Abstract
While social zeitgebers are known to shape diurnal preference, little research has been devoted to determining the contribution of the familiar group chronotype as social zeitgeber on individual circadian rhythms and sleep-wake patterns in adult subjects. The current study aimed to examine the matching between perceived family chronotype and individual chronotype and their relationship with sleep-wake patterns on weekdays and weekends, diurnal subjective somnolence, and substance consumption. Nine hundred and forty-two Colombian adults completed the Composite Scale of Morningness, the Epworth Sleepiness Scale, and responded to a questionnaire about circadian preferences of their family nucleus. We found evidence of a mismatch between perceived family and individual chronotype, mainly for morning-type individuals (Cohen’s Kappa = −0.231; p < 0.001). This mismatch was associated with diurnal subjective somnolence (β = 0.073; p < 0.001) and specific sleep-wake patterns (p < 0.01). In addition, subjects with evening-type families showed higher caffeine and alcohol consumption (p < 0.001). To our knowledge, this is the first study to assess and report the mismatching between perceived family and individual chronotypes, and it adds to the existing body of knowledge regarding the influence of social zeitgebers on circadian rhythms. This is particularly relevant since mismatching between circadian physiology and environmental cues have been shown to lead to diverse pathologies.
Similar content being viewed by others
Introduction
Circadian rhythms play a key role in human physiology by precisely regulating sleep and wake periods, appetite, cognitive function, and mood states, among many other functions1. While the temporal patterns of circadian functions follow a stable phase synchrony with daily cues (known as zeitgebers) and between each other, interindividual differences in said phase relationships have been described in humans. Based on their preferred timing of active and rest periods, people can be classified generally into three diurnal preference types or “chronotypes”: morning-type, neither-type, or evening-type2,3.
A person’s chronotype depends on several factors: genetic4, environmental5, as well as constitutional (i.e. age and sex) variables6. Older age correlates with a tendency to morningness, while young adults and teenagers are more often inclined to eveningness7. Sex differences are mainly linked to endocrine factors8, with males showing an evening preference more often than women9.
Environmental cues, most importantly the light-dark cycle, as well as social demands like school and working schedules are relevant for the determination of diurnal preference and its possible consequences in terms of health and social adaptations10. Familial interactions present a very specific type of social cueing. However, little research has been conducted in order to determine a potential contribution of this factor to individual chronotype.
Familiar effects can be mediated by genetic and heritable traits. Genetic studies have reported associations between extreme morningness with the Familial Advanced Sleep Phase Syndrome (ASPS) and of extreme eveningness with the Delayed Sleep Phase Syndrome (DSPS), though the results have been discordant11. In addition, a rural Brazilian family-based cohort study using the Morningness-Eveningness Questionnaire (MEQ), reported evidence of heritability of the MEQ score of 38% controlling for age, gender, and geographical zone of residence12. Overall, studies suggest that heritability accounts for between 12.4 and 29.4% of the variance in chronotype13, while 50% is determined by genetic factors14.
However, there can also be an effect of family derived from social behavior and individual chronotypes interactions per se. Some studies have looked at women during and after pregnancy and analyzed the interactions between the newborn’s, mother’s and father’s sleep patterns and chronotypes and they found that mother-infant matching is rooted in biological pacemakers and it predicts children’s social rhythms, and that new parent’s social rhythms showed changes on 24‐hr sleep‐wake rhythm after birth15,16.
Other studies have focused on the relationship between diurnal preferences of parents and their children. Boergers et al. reported an association between children’s sleep problems and parental chronotype, while Leonhard et al. found that children act as a social factor affecting mothers’ chronotype17,18. However, to our knowledge, no studies have addressed the relationship between family circadian preferences and individual chronotypes in adult subjects.
Additionally, substances consumption has been found relevant for sleep-wake patterns in samples of adults and young adults. Specifically, caffeine and alcohol consumption has been related to shorter sleep duration, increased sleep onset latency, and increased daytime sleepiness19,20. Smoking also has been associated with an increased long sleep latency, sleep medication use, and daytime sleepiness21.
The aim of the present study was to assess the possible matching or mismatching between perceived family and individual chronotype and their relationship with sleep and wake patterns, and sleep problems in a large sample of Colombian adults, including substances consumption as independent factors.
