Abstract
Aims
To compare retinal nerve fibre layer (RNFL) measurements were carried out with two different versions of an optical coherence tomography device in patients with band atrophy (BA) of the optic nerve and in normal controls.
Methods
The RNFL of 36 eyes (18 with BA and 18 normals) was measured using an earlier version of an optical coherence tomography device (OCT-1). The measurements were repeated using a later version of the same equipment (OCT-3), and the two sets of measurements were compared.
Results
Using OCT-1, the peripapillary RNFL thickness (mean±SD, in μm) in eyes with BA measured 80.42±6.94, 99.81±14.00, 61.69±13.02, 101.70±12.54, and 57.36±16.52 corresponding to the total RNFL average, superior, temporal, inferior, and nasal quadrants, respectively. Using OCT-3, the corresponding measurements were 63.11±6.76, 81.22±13.34, 39.50±8.27, 86.72±15.16, and 45.05±8.03. Each of these measurements was significantly smaller with OCT-3 than with OCT-1. In normal eyes, RNFL average and temporal quadrant OCT-3 values were significantly smaller than OCT-1 values, but there was no significant difference in measurements from the superior, inferior, and nasal quadrant.
Conclusions
RNFL measurements were smaller with OCT-3 than with OCT-1 for almost all parameters in eyes with BA and in the global average and temporal quadrant measurements in normal eyes. Investigators should be aware of this fact when comparing old RNFL measurement with values obtained with later versions of the equipment.
Similar content being viewed by others
Introduction
Optical coherence tomography (OCT) is a non-invasive technique for the acquisition of cross-sectional images of retinal structures from which estimates of the thickness of retinal layers can be made. The ability of OCT to provide quantitative and reproducible measurements of the retinal nerve fibre layer (RNFL) has been demonstrated in experimental and clinical studies.1, 2, 3, 4 Although most of the clinical studies using OCT have been performed in patients with glaucoma,5, 6, 7, 8, 9 many other conditions have been studied, including band atrophy (BA) of the optic nerve from chiasmal compression.10, 11
The first commercially available OCT equipment (OCT-1, Humprey-Zeiss, Dublin, CA, USA) has been widely used and its ability to measure RNFL has been well documented.12, 13, 14 The second commercial version of the equipment presented only slight modifications, but the recently released third version (OCT-3, or Stratus-OCT, Carl Zeiss Meditec Inc., Dublin, CA, USA) brought significant improvements over the original version.15 As some patients examined with OCT-1 are likely to be examined with later versions of the equipment it is important to determine whether different versions produce comparable measurements in healthy and sick subjects. The purpose of this paper is to compare RNFL measurements obtained using two different versions of OCT, old (OCT-1) and new (OCT-3), when applied to patients with BA and to normal controls.
Patients and methods
Between December 2002 and December 2003, 36 eyes were presented to OCT-1 analysis of the peripapillary RNFL. In all, 18 eyes were from 18 consecutive patients (10 males and eight females) with BA of the optic nerve owing to previous (already treated) chiasmal compression caused by suprasellar tumours. The remaining 18 eyes were from 18 normal age- and sex-matched controls. Mean±SD age of patients with BA and healthy individuals was 45.70±15.83 and 45.58±14.06, respectively. Institutional Ethics Committee approval was obtained for the study and informed consent was obtained from all participants.
Visual field (VF) testing was performed using the Goldmann perimeter. The V-4-e, I-4-e, I-3-e, I-2-e, and I-1-e stimuli were used to draw the isopters. Patients were also submitted to standard automated perimetry (Humphrey, 24-2 Full-threshold test).
The inclusion criteria for the patients were: best corrected visual acuity of 20/30 or better in the study eye; complete temporal hemianopia on Humphrey perimetry and complete or almost complete temporal hemianopia on Goldmann perimetry; nasal hemifield within normal limits; spherical refraction within ±3 D; cylinder correction within ±3 D; intraocular pressure less than 22 mmHg; and reliable VF. A reliable Humphrey VF test was defined as one with fewer than 25% fixation losses, false-positive or false-negative responses. All patients had VF defects stable for at least 1 year. Patients with clinical signs of glaucoma were excluded. In 14 patients only one eye met the inclusion criteria. In four patients, one eye was chosen at random for the study. The control group consisted of normal healthy volunteers recruited from hospital staff members, with a normal ophthalmic examination including Humphrey perimetry.
VF and OCT-1 examinations were performed on the same day or within a maximum period of 2 weeks. OCT-1 examination was performed after pupillary dilatation to a minimum diameter of 5 mm. Circular 360-degree OCT scans were obtained with a diameter of 3.4 mm centered on the optic disc. The scan was initiated at the 9 O’ clock position and proceeded clockwise. Each scan consisted of 100 evenly distributed transverse A-scans along the circumference with an acquisition time of 1 s.
