Abstract
Background:
Levels of bone turnover markers (BTM) might be correlated with outcome in terms of skeletal-related events (SRE), disease progression, and death in patients with bladder cancer (BC) and renal cell carcinoma (RCC) with bone metastases (BM). We try to evaluate this possible correlation in patients who receive treatment with zoledronic acid (ZOL).
Methods:
This observational, prospective, and multicenter study analysed BTM and clinical outcome in these patients. Serum levels of bone alkaline phosphatase (BALP), procollagen type I amino-terminal propeptide (PINP), and beta-isomer of carboxy-terminal telopeptide of type I collagen (β-CTX) were analysed.
Results:
Patients with RCC who died or progressed had higher baseline β-CTX levels and those who experienced SRE during follow-up showed high baseline BALP levels. In BC, a poor rate of survival was related with high baseline β-CTX and BALP levels, and new SRE with increased PINP levels. Cox univariate analysis showed that β-CTX levels were associated with higher mortality and disease progression in RCC and higher mortality in BC. Bone alkaline phosphatase was associated with increased risk of premature SRE appearance in RCC and death in BC.
Conclusion:
Beta-isomer of carboxy-terminal telopeptide of type I collagen and BALP can be considered a complementary tool for prediction of clinical outcomes in patients with BC and RCC with BM treated with ZOL.
Similar content being viewed by others
Main
The skeleton is the third most frequent site of tumour metastases, behind lung and liver, and often the only site where metastases of advanced solid tumours develop. Bone metastases (BM) are observed in ∼80% of patients with advanced-stage malignant tumours (Coleman et al, 2011). Thirty percent of patients with renal cell carcinoma (RCC) are diagnosed with BM, and another one-third of all patients will develop them throughout their disease period, even after undergoing nephrectomy (Wood and Brown, 2012), meaning a majority of RCC patients will suffer BM at some point of time. An estimated 40% of patients with bladder carcinoma (BC) develop BM. As of diagnosis of BM, the median survival of these patients is 12 months in RCC patients and 6–9 months in BC patients (Selvaggi and Scagliotti, 2005).
Bone metastases are associated with skeletal-related events (SRE) such as pathological fractures, spinal cord compression, severe bone pain, and hypercalcemia. Skeletal-related events can dramatically impair quality of life, and therefore appropriate management of cancer patients includes preservation of bone health.
Balance between bone resorption and bone formation is required for maintenance of bone metabolism. This equilibrium is altered by BM, which can produce an increase not only in bone formation but also in the destruction of bone. Bone metastases from RCC and BC are lytic in nature, and the increase in bone resorption is compensated by an increase in bone formation. Bone metabolism can be reflected by bone turnover markers (BTM). Previous studies have demonstrated that some BTM can alert to the existence of BM (Zhao et al, 2011), but their correlation with clinical outcomes is contradictory in different studies.
Several studies have demonstrated that bisphosphonates can reduce SRE, resulting from BM, as they are bone-targeted agents that inhibit osteoclast-mediated osteolysis and, hence, are currently being recommended as standard therapy. Although several bisphosphonates, which prevent SRE in patients with cancer and BM are available, zoledronic acid (ZOL) is the first such agent with proven efficacy for the prevention of SRE in patients with BM from breast cancer, prostate cancer (PC), and other solid tumours (Saad et al, 2012). Some authors had stated previously that ZOL could be an effective treatment for reducing morbidity in advanced RCC with BM (Zekri et al, 2001) and it has been proven in subsequent studies (Lipton et al, 2003).
The aim of this work was to study levels of two bone formation markers, bone alkaline phosphatase (BALP) and procollagen type I amino-terminal propeptide (PINP), and one marker of bone resorption, beta-isomer of carboxy-terminal telopeptide of type I collagen (β-CTX), in a population of patients with RCC or BC and bone metastases. The markers were studied at baseline and at 3, 6, 9, 12, 15, and 18 months after the beginning of treatment with ZOL. The relationship of these markers with mortality, disease progression, and SRE was also analysed.