Methods
Participants
This study was approved by the Institutional Ethics Committee of the Universidad de Ciencias Aplicadas y Ambientales (Bogotá, Colombia) which certified its compliance with the ethical principles for medical research involving human subjects. Nine hundred and forty-two Colombian subjects participated in the study (mean age: 21.8; ±SD 5.0; range: 18–49; 63.7% females) after signing an informed written consent form. No monetary or academic incentive was given to the subjects for participation in the study. All participants resided in Bogotá, Colombia (04 °38′N, 74°05′W), and were recruited from two private universities in the same city. The sample was composed of two main groups: students (n = 786; mean age: 20.8; ±SD 2.9) and institutional workers (n = 156; mean age: 27.9; ±SD 8.6). Subjects’ inclusion criteria involved the absence of a personal history of neurological disorders, and of any sleep disorder (or current sleep pharmacological treatment) or chronic somatic diseases. The sample of this study was composed in part by subjects also included in two previous studies22,23.
Measures
Chronotype
Individual chronotype was assessed through the Composite Scale of Morningness (CSM), which is a 13-items Likert-type scale widely used to assess behavioral temporal preference and to classify individuals in the dimension of morningness-eveningness24. The CSM has been shown to be highly valid and reliable across cultures25. We used the translated version to the Spanish language performed previously by Adan et al.26, which has shown be valid and consistent in Colombian samples23,27. Based on previous studies performed on local populations, the following criteria were used to determine chronotypes based on the CSM score: morning-type: 36 points or below; evening-type: 43 points or over; subjects scoring between 37 and 42 points were considered as neither-type22. The CSM can be dissected into three main factors3. The Morningness factor is composed by CSM items 1, 3, 6, 8, 10, and 11 (scores range from 6 to 25), with higher scores reflecting the effort of getting up early in the morning. The Morning alertness factor is composed by items 4, 5, and 12 (scores range from 3 to 12), with higher scores reflecting a high level of alertness during the first half hour after waking up. The Activity plan factor is composed by the items 2, 7, 9, and 13 (scores range from 4 to 18), with higher scores indicating a self-perception of a high level of morning activity and an early bedtime. This three-factor solution was corroborated in the current sample through an exploratory factorial analysis and was found a Cronbach’s alpha of 0.71 for the whole scale.
To assess the perceived “family chronotype” participants were asked the following question: How do you think the people that make up your family nucleus (e.g. parents, brothers, sisters, children, grandparents) are, regarding their sleep habits?” Participants were required to choose within three possible answers: “early risers” (morning-types), “night owls” (evening-types), or “indifferent” (neither-types). The participants were asked to consider their “family nucleus” as the people in his family with whom they currently lived.
Sleep-wake patterns
To assess the sleep-wake pattern of the participants, we asked them to inform the number of hours of nocturnal sleep (HNS) per day during weekdays and weekends, with the following question: “How many hours do you sleep per night on weekdays and weekends?”
Subjective diurnal somnolence
General subjective level of diurnal somnolence was measured with the Epworth Sleepiness Scale (ESS), an auto-administered questionnaire that evaluates dozing behavior in different daily life situations28. Its score ranges from 0 to 24 (from no to high somnolence). The validity of the ESS has been previously reported for a Colombian population29. The current study revealed a Cronbach’s alpha of 0.71 for the instrument.
Substances consumption
Participants were asked to report whether they regularly consumed 1) caffeinated drinks, 2) tobacco, and 3) alcoholic drinks. Only yes or no were recorded as answers.
Statistical analysis
After checking the normality of data through skewness and kurtosis, we examined the variance differences in HNS in weekdays and weekends and of diurnal subjective somnolence included as dependent variables, according to sex, occupation, individual chronotype and perceived family chronotype as independent/fixed factor variables.
In order to test statistical differences in the sociodemographic variables, HNS in weekdays and weekends, diurnal subjective somnolence, and scores in the CSM subscales were treated as dependent variables while perceived family chronotype was treated as the independent variable. Analysis of variance was performed for continuous outcome variables considering the partial Eta squared (η2p) as effect size. Tukey’s honestly significant difference (HSD) post hoc test was used and a p-value of 0.016 was set for the post-hoc tests. For the categorical variables (sex, caffeine, and alcohol consumption and smoking), chi-squared tests were used.
