Abstract
Background
To test clinically significant prostate cancer (csPCa) rates during follow-up in biopsy naïve patients that underwent two different diagnostic pathways: (1) SB GROUP (n = 354): systematic random biopsies (SB) vs. (2) TB GROUP (n = 264): multiparametric magnetic resonance imaging (mpMRI) and only targeted biopsies (TB) of PI-RADS ≥ 3 lesions. Patients with PI-RADS ≤ 2 score avoided prostate biopsies.
Methods
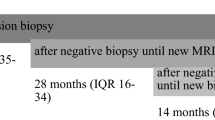
Retrospective single centre study of 618 biopsy naive patients (2015–2018). Two different definitions of csPCa were used: (1) csPCa ISUP GG ≥ 2 (ISUP grade group [GG] ≥ 2) and (2) csPCa ISUP GG ≥ 3. Kaplan–Meier plots and univariable Cox regression models tested rates over time of csPCa ISUP GG ≥ 2 and caPCa ISUP GG ≥ 3 in SB GROUP vs. TB GROUP.
Results
At initial biopsy, TB achieved higher rates of csPCa ISUP GG ≥ 2 (35.3 vs. 18.9%; p < 0.001) and csPCa ISUP GG ≥ 3 (12.6 vs. 6.2%; p = 0.04), relative to SB. After a median time follow-up of 36 months, the rates of csPCa ISUP GG ≥ 2 (6.1 vs. 4.4%; p = 0.6) and csPCa ISUP GG ≥ 3 (3.3 vs. 1.1%; p = 0.2) were similar in SB GROUP vs. TB GROUP. Moreover, in TB GROUP patients that avoided prostate biopsies because of negative baseline mpMRI (n = 145), only 4.1% exhibited csPCa ISUP GG ≥ 2 during follow-up. Moreover, none of these patients (PI-RADS ≤ 2) had csPCa ISUP GG ≥ 3.
Conclusions
In biopsy naïve setting, a diagnostic pathway including pre-biopsy mpMRI and TB of only PCa suspicious lesions is not associated with higher rates of csPCa during follow-up, relative to a diagnostic pathway of SB. Moreover, patients with negative baseline mpMRI could safely avoid prostate biopsies and could be followed with repeated PSA testing, since only a small proportion of them would harbor csPCa.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Scattoni V, Zlotta A, Montironi R, Schulman C, Rigatti P, Montorsi F. Extended and saturation prostatic biopsy in the diagnosis and characterisation of prostate cancer: a critical analysis of the literature{A figure is presented}. Eur Urol. 2007;52:1309–22.
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH, et al. MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med. 2018;378:1767–77.
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet. 2017;389:815–22.
Elkhoury FF, Felker ER, Kwan L, Sisk AE, Delfin M, Natarajan S, et al. Comparison of targeted vs systematic prostate biopsy in men who are biopsy naive: the prospective assessment of image registration in the diagnosis of prostate cancer (PAIREDCAP) study. JAMA Surg. 2019;154:811–8.
Rouvière O, Puech P, Renard-Penna R, Claudon M, Roy C, Mège-Lechevallier F, et al. Use of prostate systematic and targeted biopsy on the basis of multiparametric MRI in biopsy-naive patients (MRI-FIRST): a prospective, multicentre, paired diagnostic study. Lancet Oncol. 2019;20:100–9.
van der Leest M, Cornel E, Israël B, Hendriks R, Padhani AR, Hoogenboom M, et al. Head-to-head comparison of transrectal ultrasound-guided prostate biopsy versus multiparametric prostate resonance imaging with subsequent magnetic resonance-guided biopsy in biopsy-naïve men with elevated prostate-specific antigen: a large prospective Mu. Eur Urol. 2019;75:570–8.
Porpiglia F, Manfredi M, Mele F, Cossu M, Bollito E, Veltri A, et al. Diagnostic pathway with multiparametric magnetic resonance imaging versus standard pathway: results from a randomized prospective study in biopsy-naïve patients with suspected prostate cancer. Eur Urol. 2017;72:282–8.
Pokorny MR, De Rooij M, Duncan E, Schröder FH, Parkinson R, Barentsz JO, et al. Prospective study of diagnostic accuracy comparing prostate cancer detection by transrectal ultrasound-guided biopsy versus magnetic resonance (MR) imaging with subsequent mr-guided biopsy in men without previous prostate biopsies. Eur Urol. 2014;66:22–9.
Tonttila PP, Lantto J, Pääkkö E, Piippo U, Kauppila S, Lammentausta E, et al. Prebiopsy multiparametric magnetic resonance imaging for prostate cancer diagnosis in biopsy-naive men with suspected prostate cancer based on elevated prostate-specific antigen values: results from a randomized prospective blinded controlled trial. Eur Urol. 2016;69:419–25.
Goldberg H, Ahmad AE, Chandrasekar T, Klotz L, Emberton M, Haider MA, et al. Comparison of magnetic resonance imaging and transrectal ultrasound informed prostate biopsy for prostate cancer diagnosis in biopsy naıve men: a systematic review and meta-analysis. J Urol. 2020;203:1–9.