Materials and methods
Study group
The TUGAMO study (‘Tumores UroGenitales Avanzados y Marcadores Óseos’, or advanced urogenital tumours and BTM) was performed in patients with PC, BC, and RCC with bone metastases between 2009 and 2011. This article is a sub-analysis of this study about BC and RCC patients. This was an observational, prospective, and national multicenter study. The study enroled patients ⩾18 years of age with histologically confirmed BC or RCC, and at least one diagnosed bone lesion confirmed by scintigraphy. Patients were excluded from the study if they presented with concomitant pathologies that could interfere in the evaluation of BTM, such as bone metabolic disorders, Paget’s disease of bone, hyperparathyroidism, thyroid abnormalities, abnormal intestinal absorption, or hepatic or renal dysfunction. Patients treated with bisphosphonates prior to their inclusion in the study and those with dental infection or diagnosis of osteonecrosis of the jaw were also excluded.
A follow-up of the patients was performed over 18 months. Baseline values (visit 0, v0) were those obtained when a patient initiated treatment with ZOL (Zometa, Novartis Pharma, Basel, Switzerland), 4 mg intravenous every 4 weeks for over 18 months. In all cases, anticancer treatment could be changed as clinically indicated throughout the course of the study. Data were collected at v0, v1 (3 months), v2 (6 months), v3 (9 months), v4 (12 months), v5 (15 months), and v6 (18 months). The definition of SRE was the first of any of the following events: pathological fractures, severe pain (which needed major analgesics, radiotherapy or surgery for its treatment), hypercalcemia, and spinal cord compression. Patients were also evaluated for disease progression by physical examination, and Eastern Cooperative Oncology Group performance status and pain score.
This study was conducted in accordance with the guidelines of the Declaration of Helsinki and Good Clinical Practice Guidelines and the protocol was approved by the Ethics Committee of the Hospital Clínico of Barcelona (Spain). Patients were given verbal and written information and gave their informed consent to participate in the study.
Analytical methods
Bone turnover markers were determined in serum. Blood was collected between 0800 and 1000 hours in a fasting state. Serum was kept at −80 °C until the moment of markers determination.
Bone alkaline phosphatase was determined by ELISA (IDS, Tyne & Wear, UK). Assay sensitivity was 0.7 μg l−1. The normal range for healthy adult men was ⩽15 UI l−1.
Procollagen type I amino-terminal propeptide was determined by electrochemiluminescence (Elecsys, Roche, Mannheim, Germany). Assay sensitivity was 5 μg l−1. The normal range for healthy adult men was ⩽62 ng ml−1.
Beta-isomer of carboxy-terminal telopeptide of type I collagen was determined by electrochemiluminescence (Elecsys, Roche). Assay sensitivity was 0.07 ng ml−1. The normal range for healthy adult men was ⩽0.548 ng ml−1.
Statistical analyses
Bone marker values were presented in terms of mean, standard deviation, median, and quartiles. Absolute and relative changes in bone markers as compared with baseline and previous visit were assessed at each visit. Absolute changes were summarised by mean and standard deviation, and their statistical significance was assessed using the Wilcoxon test for paired samples. Log transformation was performed for the relative changes obtained, and these were summarised by geometric mean and standard deviation. Statistical significance was assessed using the Student’s t-test for paired samples. Receiver operating characteristic (ROC) curves were used to assess the predictive power of BTM levels for mortality, SRE, and progression. Specifically, baseline levels and relative changes at 3 months from baseline were taken as potential predictors. To assess the association between these potential predictors and time to death, time to first SRE and time to progression, a survival analysis was performed using the Kaplan–Meier method and comparisons were performed using the log-rank test. Finally, Cox regression models were fitted to quantify the degree of association between potential predictors and mortality, occurrence of SRE, and progression according to Kaplan–Meier results. The models were summarised by hazard ratio estimate, standard error, and 95% confidence interval for hazard ratio. Also, the P-value obtained from hypothesis testing of the hazard ratio was shown. The significance level was set at 0.05 for all tests.