Cohen’s Kappa coefficient was utilized to examine inter-rater reliability and accuracy of agreement between the individual and perceived family chronotypes. To test mean differences for concordance between the perceived family and individual chronotypes and sleep variables, we carried out an independent samples t-test and calculated effect sizes through Cohen’s d. In addition, to examine the association between sleep variables separately for the morning and evening participants whose chronotype did not match that of their families, Pearson’s correlation analyses were conducted. Because the sample was predominantly composed of young adults and the most frequently expected case was that of evening-type subjects along morning-type families, the above analyses were reduced to these two chronotypes.
Finally, in order to explore the association between individual and familiar chronotypes a categorical regression analysis (CATREG) version 3.0 (DTSS, Leiden, The Netherlands) was used, controlling for relevant sociodemographic variables. CATREG analysis is appropriate for models in which there are categorical variables given that each categorical variable introduced in the model is transformed by means of replacing categories with optimal values using the optimal scaling methodology. CATREG estimates the regression coefficients and the quantifications simultaneously in an iterative process; furthermore, this analysis uses Lasso (Least Absolute Shrinkage and Selection Operator), a regularized regression method that has demonstrated be more accurately for the prediction of the dependent variable through a subset of more stable predictors. Regularized regression comprises shrinking of the regression coefficients to improve the prediction accuracy by means of the reduction of standard errors of the coefficients estimates in the presence of multicollinearity30. Two CATREG models were conducted, the first for morning and evening types and the second for the “non-matching” group of participants. In both models, the outcome variable of the analysis was the individual chronotype, included as a categorical variable in the model, while the predictor variables were perceived family chronotype, sex, age, caffeine and alcohol consumption, and smoking included as categorical variables, and subjective diurnal somnolence as a continuous variable. For the individual and perceived family chronotypes only the morning- and evening-types were analyzed, for the reasons discussed above.
All statistical analyses were performed using the Statistical Package for the Social Sciences V.22 (SPSS Inc., Chicago, IL). The statistical significance was set at p values < 0.05. Data are presented as mean ± standard deviation, when applicable.
Results
Average of reported hours of nocturnal sleep per day during weekdays was 5.5 h ± 1.5 and 8.6 h ± 2.2 on weekends. The average of diurnal subjective somnolence for the whole sample was 10.1 ± 4.2. Descriptive data for the reported HNS per day during weekdays, as well as for diurnal subjective somnolence is shown in Table 1. No statistical differences were found according to sex or individual chronotype for HNS per day. Significant differences were found in HNS during weekdays according to occupation, with workers reporting a higher average of hours of nocturnal sleep (F (1, 939) = 8.48; p = 0.003; η2p = 0.009). Perceived family chronotype was found to significantly affect reported hours of sleep during weekdays, with neither-types displaying the highest average of HNS (F (2, 938) = 5.93; p = 0.002; η2p = 0.013). Regarding diurnal subjective somnolence, women showed a higher average levels than males (F (1, 940) = 30.8; p = 0.0000; η2p = 0.032), as also did students compared with workers (F (1, 940) = 6.41; p = 0.011; η2p = 0.007), and evening-types among chronotypes (F (2, 939) = 10.41; p = 0.0001; η2p = 0.022). In addition, subjects reporting a morning-type family showed a higher average of diurnal subjective somnolence (F (2, 938) = 3.40; p = 0.033; η2p = 0.007) compared with subjects reporting other perceived family chronotypes.
The overall average CSM score for the whole sample was 39.63 ± 5.51. Subjects reported their chronotype as follows: 270 morning-types (28.7%; 165 females, 105 males), 269 evening-types (28.6%; 181 females, 88 males), and 403 neither-types (42.8%; 254 females, 149 males). Perceived family chronotypes as reported by participants revealed 194 to be morning-types (20.6%), 577 evening-types (61.3%), and 170 neither types (18.1%) (Table 2).
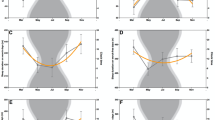
According to variance analysis, we found significant differences between reported perceived family chronotype in HNS in weekdays and weekends, diurnal subjective somnolence, and in all CSM subscales (Morningness, Activity planning, and Morning alertness; Table 2). Tukey’s HSD post hoc test showed that morning-types reported less HNS than evening-types and neither types (Mean difference: MD = 0.38; p < 0.01; MD = 0.49; p < 0.01; respectively). For the Morningness factor of the CSM, participants with morning-type families revealed lower scores when compared with evening-type families (MD = 1.12; p < 0.01) and with neither-type families (MD = 1.01; p < 0.01). Those with evening-type families and with neither type families showed higher scores for the Activity planning factor when compared with those with morning-type families (MD = 1.66; p < 0.01; MD = 1.22; p < 0.01; respectively). Regarding the Morning alertness factor a small albeit overall significant difference was found according to familiar chronotype (F = 3.35; p = 0.035; η2p = 0.007), however, a post-hoc test did not show significant differences between groups.
