Abstract
Background
The use of conjunctiva autograft, adjunct antimetabolite therapy has been shown to be effective in preventing pterygium recurrence.
Objective
To compare 5 fluorouracil (5-FU) to conjunctival autograft in the treatment of large, fleshy pterygium.
Methods
A randomised controlled prospective study of outcome of pterygium treatment using 5-FU as adjuvant treatment compared to conjunctiva autograft. Thirty-five eyes with large pterygium treated with bare sclera conjunctival excision plus 5-FU were compared with 33 eyes treated with excision and conjunctival autograft alone.
Results
Post-operative pterygium recurrence was observed in four (11.4%) eyes treated with 5-FU and 4 (12.1%) eyes treated with conjunctiva autograft (P>0.05). The post-operative complications included, granuloma formation 11.4% for 5-FU and 3.0% for autograft and conjunctival discharge 5.7% for 5-FU group only.
Conclusion
5-FU is marginally superior to conjunctival autograft in the prevention of pterygium recurrence but neither gives a more desirable single digit recurrence rate. Randomised studies combining both conjunctival autograft and 5-FU in pterygium treatment is advocated to further explore their effect.
Similar content being viewed by others
Introduction
Pterygium is a degenerative lesion presenting as a fibro vascular conjunctival growth in the palpebral aperture of the eye with corneal extension. The aetiology of pterygium has been linked to exposure to ultraviolet irradiation, chronic irritation by dust, wind, and other environmental factors.1 Thus, it is more commonly seen among outdoor workers in tropical countries.2 Pterygium may be responsible for disturbance of vision by its astigmatic effect or by growing so large as to occlude the visual axis. It could also be a cause of much ocular irritation as well as being cosmetically unacceptable for many people especially when fleshy or inflamed. The treatment for pterygium is surgical excision. However, due to high recurrence rate with simple excision which could be as high as 40% in some cases,3 the use of adjunct therapy such as beta radiation, antimetabolites such as mitomycin-C and 5-fluorouracil (5-FU), and conjunctiva autograft have been advocated.4, 5
Both mitomycin-C and 5-FU have been shown to cause a reduction in recurrence rate of pterygium but they are both potentially toxic to ocular tissues and have been associated with some complications.6 Conjunctiva autograft on the other hand has been said to be free of complications and although takes longer to perform is said to be associated with little or no recurrence.7
The main objective of this study was to compare 5-FU to conjunctival autograft in the treatment of large, fleshy pterygium in terms of preventing recurrence as well as relative safety and complication rate.
Materials and methods
A randomised controlled and prospective study of outcome of pterygium treatment using 5-FU as adjuvant treatment compared to conjunctiva autograft carried out at the University College Hospital Ibadan, between May 2003 and June 2005.
Selection of patients
All patients seen with fleshy pterygium encroaching 2 mm or more into cornea were selected and randomised into one of the two groups.
Sample size was calculated from estimation of proportions with assumption of success rate of about 80% for 5-FU and expected success rate of 100% for conjuctival autograft, alpha error, 0.05%, and a power of 90%.

The sample size was increased to 80 to take care of dropouts. Following adequate explanation and obtaining of consent, the subjects were randomised into their respective groups using a ‘lucky dip’ technique. Small folded sheets of paper numbered 1–40 and 41–80 were kept in two separate envelopes (for male patients and female patients, respectively). Male and female patients who met the selection criteria were requested to pick one folded sheet of paper from the appropriate envelope as they presented to the clinic consecutively. Those who picked odd numbers were assigned to 5-FU while even numbers were assigned to conjunctiva autograph. For patients with bilateral pterygium, the worse eye was randomised first and the other eye was assigned to the alternative group as a control.
Data collection and operation procedure
Information obtained from subjects using a structured questionnaire included age, sex, occupation, eye affected, location, morphology, size of pterygium from limbus (measured with a slit lamp), vision of eye to be operated, information on previous pterygium surgery performed.
All patients received sub-conjunctival 2% lignocaine with adrenaline, for local anaesthesia. Pterygium tissue was excised from cornea with bard parker blade under microscope and was subsequently bluntly dissected from over lying conjunctiva and underlying sclera. The use of cautery too was minimised.