Data were analysed with SAS, version 9.1.3. for Windows (SAS Analytics, Madrid, Spain) and STATA, 4.0 for Windows (StataCorp, London, UK).
Results
Patient demographics
Thirty-nine patients with RCC and BM, and thirty-four patients with BC and BM were included in the study. Table 1 shows the demographics and baseline disease characteristics of the patients studied.
Global survival, defined as the time between the beginning of the 18-month ZOL treatment and death, showed a median value of 10 months in RCC (2.4–17.5) and 8.9 months in BC (2.6–15.3). Thirty-nine patients commenced RCC study and thirty-four patients began BC study; out of them five and three patients completed it, respectively. Losses of participants (RCC/BC) were due to death (21/19), loss of informed consent (0/1), loss to follow-up (1/1), clinical criteria (5/2), and others (e.g., change of address, renal insufficiency, and progression—1/2). No patients presented with osteonecrosis of the jaw or other severe secondary effects during follow-up.
Evolution of bone markers
The correlation among the markers in RCC (β-CTX, PINP, and BALP) was strong at v1 and v2 (P<0.007), decreasing all values. In BC, β-CTX and BALP showed a strong correlation at v1 (P=0.02), BALP and PINP at v0 (P=0.03), and β-CTX and PINP at v1, v2, and v3 (P<0.03).
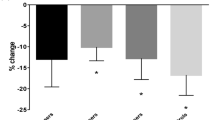
Most patients with abnormal BTM levels showed a decrease in levels after ZOL treatment. During the first six months, levels of BTM tended to decrease significantly in both patient groups (Figures 1 and 2).
Bone turnover marker evolution during follow-up in RCC patients. (A) Beta-isomer of carboxy-terminal telopeptide of collagen I (β-CTX); (B) bone alkaline phosphatase (BALP); (C) procollagen type I amino-terminal propeptide (PINP). Values (y-axis) are shown as median and standard deviation (BALP and PINP in μg l−1, and β-CTX in ng ml−1). At x-axis, time of follow-up (months) and number of patients alive (n) are shown. **Statistically significant differences with respect to baseline levels (P<0.05).
Bone turnover marker evolution during follow-up in BC patients. (A) Beta-isomer of carboxy-terminal telopeptide of collagen I (β-CTX); (B) bone alkaline phosphatase (BALP); (C) procollagen type I amino-terminal propeptide (PINP). Values (y-axis) are shown as median and standard deviation (BALP and PINP in μg l−1, and β-CTX in ng ml−1). At x-axis, time of follow-up (months) and number of patients alive (n) are shown. **Statistically significant differences with respect to baseline levels (P<0.05).
In RCC, β-CTX was the marker which experienced the greatest decrease and all patients showed normalisation in v1 (P=0.007). All patients remained normal during follow-up, except one patient who got a change for the worse in v3 and died. Bone alkaline phosphatase showed normalisation in v2 in 76.5% of patients (P=0.04), but six patients still showed abnormal values and one patient got a change for the worse and died. Changes in PINP values were not statistically significant in v1, with five patients with abnormal values and four patients with worse values.
In BC, following ZOL treatment, 65% of patients exhibited improved β-CTX and two patients got worse (P=0.02) in v1. Bone alkaline phosphatase had improved in 53% of patients at v1 (P=0.01) and three patients remained with abnormal values. Procollagen type I amino-terminal propeptide did not show statistically significant changes. Only the three first visits were analysed because the number of patients was too low at subsequent visits. Levels of PINP and β-CTX at v2 decreased by 73 and 75%, respectively (P<0.003). Bone alkaline phosphatase showed a decrease of 44% at v1 (P=0.02).