Three good-quality circular scans were taken around the centre of the optic disc in each eye. OCT software version A5 was used for analysis. The RNFL was differentiated from other retinal structures using the automated edge detection algorithm provided by the OCT software. The average RNFL thickness values were calculated globally and separately for the superior, inferior, temporal, and nasal quadrants (90 degrees each), and for the twelve 30-degree segments using OCT software. The average RNFL thickness value was calculated automatically by the OCT software. We examined both left and right eyes; left eyes were considered to be mirror images of right eyes. Therefore, when indicating the 30-degree segments as clock hours, we considered the hours from 1200 to 0600 as nasal hours, and those from 0600 to 1200 as temporal hours.
Within a maximum interval of 6 months, the same group of individuals was presented to a second OCT examination using a recent version of the same equipment (OCT-3). There was no significant change on a repeat VF test. We used the fast RNFL algorithm to obtain RNFL thickness measurements. Three images were acquired from each subject, each one consisting of 256 A-scans along a 3.4 mm-diametre circular ring around the optic disc. The parameters of RNFL thickness calculated automatically by the OCT-3 software (version 3.1) were average thickness, temporal, superior, nasal, and inferior quadrant thickness and thickness for each of the 12 30-degree segment of the disc. The parameters were the same for measurements obtained with OCT-1.
Good-quality scans had focused images, an adequate signal-to-noise ratio (>40 dB), a ring around and concentric with the optic disc, and absence of overt misalignment of the surface detection algorithm. From the three scans judged to be of acceptable quality obtained with each equipment, mean values were calculated for each studied parameter.
RNFL values with OCT-1 were compared to those from OCT-3 using paired t-test. Analysis of histograms and the Shapiro–Wilk test confirmed that the distributions satisfied the normality assumption. P-values of less than 0.05 were considered significant. Results of statistical significance were provided after Bonferroni's correction based on the number of comparisons within each analysis. Bland and Altman plots were constructed to assess agreement between OCT-1 and OCT-3 RNFL thickness measurements.16, 17 Both absolute and the percentage difference between OCT-1 and OCT-3 were evaluated. The number of disagreement measurements within 10 and 20 μm and within a certain percentage (10 and 20%) was compared between the two groups using the χ2-test. Corresponding RNFL values of patients with BA measured both with OCT-1 and OCT-3 were also compared with those of normal controls using unpaired Student's t-test.
Results
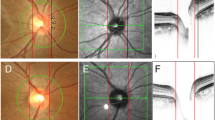
Figure 1 depicts the distribution of average RNFL thickness as well as the parameters measured by OCT-1 and OCT-3 in each quadrant of BA and normal eyes. In eyes with BA, the peripapillary RNFL (mean±SD, in μm) measured with OCT-1 was 99.81±14.00, 61.69±13.02, 101.70±12.54, and 57.36±16.52 in the superior, temporal, inferior, and nasal quadrants, respectively. The mean global RNFL was 80.42±6.94. The corresponding figures for OCT-3 were 81.22±13.34, 39.50±8.27, 86.72±15.16, and 45.05±8.03. The mean global RNFL was 63.11±6.76. Comparisons were also made in each of 12 clock hours measurements. After Bonferroni's correction (α=0.003; 17 comparisons), average measurements as well as measurements in each quadrant with OCT-3 were significantly smaller (P<0.003) than values obtained with OCT-1. Measurements in the 30-degree segments of the optic disc were significantly smaller for OCT-3 at 10, 9, 8, 2, and 1 O’ clock (Table 1).
In normal eyes, the peripapillary RNFL (mean±SD, in μm) measured by OCT-1 was 134.26±16.35, 83.50±14.57, 145.37±14.68, and 91.89±18.80 in the superior, temporal, inferior, and nasal quadrants, respectively. The mean global RNFL was 114.35±11.02. The corresponding figures for OCT-3 were 130.16±15.54, 70.83±11.29, 135.25±16.00, and 80.88±16.47. The mean global RNFL was 104.76±9.81 (Table 2). Measurements with OCT-3 were significantly smaller (P<0.003) than those obtained with OCT-1 in the global measurement as well as in the temporal quadrant. Comparisons of measurements for each of the 12 30-degree segments showed significantly smaller values for OCT-3 than for OCT-1 only at 9, 8, and 4 O’ clock (Table 2).