Elwenspoek MMC, Sheppard AL, McInnes MDF, Merriel SWD, Rowe EWJ, Bryant RJ, et al. Comparison of multiparametric magnetic resonance imaging and targeted biopsy with systematic biopsy alone for the diagnosis of prostate cancer: a systematic review and meta-analysis. JAMA Netw Open. 2019;2:e198427.
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, et al. A contemporary prostate cancer grading system: a validated alternative to the gleason score. Eur Urol. 2016;69:428–35.
Barentsz JO, Richenberg J, Clements R, Choyke P, Verma S, Villeirs G, et al. ESUR prostate MR guidelines 2012. Eur Radio. 2012;22:746–57.
Weinreb JC, Barentsz JO, Choyke PL, Cornud F, Haider MA, Macura KJ, et al. PI-RADS Prostate Imaging - Reporting and Data System: 2015, Version 2. Eur Urol. 2016;69:16–40.
Schoots IG, Roobol MJ, Nieboer D, Bangma CH, Steyerberg EW, Hunink MGM. Magnetic resonance imaging-targeted biopsy may enhance the diagnostic accuracy of significant prostate cancer detection compared to standard transrectal ultrasound-guided biopsy: a systematic review and meta-analysis. Eur Urol. 2015;68:438–50.
Wegelin O, van Melick HHE, Hooft L, Bosch JLHR, Reitsma HB, Barentsz JO, et al. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal Ultrasound fusion versus Cognitive Registration. Is There a Preferred Technique? Eur Urol. 2017;71:517–31.
Kasivisvanathan V, Stabile A, Neves JB, Giganti F, Valerio M, Shanmugabavan Y, et al. Magnetic resonance imaging-targeted biopsy versus systematic biopsy in the detection of prostate cancer: a systematic review and meta-analysis. Eur Urol. 2019;76:284–303.
Valerio M, Donaldson I, Emberton M, Ehdaie B, Hadaschik BA, Marks LS, et al. Detection of clinically significant prostate cancer using magnetic resonance imaging-ultrasound fusion targeted biopsy: a systematic review. Eur Urol. 2015;68:8–19.
Panebianco V, Barchetti G, Simone G, Del Monte M, Ciardi A, Grompone MD, et al. Negative multiparametric magnetic resonance imaging for prostate cancer: what’s next? [Figure presented]. Eur Urol. 2018;74:48–54.
Venderink W, van Luijtelaar A, van der Leest M, Barentsz JO, Jenniskens SFM, Sedelaar MJP, et al. Multiparametric magnetic resonance imaging and follow-up to avoid prostate biopsy in 4259 men. BJU Int. 2019;124:775–84.
Padhani AR, Weinreb J, Rosenkrantz AB, Villeirs G, Turkbey B, Barentsz J. Prostate imaging-reporting and data system steering committee: PI-RADS v2 status update and future directions. Eur Urol. 2019;75:385–96.
Mottet N, Bellmunt J, Bolla M, Briers E, Cumberbatch MG, De Santis M, et al. EAU-ESTRO-SIOG Guidelines on Prostate Cancer. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol. 2017;71:618–29.
Costa DN, Kay FU, Pedrosa I, Kolski L, Lotan Y, Roehrborn CG, et al. An initial negative round of targeted biopsies in men with highly suspicious multiparametric magnetic resonance findings does not exclude clinically significant prostate cancer—Preliminary experience. Urol Oncol Semin Orig Investig. 2017;35:149–e15.
Pagniez M, Kasivisvanathan V, Puech P, Drumez E, Villers A, Olivier J. Predictive factors of missed clinically significant prostate cancers in men with negative MRI: a systematic review and meta-analysis. J Urol. 2020;204:24–32.
Luzzago S, Petralia G, Musi G, Catellani M, Alessi S, Di Trapani E, et al. Multiparametric magnetic resonance imaging second opinion may reduce the number of unnecessary prostate biopsies: time to improve radiologists’ training program? Clin Genitourin Cancer. 2018;17:88–96.
Moldovan PC, Van den Broeck T, Sylvester R, Marconi L, Bellmunt J, van den Bergh RCN, et al. What Is the Negative Predictive Value of Multiparametric Magnetic Resonance Imaging in Excluding Prostate Cancer at Biopsy? A Systematic Review and Meta-analysis from the European Association of Urology Prostate Cancer Guidelines Panel. Eur Urol. 2017;72:250–66.
Acknowledgements
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5 × 1000 funds. SL had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Luzzago, S., de Cobelli, O., Mistretta, F.A. et al. MRI-targeted or systematic random biopsies for prostate cancer diagnosis in biopsy naïve patients: follow-up of a PRECISION trial-like retrospective cohort. Prostate Cancer Prostatic Dis 24, 406–413 (2021). https://doi.org/10.1038/s41391-020-00290-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41391-020-00290-4
This article is cited by
-
Can we predict pathology without surgery? Weighing the added value of multiparametric MRI and whole prostate radiomics in integrative machine learning models
European Radiology (2024)
-
Association between previous negative biopsies and lower rates of progression during active surveillance for prostate cancer
World Journal of Urology (2022)