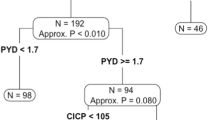
Bone markers as predictors of mortality risk, disease progression, and SRE appearance
Receiver operating characteristic analyses were performed to evaluate BTM as predictors of mortality risk, disease progression, and SRE appearance. Two different values were used as a cutoff point: baseline BTM levels and respective changes between v0 and v1 BTM levels. The sensitivity, specificity, and positive and negative predictive values of each BTM in each disease was found. The areas under the curve (AUC) were low for prediction mortality risk in RCC patients (<0.6), but AUC was 0.769 for basal β-CTX levels for prediction of disease progression and 0.719 for basal PINP levels for prediction of SRE. For BC patients, AUC for basal BALP levels was 0.801 for prediction of mortality risk and 0.716 for prediction of SRE. The other AUC were too low.
Kaplan–Meier curves (KMc) were performed with four categories:
-
a)
Baseline BTM normal or abnormal (defined as higher than the upper limit of normality).
-
b)
Basal BTM ‘higher’ or ‘equal to or less than’ the cutoff obtained in the ROC curves (ROC cutoff or ROC-CO).
-
c)
Relative changes between v0 and v1 (v1/v0) ‘higher than’ or ‘equal to or less than’ ROC-CO.
-
d)
Presence or absence of a normal BTM level at v1.
In RCC patients, KMc showed a significantly diminished survival rate in patients with abnormal baseline β-CTX and in those with higher β-CTX values than ROC-CO. Both groups also exhibited an increase in disease progression. Baseline BALP levels higher than ROC-CO showed a close relation with lesser time until SRE appearance. Statistically significant KMc are shown in Figure 3.
Kaplan–Meier analysis after the completion of treatment (18 months) with ZOL in RCC patients. (A) β-isomer of carboxy-terminal telopeptide of collagen I (β-CTX) and overall survival. Stratification was performed using ‘normal or abnormal baseline marker values’ against death. (B) β-CTX and overall survival. Stratification was performed using the cutoff point obtained from the ROC curves of ‘baseline values of biomarkers at the beginning of the study’ against death. (C) β-CTX and disease progression. Stratification was performed using ‘normal or abnormal baseline marker values’ against death. (D) β-CTX and disease progression. Stratification was performed using the cutoff point obtained from the ROC curves of ‘baseline values of biomarkers at the beginning of the study’ against death. (E) Bone alkaline phosphatase (BALP) and new SRE. Stratification was performed using the cutoff point obtained from the ROC curves of ‘baseline values of biomarkers at the beginning of the study’ against death.
Moreover, in BC patients, KMc showed a different survival rate in patients with higher β-CTX and BALP levels using ROC-CO. Patients whose PINP levels changed relatively between v0 and v1 had a KMc that showed a lower time until new SRE appearance. No significant differences were found in KMc regarding progression. These statistically significant results are shown in Figure 4.
Kaplan–Meier analysis after the completion of treatment (18 months) with ZOL in BC patients. (A) β-isomer of carboxy-terminal telopeptide of collagen I (β-CTX) and overall survival. Stratification was performed using the cutoff point obtained from the ROC curves of ‘baseline values of biomarkers at the beginning of the study’ against death. (B) Bone alkaline phosphatase (BALP) and overall survival. Stratification was performed using the cutoff point obtained from the ROC curves of ‘baseline values of biomarkers at the beginning of the study’ against death. (C) Amino-terminal propeptide of procollagen I (PINP) and new SRE. Stratification was performed using relative changes between visit 0 and visit 1 (v1/v0) in relation to cutoff point obtained from the ROC curves against death.
Univariate Cox regression was derived from the above-mentioned KMc. Table 2 shows the hazard ratios for RCC patients and Table 3 shows the hazard ratios for BC patients. In RCC, higher β-CTX levels were related with death and a poor prognosis for disease progression. Higher levels of BALP were associated with premature SRE. In BC, higher β-CTX and BALP levels were also related with death. The Cox regression regarding progression could not be made because no significant differences were found in KMc. Procollagen type I amino-terminal propeptide did not show being associated with outcomes.