Table 1 shows the variance and frequency analyses for sociodemographic variables and CSM factors according to individual chronotype. Statistical differences were found for individual chronotype according to alcohol consumption, HNS in weekdays and weekends, diurnal subjective somnolence, and each of the three CSM factors. Specifically, the post-hoc analyses of HNS in weekdays and weekends did not show statistical differences. Diurnal subjective somnolence presented a difference between morning- and evening-types (MD = −1.67; p < 0.01). Regarding CSM factors, all contrasts were significant (p < 0.01). Neither- and evening-types reported a higher alcohol consumption than morning-types (p < 0.01).
The overall Cohen’s kappa, the measure of inter-rater reliability and agreement for individual and perceived family chronotype, was −0.231 (Table 3). Based on published guidelines31 this kappa value suggests only minimal agreement, although statistically significant (p < 0.001). Morning- and evening-type participants whose chronotype matched that of their families (as perceived by themselves) represented only 38.3% of the sample, while “non-matching” subjects represented the 61.6%. In the “non-matching” participants group individual chronotypes were 34.3% morning-types and 10.7% evening-types; while perceived family chronotypes were 23.4% morning-types and 62.8% evening-types.
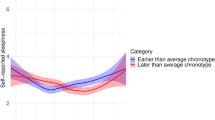
The “non-matching” participants displayed significantly lower levels of diurnal subjective somnolence compared with “matching” participants, although with a small effect size (Cohen’s d = 0.10). No differences were observed for the average HNS during weekdays nor during weekends (Table 4). Furthermore, “non-matching” subjects displayed higher mean values at all CSM subscales, and these differences showed medium effect sizes (Table 4).
The Pearson’s correlation analysis for the non-matching participants showed significant negative associations between diurnal subjective somnolence with the CSM morningness factor (p < 0.01) and with the morning alertness factor (p < 0.01). Also, we found significant positive associations between HNS during weekdays and all CSM factors (p < 0.05) (Supplementary material, Table S1).
A CATREG analysis revealed that the model including perceived family chronotype can explain 11% of the variance in individual chronotype (morning- and evening-types) (Table 5). Perceived family chronotype explains on its own 6.8% of the variance (β = 0.26; p < 0.01). Age, alcohol consumption, diurnal subjective sleepiness and hours of nocturnal sleep during weekends also correlated significantly with individual chronotype in the whole sample. In the CATREG analysis only including the “non-matching” subjects, the perceived family chronotype can explain 72.5% of the variance in individual chronotype (morning- and evening-types). Perceived family chronotype explains on its own 71% of the variance (β = 0.84; p < 0.01). Age and diurnal subjective somnolence were significant variables in the model (Table 5).
Discussion
To our knowledge, this is the first study to present evidence of a correlation between individual chronotype and reported familiar chronotype. The results of our work indicate that familiar interactions should be added to the list of the multiple factors that determine diurnal preference phenotype. We observed several differences in sleep patterns according to perceived family chronotype: individuals that considered their families as morning-type reported fewer hours of nocturnal sleep during weekdays and a higher level of subjective sleepiness during the day. In addition, perceived family chronotype was found to be an important explicative factor on individual chronotype variance.
All three CSM subscales showed significant association with reported familiar chronotype. We found that individuals whose chronotypes did not match with their perceived family chronotype (excluding neither-types) showed higher values in the CSM subscales, suggesting that these individuals could have a tendency to be “early risers”. This finding is concordant with the fact that in the “non-matching” participants group the predominant individual chronotype was the morning type (34.3%), while the predominant perceived family chronotype was the evening type (62.8%). At this point, it is interesting to highlight previous results from a Colombian study, showing significant associations between PER2 gene polymorphisms with higher values of CSM-morning alertness factor and between PER3 gene polymorphisms with higher values of CSM-morningness factor22. Future studies could address this genetic variables in relation to the self-reports used in this study, considering that these genes have a central role in the molecular mechanism of the circadian rhythms.
