N=7). Note that there is no significant difference between the response at 50 and 100 ms at both 500 and 1000 Hz (P>0.05)
Discussion
Previous studies of in vitro spinal cord ischemic injury
In the current study, we have found that guinea pig white matter can retain 63% of pre-oxygen deprivation level of axonal CAP amplitude following 60 min of oxygen deprivation and 30 min of reoxygenation. Consistent with the changes of CAP conduction, the responding membrane potential was observed to correlate with CAP amplitude, with depolarization in response to oxygen deprivation and partial repolarization upon reoxygenation (Figure 1b).
The changes of conduction observed in this study are, in general, consistent with our previous work showing that axons regained ∼70% of predeprivation conduction following a similar time course (30 min reoxygenation).13 In two out of 17 cords tested in the current study, we extended the reoxygenation period to 60 min and a full recovery of conduction was achieved (102 and 97%, respectively). This is also similar to the complete recovery of conduction achieved following a total of 60 min of reoxygenation in our previous study where both oxygen and glucose were deprived.13
It is interesting that, compared to our previous study where both oxygen and glucose were omitted in the media,13 the current study achieved a similar, if not slightly less, recovery of axonal conduction following 30 min of reoxygenation. This suggests that glucose may not be as influential a factor in ischemic insults within 30 min post oxygen deprivation. This is consistent with the previous observation that glucose given after hypoxic ischemia does not affect brain injury in piglets.26 Furthermore, it has been suggested that glucose may worsen the outcome of functional recovery following ischemic injury,27, 28 possibly through the promotion of an intracellular lactic acidosis where associated hydrogen ions are injurious to neurons and glia.29
Membrane potential depolarization is likely due to ionic imbalances across the axonal membrane as a result of lower energy levels, which stem from oxygen deprivation. The resulting ionic imbalance and depolarization could directly contribute to the failure of conduction loss. Specifically, prolonged membrane depolarization could inactivate Na channels and make it unresponsive to incoming stimuli. In addition, prolonged membrane depolarization could also contribute to the reduction of DAPs. DAPs have been shown to be generated, in part, through a voltage-dependent inward positive current, such as sodium or calcium.30, 31, 32 Therefore, prolonged depolarization may inactivate those channels that are responsible for the inward positive current. In addition, several other mechanisms have also been proposed to influence DAPs which will be discussed in detail below.
Reduction of DAP due to oxygen deprivation
Afterpotential is an important electrophysiological phenomenon that has been documented in animals ranging from the excitable cells of lizards33 to guinea pigs,34 rats,22 cats,22 and sheep.35 Afterpotential has long been recognized to influence the frequency of repetitive firing of action potentials as well as the excitability of neurons in certain areas of the central nervous system, such as motor cortex36 and hippocampus.37 It has been shown that afterpotential is affected by the activity of calcium-dependent potassium conductivity,38 ouabain (Na+/K+ pump blocker),39 and calcium channel blockers.39 Interestingly, an overactivation of K+ channel, or Na+/K+ pump, as a result of repetitive firing, has been shown to elicit a hyperpolarizing afterpotential in rat optic nerves, which can be blocked by TEA, 4-aminopyridine (4-AP), or strophanthidin, a blocker of the electrogenic pump (Na+/K+-ATP ase).40, 41 Furthermore, Kaji and Sumner42 have shown that conduction block at the site of demyelination can be improved by ouabain, likely through the blockade of the Na+/K+ electrogenic pump. We have found in the current study that the DAP, either normalized to its CAP peak amplitude or in absolute value, is significantly depressed following oxygen deprivation, but recovered upon 30 min of reoxygenation. This is true when the DAP was measured at both 2 and 4 ms after the peak of action potential. This may indicate a change in the activity of K+ channel and/or the Na+/K+ pump which have already been implicated in the formation of afterpotential.40, 41 For the same reason, the change in the activity of K+ channel and/or the Na+/K+ pump may directly lower the excitability of axons and lead to conduction block. A further ramification of a decrease of the DAP is that it may affect the responsiveness of axons to dual or multiple stimuli, which will be discussed next.
It is also worth mentioning that CAP amplitude following reoxygenation is about 70% of that at pre-oxygen deprivation, while DAP amplitude after reoxygenation is higher than the level at pre-oxygen deprivation. This infers that some process may affect DAP but not CAP, or at least contribute differently to these two phenomena.
Changes of responsiveness to dual and multiple stimuli
Similar to the decrease of CAP amplitude following oxygen deprivation, the responsiveness of axons to multiple stimuli following oxygen deprivation is also decreased. This is signified in the increase of the absolute and relative refractory periods, as well as the decreased ability to follow repetitive stimuli. As discussed above, an overactivation of the K+ channel and/or the Na+/K+ pump may contribute to the decrease of excitability by lowering the DAP.
It is interesting to point out that upon reoxygenation, the overall excitability of axons that are capable of conducting an action potential is actually higher than during pre-oxygen deprivation. This phenomenon was also noted in our previous study where both oxygen and glucose were deprived.13 The mechanism of such an increase in responsiveness is unknown.