Discussion
The usefulness of BTM as tool for the diagnosis of BM in many types of cancers has been investigated previously (Coleman et al, 2011; Huang and Ouyang, 2012). Many studies have analysed their relationship with clinical outcomes (Mountzios et al, 2010; Kamiya et al, 2010; Zaghloul et al, 2010; Coleman et al, 2011; Jung et al, 2011; Saad et al, 2012), as well as their clinical importance (Coleman et al, 2010; Armstrong et al, 2012). However, only a few articles have analysed the usefulness of BTM in RCC and less in BC, and there is no consensus among these studies as to which BTM is the ideal marker. Recently, the International Osteoporosis Foundation and the International Federation of Clinical Chemistry and Laboratory Medicine have recommended PINP and β-CTX as reference markers in all clinical studies (Vasikaran et al, 2011), and we have used them in our study previously to this recommendation. The utility of BTM as markers of the presence of BM before their appearance in the bone scintigraphy has been taken up in many studies (Zhao et al, 2011). In the case of RCC and BC, BTM utility is more important because early bone metastatic lesions in these tumours may not be easily detected by scintigraphy due to their lytic nature (Wood and Brown, 2012). In one study (Kleipzig et al, 2008), they found that PINP was a good predictor of BM in patients with RCC. In two studies (Ramankulov et al, 2007, 2008), these authors analysed osteopontin (a bone-related protein) and serum amyloid A, finding that both were unspecific markers in relation to the number or localisation of metastatic lesions in patients with RCC. Other authors (Okamura et al, 2003) found that ICTP (a telopeptide of collagen type I) can detect BM in genitourinary cancers. In a study of BC patients (Zissimopoulos et al, 2009), PICP (similar to PINP) showed a significant difference between patients with or without BM. In spite of these results, in a recent review (Huang and Ouyang, 2012) they concluded that, currently, no BTM can predict occurrence of BM in the absence of bone imaging techniques, and that more prospective trials are needed to assess this possibility. We are currently unable to answer this question, because all our patients were previously diagnosed with BM. To date, no study has provided a definitive answer to this question about BTM and premature diagnosis of BM in RCC.
In the current work, we have demonstrated that patients with RCC and BM and elevated baseline β-CTX levels had a higher risk of death and a higher estimated risk of disease progression than those patients whose levels were normal or lower than ROC-CO. When baseline BALP levels were higher than ROC-CO, the estimated risk of premature SRE was also elevated. Procollagen type I amino-terminal propeptide was not associated with analysed clinical outcomes.
No study has arrived at the same conclusions as these regarding RCC. Some authors (Ramankulov et al, 2007, 2008) have found that osteopontin, serum amyloid A, and presence of distant metastases were independent survival predictors in RCC. Other articles (Vermaat et al, 2010) found the same results about amyloid A and added to that elevated levels of apolipoprotein-A2 and transthyretin were associated with better prognosis. Other authors (Kume et al, 2011) collected RCC cases and found an association between total alkaline phosphatase and overall survival. Another one (Jung et al, 2006) had found that osteoprotegerin was predictive of cancer-specific survival in a multivariate model. In a study with a variety of solid tumours, including RCC, a multicenter study (Coleman et al, 2005) found that increased values of BALP and NTX (amino-terminal telopeptide of collagen I) were associated with increased risk of death, SRE, and disease progression in patients with breast cancer, PC, myeloma, non-small-cell lung cancer and other solid tumours, treated with bisphosphonates. Similar results had been found by the same authors about NTX in bisphosphonates naive patients (Brown et al, 2005).
As for patients with BC, an increased risk of death was associated with high baseline β-CTX and BALP levels. Only one similar result has been found previously (López-Carrizosa et al, 2010), but the lower number of patients (2) made the results of the study unreliable. Other authors (Ang et al, 2005) had found a relation between osteopontin levels and stage of disease previously. Although the current study is limited by the small number of cases in the study groups, this is the first report in the literature showing a relationship between BTM, BC, and clinical outcome.