Our findings are in line with those reported by Salgado et al. regarding sleep disturbances associated with disruption of circadian rhythms by lifestyle conditions32. In the first place, we found that diurnal sleepiness scores were higher for participants who considered their families to be “morning-types”, and this was the group that presented the lesser level of agreement between individual and familiar chronotype (only 7%). Individuals who matched their own with their families’ chronotype reported higher average levels of somnolence, although this seemingly paradoxical result may arise as an indirect effect of these being mainly evening-type individuals, which showed greater subjective somnolence values. On the other hand, when we conducted a correlation analysis only for the group of the “non-matching” subjects (including only evening- and morning-types individuals), significant negative associations were found between diurnal subjective somnolence and the CSM Morningness and Morning Alertness factors. This finding shows the impact of having an evening preference on diurnal alertness when the perceived family chronotype does not match with the individual chronotype. In addition, the association found between HNS in weekdays and all CSM factors strengthens this interpretation, showing an apparent attempt of the non-matching individuals to compensate the sleep debt and diurnal somnolence of the week with more hours of sleep on weekends.
Furthermore, previous studies also found a significant relationship between diurnal subjective somnolence evening preference chronotype33,34. If we assume both the subject and her family to prefer to go to bed late while demands of study and work requirements that they wake up early we can hypothesize that sleep timing will not be satisfying or even appropriate, leading to increased sleepiness during the day. In this sense, we found that a high proportion of evening-type subjects and of subjects reporting evening-type families sleep fewer hours than other chronotypes during weekdays, and sleep more hours on weekends, which may suggest that evening-types try to compensate on the weekends the few hours of sleep achieved during the weekdays. In addition, this need for sleep compensation could be more important when both the subject and her family are evening-types.
We found that participants with perceived evening-type families reported more often to consume caffeinated and alcoholic beverages. This result fits in with reports indicating a higher prevalence of substance use by evening-type subjects, being considered this chronotype as a risk factor in the onset and maintenance of drug consumption35,36,37. Moreover, a relevant hypothesis to consider is that having an evening chronotype added to family mismatch could represent an increased risk factor. However, it is important to mention that a relevant limitation of the current study was the assessment of substance consumption which was in a dichotomous form (yes or no), therefore the consumption could not be quantified.
Mismatch of natural circadian rhythmicity and individual chronotype with natural and/or social zeitgebers has been proven deleterious to human health at several levels including mental health38,39. Our work has addressed the subject of “familiar” diurnal preference understood as an additional social zeitgeber affecting human daily rhythms, beyond those widely studied as work and school schedules and social-cultural interactions. As such, it could be considered as an element in therapies aiming to stabilize social rhythms, according to the “social zeitgeber” theory40.
Some limitations of the present study should be addressed. More importantly, this work consisted of a cross-sectional design relaying in undetailed self-reports of the several variables studied and family-chronotype was assessed through the subjects’ own perception. Moreover, the effect sizes of our results were relatively small. In this sense, the inclusion of a standardized assessment of social rhythm disruption or the individual chronotype of family members would have increased the weight of our findings. Moreover, while the absence of a diagnosis of the mental disease was included as an inclusion criterion, we did not record any depressive and anxiety symptomatology measures. However, the size of our sample is large enough to support the general outline of our findings. Also, importantly, our data add to previous literature in the field, focused mainly in European and North American samples, by including a previously non-studied population from South America.
Our findings suggest that mismatching between perceived family and individual chronotypes represents a relevant factor affecting biological rhythmicity that should be addressed in future studies. More detailed studies dissecting each of the variables in this work through precise measurements should be conducted in order to determine the exact contributions of familiar chronotype on individual circadian health and disease.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Tsaousis, I. Circadian preferences and personality traits: A meta‐analysis. European Journal of Personality 24, 356–373 (2010).
Adan, A. et al. Circadian typology: a comprehensive review. Chronobiology international 29, 1153–1175, https://doi.org/10.3109/07420528.2012.719971 (2012).
Randler, C. & Díaz‐Morales, J. F. Morningness in German and Spanish students: A comparative study. European Journal of Personality 21, 419–427 (2007).
Roenneberg. & Merrow, M. The network of time: understanding the molecular circadian system. Current biology: CB 13, R198–207 (2003).
Roenneberg et al. Epidemiology of the human circadian clock. Sleep medicine reviews 11, 429–438 (2007).
Fischer, D., Lombardi, D. A., Marucci-Wellman, H. & Roenneberg, T. Chronotypes in the US - Influence of age and sex. PloS one 12, e0178782, https://doi.org/10.1371/journal.pone.0178782 (2017).