Bland–Altman17 plots were made depicting the agreement between OCT-1 and OCT-3 RNFL thickness measurements in eyes with BA and in normal controls. The difference (OCT-1 RNFL thickness minus OCT-3 thickness) was plotted against the mean of the two measurements for the average value as well as for measurements of each quadrant around the disc (Figure 2). There was considerable disagreement between the 90 measurements made with OCT-1 and OCT-3. In most cases, measurements were greater with OCT-1 than with OCT-3. The discrepancies between OCT-1 and OCT-3 RNFL thickness measurements were more evident in eyes with BA compared with normal eyes. The difference between the OCT-1 and OCT-3 measurements was within 20 μm in 53 (58.8%) measurements in eyes with BA and in 73 (81.1%) measurements in normal eyes. The χ2-test showed a significant difference between the two groups (P=0.001). The difference was within 10 μm in 30 (33.3%) measurements in eyes with BA and in 38 (42.2%) measurements in normal eyes. No significant difference was observed (P=0.219) in this comparison.
Bland–Altman plots of the agreement in RNFL thickness between OCT-1 and OCT-3. The difference (OCT-1 RNFL thickness minus OCT-3 RNFL thickness) was plotted against the average of the two measurements for the global measurements and for measurements in each quadrant (90 measurements). Above: eyes with band atrophy. Below: normal control eyes.
The difference in measurements of eyes with relatively thinner RNFL became more evident when the percentage difference between the two methods was plotted against the mean of the two measurements (Figure 3). The difference was within 20% of the mean in 75 (83.3%) measurements in normal eyes but only in 37 (41.1%) measurements from eyes with BA (P<0.0001, χ2-test). The percentage difference was within 10% of the mean in 38 (42.2%) of measurements in normal eyes and in only 20 (22.2%) of measurements in eyes with BA (P=0.004).
Bland–Altman plots of the agreement in RNFL thickness between OCT-1 and OCT-3. The percentage difference ((OCT-1 RNFL thickness minus OCT-3 RNFL thickness)/mean of OCT-1 and OCT-3) was plotted against the average of the two measurements for the global measurements and for measurements in each quadrant. Above: eyes with band atrophy. Below: normal control eyes.
OCT-1 and OCT-3 values were both significantly smaller (P<0.001) in eyes with BA than in normal eyes, in the average measurements as well as in all four quadrants studied.
Discussion
Several studies have demonstrated improvement in examinations performed with OCT-3 when compared to previous versions of the same equipment.15, 18, 19 One of the most significant improvements of the OCT-3 version is its shorter acquisition time, especially in the FAST version used in the present study. In the OCT-1 version, images are produced from 100 A-scans performed during 1 s.6, 20 On the other hand, when using the FAST protocol with OCT-3, images are produced from 256 A-scans performed during a four-times shorter acquisition time.15 Thus, three images are captured from which the software automatically calculates the mean. As a result inter- and intra-examiner variability is smaller and reproducibility higher in OCT-3 than in OCT-1.
The higher variability observed for OCT-1 should in theory lead us to expect values both greater and smaller than those provided by later versions; however, we observed consistently smaller values with OCT-3 than with OCT-1. As the same patients were presented by the same examiner to both OCT-1 and OCT-3 within a short period of time, we may conclude that the observed difference may be accounted for by differences in the specifications of the two devices. Our study also shows that such difference may be observed with both normal individuals and patients with optic atrophy. However, differences were much more evident in eyes with BA than in normal eyes. This finding is important since interpretation of data from eyes with RNFL loss from glaucoma or other condition causing loss of RNFL fibres may become strongly biased in sequential examinations if results from different devices are treated as equivalent.
Bourne et al21 recently evaluated the comparability of RNFL thickness measurements obtained by two versions of OCT (Stratus OCT and OCT 2000). These authors analysed the results obtained by both devices obtained on the same day in 104 eyes of 104 individuals (28 with open-angle glaucoma, 40 suspected of having glaucoma, and 36 healthy subjects) and reported thinner RNFL measurements with Stratus OCT compared to OCT 2000. Application of a correction factor to OCT 2000 measurements predicted Stratus OCT RNFL thickness within 10 μm of the observed measurement in 75% of the eyes, although they observed considerable variability that exceeds the limits of resolution afforded by the instruments. We therefore suggested that comparisons between instruments using these approximations should be interpreted with caution.21 Our results agree with those from Bourne et al in that RNFL thickness measurements obtained with the Stratus OCT were significantly thinner than those measured by older versions of this technology. However, contrary to Bourne et al, we found that the discrepancies between the two devices tended to become worse in patients with thinner RNFL. It should be noted that our study included eyes with more severe optic atrophy and thinner RNFL measurements than those studied by Bourne et al,21 which may have contributed to reveal more discrepancies between the two OCT devices in the presence of severe RNFL loss. We are unaware of previous reports comparing measurements between different versions of OCT in eyes with BA of the optic nerve. Such eyes represent an important model when investigating RNFL measuring equipments, as the pattern of RNFL loss is markedly different from the one occurring in glaucoma.