As in our study, other authors have found relationships between different tumours, clinical outcomes, and β-CTX. In patients with PC, increased BTM levels (especially PINP and ICTP, a resorption marker) have been related with survival, disease progression, and SRE (Jung et al, 2011). Other authors (Zhao et al, 2011) studied patients with PC and lung- and breast carcinoma. According to their data, β-CTX and BALP can be considered to be good markers for detecting BM. In addition, high values of PINP were related with poor rates of survival.
Procollagen type I amino-terminal propeptide did not show a statistically significant relation in either of the two cancers in our study. The findings in KMc about relation between progression and relative changes in PINP values in BC are not corroborated to Cox regression, and it can be explained for low number of patients in this group. Further studies with more patients are necessary to support our findings.
Other markers have been well established as prognostic factors in RCC, such as Motzer criteria (haemoglobin, Karnowsky performance status, time from diagnosis to treatment with interferon-alpha, lactate dehydrogenase, and corrected serum calcium) (Motzer et al, 2002) or Heng criteria (haemoglobin, time from diagnosis to treatment with interferon-alpha, corrected serum calcium, neutrophils and platelets number) (Heng et al, 2009). In BC, Eastern Cooperative Oncology Group performance status and the presence of visceral metastasis have been associated with decreased survival (Bellmunt et al, 2002). The main limitation of our study is the small sample size of each of the groups (39 RCC and 34 BC), which are far too small to do multivariable analysis to determine if the BTM are independently predictive of important clinical outcomes when these known prognostic factors (Bellmunt et al, 2002; Motzer et al, 2002; Heng et al, 2009), history of prior SRE, other bone-associated markers, and treatment effects are considered all together. Future studies will have to address this point.
Conclusions
Beta-isomer of carboxy-terminal telopeptide of type I collagen and BALP can be considered promising prognostic factors of clinical outcome in patients with RCC and BC with BM treated with ZOL and they can be one more tool to those existent previously. Metastatic bone disease in RCC and BC may benefit from greater focus than it has to date, and their use may bring about an important advance in the management of these patients. More studies in larger groups of patients are necessary for further confirmatory research.
Change history
09 July 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Ang C, Chambers AF, Tuck AB, Winquist E, Izawa JI (2005) Plasma osteopontin levels are predictive of disease stage in patients with transitional cell carcinoma of the bladder. BJU Int 96: 803–805.
Armstrong AJ, Eisenberger MA, Halabi S, Oudard S, Nanus DM, Petrylak DP, Sartor AO, Scher HI (2012) Biomarkers in the management and treatment of men with metastatic castration-resistant prostate cancer. Eur Urol 61: 549–559.
Bellmunt J, Albanell J, Paz-Ares L, Climent MA, González-Larriba JL, Carles J, de la Cruz JJ, Guillem V, Díaz-Rubio E, Cortés-Funes H, Baselga J Spanish Oncology Genitourinary Group (2002) Pretreatment prognostic factors for survival in patients with advanced urothelial tumors treated in a phase I/II trial with paclitaxel, cisplatin, and gemcitabine. Cancer 95: 751–757.
Brown JE, Cook RJ, Major P, Lipton A, Saad F, Smith M, Lee KA, Zheng M, Hei YJ, Coleman RE (2005) Bone turnover markers as predictors of skeletal complications in prostate cancer, lung cancer, and other solid tumors. J Natl Cancer Inst 97: 59–69.
Coleman R, Costa L, Saad F, Cook R, Hadji P, Terpos E, Garnero P, Brown J, Body JJ, Smith M, Lee KA, Major P, Dimopoulos M, Lipton A (2011) Consensus on the utility of bone markers in the malignant bone disease setting. Crit Rev Oncol Hematol 80: 411–432.
Coleman RE, Lipton A, Roodman GD, Guise TA, Boyce BF, Brufsky AM, Clézardin P, Croucher PI, Gralow JR, Hadji P, Holen I, Mundy GR, Smith MR, Suva LJ (2010) Metastasis and bone loss: advancing treatment and prevention. Cancer Treat Rev 36: 615–620.