Randler, C. Ontogeny of morningness-eveningness across the adult human lifespan. Die Naturwissenschaften 103, 3, https://doi.org/10.1007/s00114-015-1326-z (2016).
Park, Y. M., Matsumoto, K., Seo, Y. J., Kang, M. J. & Nagashima, H. Changes of sleep or waking habits by age and sex in Japanese. Perceptual and motor skills 94, 1199–1213, https://doi.org/10.2466/pms.2002.94.3c.1199 (2002).
Adan, A. & Natale, V. Gender differences in morningness-eveningness preference. Chronobiology international 19, 709–720 (2002).
Roenneberg., W.-J., Merrow, A. & Life, M. between clocks: daily temporal patterns of human chronotypes. Journal of biological rhythms 18, 80–90, https://doi.org/10.1177/0748730402239679 (2003).
Allebrandt, K. V. & Roenneberg, T. The search for circadian clock components in humans: new perspectives for association studies. Brazilian journal of medical and biological research = Revista brasileira de pesquisas medicas e biologicas 41, 716–721 (2008).
von Schantz, M. et al. Distribution and heritability of diurnal preference (chronotype) in a rural Brazilian family-based cohort, the Baependi study. Scientific reports 5, 9214, https://doi.org/10.1038/srep09214 (2015).
Klei, L. et al. Heritability of morningness-eveningness and self-report sleep measures in a family-based sample of 521 hutterites. Chronobiology international 22, 1041–1054, https://doi.org/10.1080/07420520500397959 (2005).
Hur, Y. M. Stability of genetic influence on morningness-eveningness: a cross-sectional examination of South Korean twins from preadolescence to young adulthood. Journal of sleep research 16, 17–23, https://doi.org/10.1111/j.1365-2869.2007.00562.x (2007).
Yamazaki, A., Lee, K. A., Kennedy, H. P. & Weiss, S. J. Parent chronotypes and sleeping and crying/fussing in 4–5 week infants. Sleep and Biological Rhythms 3, 158–161 (2005).
Feldman, R. From biological rhythms to social rhythms: Physiological precursors of mother-infant synchrony. Developmental psychology 42, 175–188, https://doi.org/10.1037/0012-1649.42.1.175 (2006).
Boergers, J., Hart, C., Owens, J. A., Streisand, R. & Spirito, A. Child sleep disorders: associations with parental sleep duration and daytime sleepiness. Journal of family psychology: JFP: journal of the Division of Family Psychology of the American Psychological Association 21, 88–94, https://doi.org/10.1037/0893-3200.21.1.88 (2007).
Leonhard, C. & Randler, C. In sync with the family: children and partners influence the sleep-wake circadian rhythm and social habits of women. Chronobiology international 26, 510–525, https://doi.org/10.1080/07420520902821101 (2009).
Owens, J. Adolescent Sleep Working, G. & Committee on, A. Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics 134, e921–932, https://doi.org/10.1542/peds.2014-1696 (2014).
Thakkar, M. M., Sharma, R. & Sahota, P. Alcohol disrupts sleep homeostasis. Alcohol 49, 299–310, https://doi.org/10.1016/j.alcohol.2014.07.019 (2015).
Lohsoonthorn, V. et al. Sleep quality and sleep patterns in relation to consumption of energy drinks, caffeinated beverages, and other stimulants among Thai college students. Sleep & breathing = Schlaf & Atmung 17, 1017–1028, https://doi.org/10.1007/s11325-012-0792-1 (2013).
Ojeda, D. A. et al. A novel association of two non-synonymous polymorphisms in PER2 and PER3 genes with specific diurnal preference subscales. Neuroscience letters 553, 52–56, https://doi.org/10.1016/j.neulet.2013.08.016 (2013).
Pereira-Morales, A. J., Adan, A., Bussi, I. L. & Camargo, A. Anxiety symptomatology, sex and chronotype: The mediational effect of diurnal sleepiness. Chronobiology international, 1–11, https://doi.org/10.1080/07420528.2018.1479713 (2018).
Smith, C. S., Reilly, C. & Midkiff, K. Evaluation of three circadian rhythm questionnaires with suggestions for an improved measure of morningness. The Journal of applied psychology 74, 728–738 (1989).