Vulnerability of larger axons to hypoxic insult
Consistent with our previous observation, we have shown that larger diameter axons are more vulnerable to oxygen deprivation in terms of impulse conduction.13 This phenomenon is probably due to the fact that larger diameter axons are more energy demanding than smaller diameter axons.13 However, it is also interesting to point out that such vulnerability was partially reversible following 30 min of reoxygenation even though a complete recovery of the CAP conduction was not achieved (Figures 1 and 4). This indicates that even though the larger axons are more vulnerable to oxygen deprivation, they are sensitive to the return of the oxygen and regain conduction upon reoxygenation.
Method of quantifying CAP conduction: peak amplitude versus CAP area
It is clear in this study that the measurement of CAP conduction using both peak amplitude and CAP area is similar. This is important since both methods are used in different preparations in various labs.16, 18, 20, 43 Knowing the equivalency of these two methods in some situations will facilitate the comparisons of various findings and avoid duplicated and redundant efforts. Despite the similarity of these two methods in the current study, we suggest that caution be taken in some extreme situations where these two methods may produce significantly different results. One such situation is a significant increase of the DAP independent of peak CAP amplitude. In this case, CAP area will increase significantly, which could be much greater than the degree change in peak amplitude. This has been the case in the study where the millimolor 4-AP was applied to both uninjured and injured guinea pig cords.44 In conclusion, although the two approaches may make relatively little difference in the current study, it does not mean that they can be used interchangeably elsewhere. Similarity between these methods can only be expected in the cases where the DAP is only a small fraction of the peak amplitude or the DAP changes proportionally compared to the peak amplitude.
References
Allen BT . Spinal cord ischemia complicating aortic surgery. In: Callow AD, Ernst CB (eds). Vascular Surgery: The Theory and Practice. Appleton & Lange: Stamford, Conn 1995, pp 1402–1425.
Satran R . Spinal cord infarction. Stroke 1988; 19: 529–532.
Stys PK . Anoxic and ischemic injury of myelinated axons in CNS white matter: from mechanistic concepts to therapeutics. J Cereb Blood Flow Metab 1998; 18: 2–25.
Stys PK, Lopachin RM . Mechanisms of calcium and sodium fluxes in anoxic myelinated central nervous system axons. Neuroscience 1998; 82: 21–32.
White BC et al. Brain ischemia and reperfusion: molecular mechanisms of neuronal injury. J Neurol Sci 2000; 179: 1–33.
Coselli JS et al. Paraplegia after thoracoabdominal aortic aneurysm repair: is dissection a risk factor? Ann Thorac Surg 1997; 63: 28–35.
Kanellopoulos GK et al. Spinal cord ischemic injury. Development of a new model in the rat. Stroke 1997; 28: 2532–2538.
Lang-Lazdunski L et al. Ischemic spinal cord injury induced by aortic cross-clamping: prevention by riluzole. Eur J Cardiothorac Surg 2000; 18: 174–181.
Safi HJ et al. Effect of extended cross-clamp time during thoracoabdominal aortic aneurysm repair. Ann Thorac Surg 1998; 66: 1204–1209.
Young W . Secondary injury mechanisms in acute spinal cord injury. J Emergency Med 1993; 11: 13–22.
Young W . Blood flow, metabolic and neurophysiological mechanisms in spinal cord injury. In: Becker DP, Povlishock JT (eds). Central Nervous System Trauma Status Report. NIH, NINCDS: Bethesda, MD 1985, pp 463–473.
Sandler AN, Tator CH . Review of the effect of spinal cord trauma on the vessels and blood flow in the spinal cord. J Neurosurg 1976; 45: 638–646.
Peasley MA, Shi R . Resistance of isolated mammalian spinal cord white matter to oxygen–glucose deprivation. Am J Physiol Cell Physiol 2002; 283: C980–C989.
Borgens RB . Restoring function to the injured human spinal cord. Adv Anat Embryol Cell Biol 2003; 171 III–IV, 1–155.
Tator CH . Update on the pathophysiology and pathology of acute spinal cord injury. Brain Pathol 1995; 5: 407–413.
Stys PK et al. Role of extracellular calcium in anoxic injury of mammalian central white matter. Proc Natl Acad Sci USA 1990; 87: 4212–4216.
Stys PK, Ransom BR, Waxman SG . Compound action potential of nerve recorded by suction electrode: a theoretical and experimental analysis. Brain Res 1991; 546: 18–32.
Shi R, Blight AR . Compression injury of mammalian spinal cord in vitro and the dynamics of action potential conduction failure. J Neurophysiol 1996; 76: 1572–1580.
Shi R et al. Control of membrane sealing in injured mammalian spinal cord axons. J Neurophysiol 2000; 84: 1763–1769.
Jensen JM, Shi R . Effects of 4-aminopyridine on stretched mammalian spinal cord: the role of potassium channels in axonal conduction. J Neurophysiol 2003; 90: 2334–2340.
Shi R, Borgens RB . Acute repair of crushed guinea pig spinal cord by polyethylene glycol. J Neurophysiol 1999; 81: 2406–2414.