Coleman RE, Major P, Lipton A, Brown JE, Lee KA, Smith M, Saad F, Zheng M, Hei YJ, Seaman J, Cook R (2005) Predictive value of bone resorption and formation markers in cancer patients with bone metastases receiving the bisphosphonate zoledronic acid. J Clin Oncol 23: 4925–4935.
Heng DY, Xie W, Regan MM, Warren MA, Golshayan AR, Sahi C, Eigl BJ, Ruether JD, Cheng T, North S, Venner P, Knox JJ, Chi KN, Kollmannsberger C, McDermott DF, Oh WK, Atkins MB, Bukowski RM, Rini BI, Choueiri TK (2009) Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol 27: 5794–5799.
Huang Q, Ouyang X (2012) Biochemical-markers for the diagnosis of bone metastasis: a clinical review. Cancer Epidemiol 36: 94–98.
Jung K, Lein M, Ringsdorf M, Roigas J, Schnorr D, Loening SA, Staack A (2006) Diagnostic and prognostic validity of serum bone turnover markers in metastatic renal cell carcinoma. J Urol 176: 1326–1331.
Jung K, Miller K, Wirth M, Albrecht M, Lein M (2011) Bone turnover markers as predictors of mortality risk in prostate cancer patients with bone metastases following treatment with zoledronic acid. Eur Urol 59: 604–612.
Kamiya N, Suzuki H, Yano M, Endo T, Takano M, Komaru A, Kawamura K, Sekita N, Imamoto T, Ichikawa T (2010) Implications of serum bone turnover markers in prostate cancer patients with bone metastasis. Urology 75: 1446–1451.
Klepzig M, Sauer-Eppel H, Jonas D, Oremek GM (2008) Value of procollagen type 1 amino-terminal propeptide in patients with renal cell carcinoma. Anticancer Res 28: 2443–2446.
Kume H, Kakutani S, Yamada Y, Shinohara M, Tominaga T, Suzuki M, Fujimura T, Fukuhara H, Enomoto Y, Nishimatsu H, Homma Y (2011) Prognostic factors for renal cell carcinoma with bone metastasis: who are the long-term survivors? J Urol 185: 1611–1614.
Lipton A, Zheng M, Seaman J (2003) Zoledronic acid delays the onset of skeletal-related events and progression of skeletal disease in patients with advanced renal cell carcinoma. Cancer 98: 962–969.
López-Carrizosa MC, Samper-Ots PM, Pérez AR (2010) Serum C-telopeptide levels predict the incidence of skeletal-related events in cancer patients with secondary bone metastases. Clin Transl Oncol 12: 568–573.
Motzer RJ, Bacik J, Murphy BA, Russo P, Mazumdar M (2002) Interferon-alfa as a comparative treatment for clinical trials of new therapies against advanced renal cell carcinoma. J Clin Oncol 20: 289–296.
Mountzios G, Terpos E, Syrigos K, Papadimitriou C, Papadopoulos G, Bamias A, Mavrikakis M, Dimopoulos MA (2010) Markers of bone remodeling and skeletal morbidity in patients with solid tumors metastatic to the skeleton receiving the biphosphonate zoledronic acid. Transl Res 155: 247–255.
Okamura T, Akita H, Tatsura H, Kawai N, Nagata D, Azemoto M, Iwase Y, Kohri K (2003) The efficacy of a serum carboxyterminal pyridinoline cross-linked telopeptide of type I collagen as a quantitative screening marker for bone metastases in patients with urological malignancies. Cancer Detect Prev 27: 14–18.
Ramankulov A, Lein M, Johannsen M, Schrader M, Miller K, Loening SA, Jung K (2008) Serum amyloid A as indicator of distant metastases but not as early tumor marker in patients with renal cell carcinoma. Cancer Lett 269: 85–92.