5-FU group
The 5-FU group after an initial pterygium excision had the bare scleral area of the pterygium bed exposed to a section of a Weck-cel sponge soaked in 50 mg/ml of 5-FU for 5 min during which there was intermittent wetting of the sponge every minute with a drop of 5-FU, at the end of 5 min, the sponge was removed and discarded and the eye copiously irrigated with saline solution for about 1 min. The cut conjunctiva ends were anchored to sclera with 8–0 silk suture.
Conjunctiva graft procedure
The conjunctiva autograft group after an initial pterygium excision had a conjunctiva free graft of a size equivalent to the scleral defect excised from the pterygium free superior 12 O'-clock bulbar conjunctiva inclusive of limbal conjunctiva and 0.5 mm of clear cornea of the same eye. There after the free graft was sutured to the recipient bed with interrupted 8–0 sutures taking care to ensure proper orientation of the ends of the graft (cornea end of the graft sutured to the recipient cornea).
Postoperatively, both groups had instillation of antibiotic ointment and dexametasone (steroid) drops postoperatively for between 8 and 10 weeks, depending on duration of inflammation. Follow-up visits were at post op days 1, 7, 21, monthly for 2 months and every 3months for between 1 and 2 years.
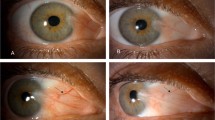
Recurrence of pterygium was defined as growth of fibro vascular tissue 1 mm or more into cornea as observed with a slit lamp.
Data collected were analysed with the aid of a personal computer using SPSS version 10.
Results
A total of 68 eyes of 62 subjects where studied. 12 eyes that were initially randomised and included in the study did not show up for surgery. Thirty-five eyes were treated with 5-FU (16 male patients and 19 female patients) while 33 eyes were treated with conjuctival autograft (19 male patients and 14 female patients). The mean age of the 5-FU group was 49 years while that for the autograft group was 45.7 years (P>0.05). All the treated pterygia where large and fleshy, and extended from 2 mm to over 4 mm into the cornea in size. About 57.2% of eyes treated with 5-FU compared to 90% of those treated by autograft ranged from 2 to 4 mm in size while the remainder were over 4 mm in size. There were five recurrent pterygia included in the study, two were treated by 5-FU while three were treated by autograft.
Postoperatively pterygium recurrence was observed in four (11.4%) eyes treated with 5-FU and four (12.1%) eyes treated with conjunctiva autograft (P>0.05). All recurrences were observed between the third and fifth postoperative visits (2–8 months post op) for conjunctiva autograft and between fourth and fifth post op visit (3–8 months post op) for the 5-FU group. Examination of the profile of eyes with pterygium recurrence showed that five out of the eight were between 2 and 4 mm in size pre op, while 2 were over 4 mm in size pre op, all were fleshy but 2 were also inflamed while only one (from the autograft group) had previously been operated by the bare sclera technique. Table 1 shows the detailed profile of eyes that developed pterygium recurrence.
Postoperative complications observed among the studied eyes included granuloma formation 11.4% for 5-FU and 3.0% for autograft and surface infection 5.7% for 5 FU only (Table 2).
Discussion
This study has observed comparable rates of 88.6 and 87.9%, respectively, for the successful treatment of large and fleshy pterygia using either 5-FU or conjunctival autograft. Although 5-FU appears to be marginally superior to conjunctival autograft in preventing recurrence, both are however, far from having desirable success rates of 100%. The recurrence rate of 11.4% obtained by intraoperative application of 50 mg/ml of 5-FU for 5 min was marginally better than 12.4% observed for conjuctival autograft, the difference was however, not statistically significant. Less time is also spent in applying 5-FU (5 min) than conjunctiva autograft (20–30 min, although this could be reduced with use of fibrin tissue glue when it is available). Conjunctiva autograft, however, has an edge over 5-FU in that it is much cheaper and has fewer complications associated with it.