Blight AR, Someya S . Depolarizing afterpotentials in myelinated axons of mammalian spinal cord. Neuroscience 1985; 15: 1–12.
Lemon N, Turner RW . Conditional spike backpropagation generates burst discharge in a sensory neuron. J Neurophysiol 2000; 84: 1519–1530.
BeMent SL, Ranck Jr JB . A quantitative study of electrical stimulation of central myelinated fibers. Exp Neurol 1969; 24: 147–170.
West DC, Wolstencroft JH . Strength-duration characteristics of myelinated and non-myelinated bulbospinal axons in the cat spinal cord. J Physiol (Lond) 1983; 337: 37–50.
LeBlanc MH et al. Glucose given after hypoxic ischemia does not affect brain injury in piglets. Stroke 1994; 25: 1443–1447.
Zareie M et al. Contribution of lactate buffer, glucose and glucose degradation products to peritoneal injury in vivo. Nephrol Dial Transplant 2003; 18: 2629–2637.
Sala F et al. Role of glycemia in acute spinal cord injury. Data from a rat experimental model and clinical experience. Ann NY Acad Sci 1999; 890: 133–154.
Wass CT, Lanier WL . Glucose modulation of ischemic brain injury: review and clinical recommendations. Mayo Clin Proc 1996; 71: 801–812.
Suarez-Kurtz G . The depolarizing afterpotential of crab muscle fibres. A sodium-dependent process mediated by intracellular calcium. J Physiol 1979; 286: 317–329.
Zhang L, Valiante TA, Carlen PL . Contribution of the low-threshold T-type calcium current in generating the post-spike depolarizing afterpotential in dentate granule neurons of immature rats. J Neurophysiol 1993; 70: 223–231.
Friedman A et al. Slow depolarizing afterpotentials in neocortical neurons are sodium and calcium dependent. Neurosci Lett 1992; 135: 13–17.
Barrett EF, Barrett JN . Intracellular recording from vertebrate myelinated axons: mechanism of the depolarizing afterpotential. J Physiol 1982; 323: 117–144.
Lasser-Ross N, Ross WN, Yarom Y . Activity-dependent [Ca2+]i changes in guinea pig vagal motoneurons: relationship to the slow afterhyperpolarization. J Neurophysiol 1997; 78: 825–834.
Terek RM, January CT . Excitability and oscillatory afterpotentials in isolated sheep cardiac Purkinje fibers. Am J Physiol 1987; 252: H645–H652.
Witte OW . Afterpotentials of penicillin-induced epileptiform neuronal discharges in the motor cortex of the rat in vivo. Epilepsy Res 1994; 18: 43–55.
Wong RK, Prince DA . Afterpotential generation in hippocampal pyramidal cells. J Neurophysiol 1981; 45: 86–97.
Lopantsev VE, Taranenko VD . Paroxysmal afterpotentials and role of calcium-dependent potassium conductivity in neuronal activity of strychninized neocortex. Neuroscience 1990; 38: 137–143.
Kojima M, Sperelakis N . Effects of calcium channel blockers on ouabain-induced oscillatory afterpotentials in organ-cultured young embryonic chick hearts. Eur J Pharmacol 1986; 122: 65–73.
Gordon TR, Kocsis JD, Waxman SG . Pharmacological sensitivities of two hyperpolarizations in rat optic nerve. Brain Res 1989; 502: 252–257.
Gordon TR, Kocsis JD, Waxman SG . Electrogenic pump (Na+/K(+)-ATPase) activity in rat optic nerve. Neuroscience 1990; 37: 829–837.
Kaji R, Sumner AJ . Ouabain reverses conduction disturbances in single demyelinated nerve fibers. Neurology 1989; 39: 1364–1368.
Agrawal SK, Fehlings MG . Mechanisms of secondary injury to spinal cord axons in vitro: role of Na+, Na(+)-K(+)-ATPase, the Na(+)-H+ exchanger, and the Na(+)-Ca2+ exchanger. J Neurosci 1996; 16: 545–552.
Shi R, Blight AR . Differential effects of low and high concentrations of 4-aminopyridine on axonal conduction in normal and injured spinal cord. Neuroscience 1997; 77: 553–562.
Acknowledgements
We thank Dr Richard Borgens for his support and encouragement, and Dr Melissa Peasley and Duane Estep for their invaluable assistance in the course of this study. We also thank Jennifer McBride and Phyllis Zickmund for their critical reading of the manuscript. This study was supported by a NIH grant (R Shi) and funding from both Purdue University and the State of Indiana.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Pryor, J., Shi, R. Electrophysiological changes in isolated spinal cord white matter in response to oxygen deprivation. Spinal Cord 44, 653–661 (2006). https://doi.org/10.1038/sj.sc.3101901
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101901
Keywords
This article is cited by
-
Efficient repairing effect of PEG based tri-block copolymer on mechanically damaged PC12 cells and isolated spinal cord
Journal of Materials Science: Materials in Medicine (2014)
-
The Neuroprotective Ability of Polyethylene Glycol is Affected by Temperature in Ex Vivo Spinal Cord Injury Model
The Journal of Membrane Biology (2013)