We could not find an exact explanation for the consistent difference observed between the measurements from the two versions of the technology. This difference could be related to modifications in the hardware as well as in the software of the instrument. Differences in the axial and longitudinal resolution as well as in the algorithm for detection of the RNFL borders between the two versions of the instrument may explain in part our findings. High-density scan measurements of the RNFL tend to result in lower values of thickness than standard-density scans, perhaps owing to the higher accuracy of detection of the retinal posterior border of the RNFL with the former.19 Our data analyses show that the differences between OCT-1 and OCT-3 were more evident in areas with lower values of RNFL thickness. In normal eyes, differences were significant for average values as well as for thickness in the temporal quadrants and in some of the 30-degree segments located temporally (9 and 8 O’ clock) and nasally (4 O’ clock). The RNFL is known to be thinner in these areas than in the superior and inferior areas of the optic disc. On the other hand, in eyes with BA OCT-1 and OCT-3 measurements differed in every quadrant and in most 30-degree segments. Bland and Altman17 plot analyses of BA and normal controls examinations lend support to this conclusion because measurement discrepancies between the two OCT devices were more evident for the smaller measurements (Figures 2 and 3).
As there is no external validation for measurements obtained with either version of the equipment it is not possible to be certain about which one of the devices is more accurate. However, if we assume that the newest generation of the equipment (OCT-3) is the more accurate one, one possible interpretation would be that the OCT-1 overestimates the thickness in areas with thin RNFL. In these areas, the OCT-3 would be able to provide better estimates of thickness because of its superior performance in correctly identifying the borders of the RNFL. These findings are in agreement with those of Ishikawa et al22 who observed significantly lower values of RNFL thickness using a refined and more accurate algorithm for detection of the inner and outer borders of the RNFL, compared with the commercially available OCT-1 software (version A5). These authors also observed that the commercially available algorithm, which is similar to the one used in the present study, lacks the flexibility required to adapt to various conditions of reflectivity. This is particularly important in glaucomatous eyes owing to their thin and uneven RNFL reflectivity.22 Thus, it would seem that the more recently developed software (version 3.1) used by the OCT-3 equipment improves detection of inner and outer borders of the RNFL, yielding smaller values particularly for the thinner areas in both normal and BA-affected eyes, but mainly in the latter.
In conclusion, our study shows RNFL measurements obtained with OCT-3 to be significantly smaller than those obtained with OCT-1 in almost all study parameters in eyes with BA and in the nasal and temporal disc areas of normal eyes. Although both OCT devices were able to differentiate eyes with BA from normal eyes, the values of RNFL thickness obtained by the two instruments were significantly different. Researchers and clinicians should be aware of this fact when comparing older RNFL measurements with values obtained with later versions of the same equipment.
References
Chauhan DS, Marshall J . The interpretation of optical coherence tomography images of the retina. Invest Ophthalmol Vis Sci 1999; 40: 2332–2342.
Huang Y, Cideciyan AV, Papastergiou GI . Relation of optical coherence tomography to microanatomy in normal and rd chickens. Invest Ophthalmol Vis Sci 1998; 39: 2405–2416.
Toh CA, Narayan DG, Boppart SA, Hee MR, Fujimoto JG, Birngruber R et al. A comparison of retinal morphology viewed by light microscopy. Arch Ophthalmol 1997; 115: 1425–1428.
Jones AL, Sheen NJL, North RV, Morgan JE . The Humphrey optical coherence tomography scanner: quantitative analysis and reproducibility study of the normal human retinal nerve fibre layer. Br J Ophthalmol 2001; 85: 673–677.
Schuman JS, Hee MR, Puliafito CA, Wong C, Pedut-Kloizman T, Lin CP et al. Quantification of nerve fibre layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol 1995; 113: 586–596.
Hoh ST, Greenfield DS, Mistlberger A, Liebmann JM, Ishikawa H, Ritch R . Optical coherence tomography and scanning laser polarimetry in normal, ocular hypertensive and glaucomatous eyes. Am J Ophthalmol 2000; 129: 129–135.
Parisi V, Manni G, Centofanti M, Gandolfi SA, Olzi D, Bucci MG . Correlation between optical coherence tomography, pattern electroretinogram, and visual evoked potentials in open-angle glaucoma patients. Ophthalmology 2001; 108: 905–912.