The recurrence rate from 5-FU observed in this study is lower than the 14% recurrence observed by Akarsu et al8 from combined intraoperative (3 min) application and postoperative injection of 25 mg/ml of 5-FU. The recurrence rate following autograft was also lower than 18% reported by Wang and Law9 and 14.6% for recurrent pterygium by Mutlu et al.10 Mitomycin C is reported11 to be more effective in preventing pterygium recurrence than conjunctiva autograft but cost and associated side effects are factors, which could limit its use. 5-FU is cheaper than mitimycin C and is associated with fewer side effects. Although 5-FU appears to be marginally superior to conjunctiva autograft in the prevention of pterygium neither gives a recurrence of near zero percent. Thus more randomised studies possibly combining 5-FU with autograft are desirable. Such a combination may have fewer side effects than treatment with mitomycin C but possibly better prevention of pterygium recurrence than either 5-FU or autograft alone.
Five subjects with previous pterygium recurrence following use of other surgical methods were included in the study because excluding them would have reduced the number of cases available for analysis. Their presence is, however, not likely to bias the study because they were evenly distributed between the two study groups.
Conclusion
5-FU is marginally superior to conjunctiva autograft in the prevention of pterygium recurrence but neither gives 100% success rate, randomised studies combining both conjuctival autograft and 5-FU in pterygium treatment are desirable.
References
Cameron ME . Pterygium throughout the world. Charles C. Thomas publisher: Springfield, Illinois, 1965.
Detels R, Dhir SP . Pterygium—a geographical study. Arch Ophthalmol 1967; 78: 485–491.
Ashaye AO . Ptrygium in Ibadan. WAJM 1991; 10(3): 232–243.
Amano SAU, Motoyama YAU, Oshika TAU, Eguchi SAU, Eguchi K . Comparative study of intraoperative mitomycin C and beta irradiation in pterygium surgery. Br J Ophthalmol 2000; 84(6): 618–621.
Pikkel JAU, Porges YAU, Ophir A . Halting pterygium recurrence by postoperative 5-fluorouracil. Cornea 2001; 20(2): 168–171.
Morrow GL, Stein RM, Heathcote JG, Ikeda-Douglass JV, Feldman F . Ocular toxicity of mitomycin C and 5-fluorouracil in the rabbit. Can J Ophthalmol 1994; 29(6): 268–273.
Prabhasawat P, Barton K, Burkett G, Tseng SCG . Comparison of conjunctival auto grafts, amniotic membrane grafts and primary closure for pterygium excision. Ophthalmology 1997; 104(6): 974–985.
Akarsu C, Taner P, Ergin A . 5-Fluorouracil as chemo adjuvant for primary pterygium surgery: preliminary report. Cornea 2003; 22(5): 522–526.
Wang VA, Law FCH . Use of motomycin C with conjuctival auto graft in pterygium surgery in Asian-n Canadians. Ophthalmology 1999; 106(8): 1512–1515.
Mutlu FM, Sobaci G, Tatar T, Yidirim E . A comparative study of recurrent pterygium surgery: limbal conjunctival auto graft transplantation versus mitomycin C with conjunctival flap. Ophthalmology 1999; 106(4): 817–821.
Mahar PS . Conjunctival auto graft versus topical mitomycin C in treatment of pterygium. Eye 1997; 11: 790–792.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bekibele, C., Baiyeroju, A., Olusanya, B. et al. Pterygium treatment using 5-FU as adjuvant treatment compared to conjunctiva autograft. Eye 22, 31–34 (2008). https://doi.org/10.1038/sj.eye.6702480
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702480
Keywords
This article is cited by
-
Anti-fibrotic, anti-VEGF or radiotherapy treatments as adjuvants for pterygium excision: a systematic review and network meta-analysis
BMC Ophthalmology (2017)
-
Developments and current approaches in the treatment of pterygium
International Ophthalmology (2017)
-
5-Fluorouracil vs avastin as adjunct to conjunctival autograft in the surgical treatment of pterygium
Eye (2016)
-
Intra-lesional 5 fluorouracil for the management of recurrent pterygium
Eye (2013)
-
5-Fluorouracil versus mitomycin C as adjuncts to conjunctival autograft in preventing pterygium recurrence
International Ophthalmology (2012)