Ramankulov A, Lein M, Kristiansen G, Meyer HA, Loening SA, Jung K (2007) Elevated plasma osteopontin as marker for distant metastases and poor survival in patients with renal cell carcinoma. J Cancer Res Clin Oncol 133: 643–652.
Saad F, Eastham JA, Smith MR (2012) Biochemical markers of bone turnover and clinical outcomes in men with prostate cancer. Urol Oncol 30: 369–378.
Selvaggi G, Scagliotti GV (2005) Management of bone metastases in cancer: a review. Crit Rev Oncol Hematol 56: 365–378.
Vasikaran S, Eastell R, Bruyère O, Foldes AJ, Garnero P, Griesmacher A, McClung M, Morris HA, Silverman S, Trenti T, Wahl DA, Cooper C, Kanis JA IOF-IFCC Bone Marker Standards Working Group (2011) Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: a need for international reference standards. Osteoporos Int 22: 391–420.
Vermaat JS, van der Tweel I, Mehra N, Sleijfer S, Haanen JB, Roodhart JM, Engwegen JY, Korse CM, Langenberg MH, Kruit W, Groenewegen G, Giles RH, Schellens JH, Beijnen JH, Voest EE (2010) Two-protein signature of novel serological markers apolipoprotein-A2 and serum amyloid alpha predicts prognosis in patients with metastatic renal cell cancer and improves the currently used prognostic survival models. Ann Oncol 21: 1472–1481.
Wood SL, Brown JE (2012) Skeletal metastasis in renal cell carcinoma: current and future management options. Cancer Treat Rev 38: 284–291.
Zaghloul MS, Boutrus R, El-Hossieny H, Kader YA, El-Attar I, Nazmy M (2010) A prospective, randomized, placebo-controlled trial of zoledronic acid in bony metastatic bladder cancer. Int J Clin Oncol 15: 382–389.
Zekri J, Ahmed N, Coleman RE, Hancock BW (2001) The skeletal metastatic complications of renal cell carcinoma. Int J Oncol 19: 379–382.
Zhao H, Han KL, Wang ZY, Chen Y, Li HT, Zeng JL, Shen Z, Yao Y (2011) Value of C-telopeptide-cross-linked type I collagen, osteocalcin, bone-specific alkaline phosphatase and procollagen type I N-terminal propeptide in the diagnosis and prognosis of bone metastasis in patients with malignant tumors. Med Sci Monit 17: CR626–CR633.
Zissimopoulos A, Stellos K, Matthaios D, Petrakis G, Parmenopoulou V, Babatsikou F, Matthaiou E, Theodosiadou E, Hountis P, Koutis C (2009) Type I collagen biomarkers in the diagnosis of bone metastases in breast cancer, lung cancer, urinary bladder cancer and prostate cancer. Comparison to CEA, CA 15-3, PSA and bone scintigraphy. J BUON 14: 463–472.
Acknowledgements
As this was a multicenter study, Adknoma Health Research (Barcelona, Spain) collected and ordered data throughout the study. We especially thank Margarida Garcia from Adknoma who followed carefully the development of the study. And we thank Novartis Oncology Spain for supporting this study.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Alcaraz, A., González-López, R., Morote, J. et al. Biochemical markers of bone turnover and clinical outcome in patients with renal cell and bladder carcinoma with bone metastases following treatment with zoledronic acid: The TUGAMO study. Br J Cancer 109, 121–130 (2013). https://doi.org/10.1038/bjc.2013.272
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.272
Keywords
This article is cited by
-
Utility of urinary type I collagen cross-linked N-telopeptide as a prognostic indicator in breast cancer patients with bone metastases
Breast Cancer (2020)
-
No associations of 25-hydroxycholecalciferol and parathyroid hormone concentrations with calcaneal bone characteristics in community-dwelling elderly subjects: A cross-sectional study
The journal of nutrition, health & aging (2017)
-
Biochemical markers of bone turnover in patients with spinal metastases after resistance training under radiotherapy – a randomized trial
BMC Cancer (2016)