Furuichi M, Kashiwagi K, Furuichi Y, Tsukahara S . Comparison of the effectiveness of scanning laser polarimetry and optical coherence tomography for estimating optic nerve fibre layer thickness in patients with glaucoma. Ophthalmologica 2002; 216: 168–174.
Greaney MJ, Hoffman DC, Garway-Heath DF, Nakla M, Coleman AL, Caprioli J . Comparison of optic nerve imaging methods to distinguish normal eyes from those with glaucoma. Invest Ophthalmol Vis Sci 2002; 43: 140–145.
Monteiro MLR, Leal BC, Rosa AAM . Optical coherence tomography analysis of axonal loss in band atrophy of the optic nerve. Br J Ophthalmol 2004; 88: 896–899.
Kanamori A, Nakamura M, Matsui N, Nagai A, Nakanishi Y, Kusubara S et al. Optical coherence tomography detects characteristic retinal nerve fiber layer thickness corresponding to band atrophy of the optic discs. Ophthalmology 2004; 111: 2278–2283.
Blumenthal EZ, Williams JM, Weinreb RN, Girkin CA, Berry CC, Zangwill LM . Reproducibility of nerve fiber layer thickness measurements by use of optical coherence tomography. Ophthalmology 2000; 107: 2278–2282.
Jones AL, Sheen NJL, North RV, Morgan JE . The Humphrey optical coherence tomography scanner: quantitative analysis and reproducibility study of the normal human retinal nerve fibre layer. Br J Ophthalmol 2001; 85: 673–677.
Villain MA, Greenfield DS . Peripapillary nerve fiber layer thickness measurement reproducibility using optical coherence tomography. Ophthalmic Surg Lasers Imaging 2003; 34: 33–37.
Jaffe GJ, Caprioli J . Optical coherence tomography to detect and manage retinal disease and glaucoma. Am J Ophthalmol 2004; 137: 156–169.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurements. Lancet 1986; 1: 307–310.
Bland JM, Altman DG . Measuring agreement in method of comparison studies. Stat Methods Med Res 1999; 8: 135–160.
Schuman JS, Pedut-Kloizman T, Hertzmark E, Hee MR, Wilkins JR, Coker JG et al. Reproducibility of nerve fiber layer thickness measurements using optical coherence tomography. Ophthalmology 1996; 103: 1889–1898.
Paunescu LA, Schuman JS, Price LL, Stark PC, Beaton S, Ishikawas H et al. Reproducibility of nerve fiber thickness, macular thickness, and optic nerve head measurements using Stratus OCT. Invest Ophthalmol Vis Sci 2004; 45: 1716–1724.
Kanamori A, Nakamura M, Escano MFT, Seya R, Maeda H, Negi A . Evaluation of the glaucomatous damage on retinal nerve fiber layer thickness measured by optical coherence tomography. Am J Ophthalmol 2003; 135: 513–520.
Bourne RAR, Medeiros FA, Bowd C, Jahanbakhsh D, Zangwill LM, Weinreb RN . Comparability of retinal nerve fiber layer thickness measurements of optical coherence tomography instruments. Invest Ophthalmol Vis Sci 2005; 46: 1280–1285.
Ishikawa H, Piette S, Liebmann JM, Ritch R . Detecting the inner and outer borders of the retinal nerve fiber layer using optical coherence tomography. Graefe's Arch Clin Exp Ophthalmol 2002; 240: 362–371.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Monteiro, M., Leal, B., Moura, F. et al. Comparison of retinal nerve fibre layer measurements using optical coherence tomography versions 1 and 3 in eyes with band atrophy of the optic nerve and normal controls. Eye 21, 16–22 (2007). https://doi.org/10.1038/sj.eye.6702182
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702182
Keywords
This article is cited by
-
Macular thickness measurements with frequency domain-OCT for quantification of axonal loss in chronic papilledema from pseudotumor cerebri syndrome
Eye (2014)
-
Correlation between multifocal pattern electroretinography and Fourier-domain OCT in eyes with temporal hemianopia from chiasmal compression
Graefe's Archive for Clinical and Experimental Ophthalmology (2013)
-
Correlation between macular and retinal nerve fibre layer Fourier-domain OCT measurements and visual field loss in chiasmal compression
Eye (2010)
-
Comparison of the GDx VCC scanning laser polarimeter and the stratus optical coherence tomograph in the detection of band atrophy of the optic nerve
Eye (2008)
-
Pattern electroretinograms for the detection of neural loss in patients with permanent temporal visual field defect from chiasmal compression
Documenta Ophthalmologica (2008)