Caci, H. et al. Transcultural properties of the composite scale of morningness: the relevance of the “morning affect” factor. Chronobiology international 22, 523–540, https://doi.org/10.1081/CBI-200062401 (2005).
Adan, A., Caci, H. & Prat, G. Reliability of the Spanish version of the Composite Scale of Morningness. European psychiatry: the journal of the Association of European Psychiatrists 20, 503–509, https://doi.org/10.1016/j.eurpsy.2005.01.003 (2005).
Smith, C. S. et al. Investigation of morning–evening orientation in six countries using the preferences scale. Personality and Individual Differences 32, 949–968 (2002).
Johns, M. W. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15, 376–381 (1992).
Chica-Urzola, H. L., Escobar-Cordoba, F. & Eslava-Schmalbach, J. Validating the Epworth sleepiness scale. Revista de salud publica 9, 558–567 (2007).
Hartmann, A., Van Der Kooij, A. J. & Zeeck, A. Exploring nonlinear relations: models of clinical decision making by regression with optimal scaling. Psychotherapy research: journal of the Society for Psychotherapy Research 19, 482–492, https://doi.org/10.1080/10503300902905939 (2009).
McHugh, M. L. Interrater reliability: the kappa statistic. Biochemia medica 22, 276–282 (2012).
Salgado-Delgado, R., Tapia Osorio, A., Saderi, N. & Escobar, C. Disruption of circadian rhythms: a crucial factor in the etiology of depression. Depression research and treatment 2011, 839743, https://doi.org/10.1155/2011/839743 (2011).
Kitamura, S. et al. Evening preference is related to the incidence of depressive states independent of sleep-wake conditions. Chronobiology international 27, 1797–1812, https://doi.org/10.3109/07420528.2010.516705 (2010).
Hidalgo, M. P., de Souza, C. M., Zanette, C. B. & Nunes, P. V. Association of daytime sleepiness and the morningness/eveningness dimension in young adult subjects in Brazil. Psychological reports 93, 427–434, https://doi.org/10.2466/pr0.2003.93.2.427 (2003).
Prat, G. & Adan, A. Influence of circadian typology on drug consumption, hazardous alcohol use, and hangover symptoms. Chronobiology international 28, 248–257, https://doi.org/10.3109/07420528.2011.553018 (2011).
Whittier, A. et al. Eveningness Chronotype, Daytime Sleepiness, Caffeine Consumption, and Use of Other Stimulants Among Peruvian University Students. Journal of caffeine research 4, 21–27, https://doi.org/10.1089/jcr.2013.0029 (2014).
Adan, A. A chronobiological approach to addiction. Journal of Substance Use 18, 171–183 (2013).
Grandin, L. D., Alloy, L. B. & Abramson, L. Y. The social zeitgeber theory, circadian rhythms, and mood disorders: review and evaluation. Clinical psychology review 26, 679–694, https://doi.org/10.1016/j.cpr.2006.07.001 (2006).
Reed, V. A. Shift work, light at night, and the risk of breast cancer. AAOHN journal: official journal of the American Association of Occupational Health Nurses 59, 37–45, quiz 46, https://doi.org/10.3928/08910162-20101216-01 (2011).
Frank, E. et al. Two-year outcomes for interpersonal and social rhythm therapy in individuals with bipolar I disorder. Archives of general psychiatry 62, 996–1004, https://doi.org/10.1001/archpsyc.62.9.996 (2005).
Acknowledgements
The authors wish to thank Carmen L Niño, Isabel Avila, Lorena Camacho, Sebastián Higuera and Mery López for their assistance in data collection. This study was supported by Universidad de Ciencias Aplicadas y Ambientales U.D.C.A, Bogotá, Colombia; and in part by grants from COLCIENCIAS (Contract #765–2011). The Spanish Ministry of Economy, Industry, and Competitiveness (Grant PSI2015-65026; MINECO/FEDER/UE) supports A.A.
Author information
Authors and Affiliations
Contributions
A.P.-M. conceived the study, analyzed the data, and wrote the manuscript. A.A. provided support in the data analysis, discussion, and writing of the manuscript. L.C. provided support in the data analysis, discussion, and writing of the manuscript. A.C. conceived the study and provided support in the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pereira-Morales, A.J., Adan, A., Casiraghi, L.P. et al. Mismatch between perceived family and individual chronotype and their association with sleep-wake patterns. Sci Rep 9, 6756 (2019). https://doi.org/10.1038/s41598-019-43168-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-43168-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.