Abstract
Background
The impact of body mass index (BMI) on pharyngeal fat pads has been well studied, yet no study has assessed its associations on laryngeal morphology.
Objectives
To study the associations of BMI differences on laryngeal morphology in adult males using computed tomography angiography (CTA) scans.
Methods
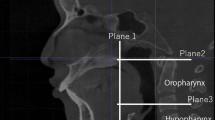
All adult male patients who underwent head and neck CTAs between 2011 and 2018 were initially included and categorized according to their BMI: (1) BMI < 20; (2) 20 ≤ BMI < 25; (3) 25 ≤ BMI < 30; (4) 30 ≤ BMI < 35; and (5) BMI ≥ 35. Anatomical measurements included pre-epiglottic and paraglottic fat-pad dimensions, airway width at the epiglottis tip and base, and epiglottis angle. For statistical analysis, BMI was regarded both as a categorical and continuous variable.
Results
One hundred and five scans were included. BMI ranged from 15.90 to 44.40 kg/m2. Significant differences were found in pre-epiglottic and paraglottic fat measurements between BMI subgroups 1–5 (Pre-epiglottic fat depth: 17.75, 17.74, 19.04, 20.73, and 21.09 mm, respectively, P = 0.005, correlation 0.343, and P < 0.001 in continuous measurement; Paraglottic space average width: 3.5, 5.4, 5.46, 6.85, and 7.38 mm, P < 0.001, correlation 0.532, and P < 0.001 in continuous measurement). As BMI increased, the epiglottis-hard-palate angle increased (56.4°, 55.3°, 65.2°, 64°, and 68.4°, P = 0.001, correlation 0.354, and P < 0.001 in continuous measurement). No significant difference was found in airway width between subgroups at the epiglottis tip or base. Yet, in continuous variables analysis, a significant negative correlation was found between BMI scores and the airway width at the epiglottis base (−0.226, P = 0.02).
Conclusions
In adult males, BMI is correlated with laryngeal fat-pad volume, affecting its morphology and airway width. Clinical implications regarding obstructive sleep apnea and voice quality should be further investigated.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Ciscar MA, Juan G, Martínez V, Ramón M, Lloret T, Mínguez J, et al. Magnetic resonance imaging of the pharynx in OSA patients and healthy subjects. Eur Respir J. 2001;17:79–86. https://doi.org/10.1183/09031936.01.17100790.
Whittle AT, Marshall I, Mortimore IL, Wraith PK, Sellar RJ, Douglas NJ. Neck soft tissue and fat distribution: comparison between normal men and women by magnetic resonance imaging. Thorax. 1999;54:323–8. https://doi.org/10.1136/thx.54.4.323.
Welch KC, Foster GD, Ritter CT, Wadden TA, Arens R, Maislin G, et al. A novel volumetric magnetic resonance imaging paradigm to study upper airway anatomy. Sleep. 2002;25:530–40. https://doi.org/10.1093/sleep/25.5.530.
Yiu Y, Tibbetts KM, Simpson CB, Matrka LA. Shar Pei larynx: supraglottic and postcricoid mucosal redundancy and its association with medical comorbidities. Ann Otol Rhinol Laryngol. 2019;128:121–7.
Da Cunha MGB, Passerotti GH, Weber R, Zilberstein B, Cecconello I. Voice feature characteristic in morbid obese population. Obes Surg. 2011;21:340–4. https://doi.org/10.1007/s11695-009-9959-7.
Hamdan AL, Safadi B, Chamseddine G, Kasty M, Turfe ZA, Ziade G. Effect of weight loss on voice after bariatric surgery. J Voice. 2014;28:618–23. https://doi.org/10.1016/j.jvoice.2014.03.004.
WHO expert consultation. Public health appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–63.
Dedhia RC, Rosen CA, Soose RJ. What is the role of the larynx in adult obstructive sleep apnea? Laryngoscope. 2014;124:1029–34. https://doi.org/10.1002/lary.24494.
Yamashiro Y, Kryger M. Is laryngeal descent associated with increased risk for obstructive sleep apnea?. Chest. 2012;141:1407–13. https://doi.org/10.1378/chest.10-3238.
Kezirian EJ, White DP, Malhotra A, Ma W, McCulloch CE, Goldberg AN. Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol. 2010;136:393–7. https://doi.org/10.1001/archoto.2010.26.
Solomon NP, Helou LB, Dietrich-Burns K, Stojadinovic A. Do obesity and weight loss affect vocal function? Semin Speech Lang. 2011;32:31–42. https://doi.org/10.1055/s-0031-1271973.
Hamdan AL, Al-Barazi R, Tabri D, Saade R, Kutkut I, Sinno S, et al. Relationship between acoustic parameters and body mass analysis in young males. J Voice. 2012;26:144–7. https://doi.org/10.1016/j.jvoice.2011.01.011.
Friedman AD. Adiposity, estrogen, and voice: the opera has just begun. Menopause. 2011;18:723–4. https://doi.org/10.1097/gme.0b013e31821f7ee9.
Yanagisawa E, Estill J, Mambrino LTD. Supraglottic contributions to pitch raising. Videoendoscopic study with spectroanalysis. Ann Otol Rhinol Laryngol. 1991;100:19–30.
Roers F, Mürbe D, Sundberg J. Voice classification and vocal tract of singers: a study of x-ray images and morphology. J Acoust Soc Am. 2009;125:503–12. https://doi.org/10.1121/1.3026326.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Lahav, Y., Adi, M., Arberboy, E. et al. Relations between body mass index, laryngeal fat pads, and laryngeal airway configuration in adult men population. Int J Obes 45, 288–295 (2021). https://doi.org/10.1038/s41366-020-0631-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0631-6