Abstract
Breast cancer is a heterogeneous disease, having multiple subtypes with different malignant phenotypes. The triple-negative breast cancer, or basal breast cancer, is highly aggressive, metastatic and difficult to treat. Previously, we identified that key molecules (IL6, CSF2, CCL5, VEGFA and VEGFC) secreted by tumor cells and stromal cells in basal breast cancer can promote metastasis. It remains to assess whether these molecules function similarly in other subtypes of breast cancer. Here, we characterize the relative gene expression of the five secreted molecules and their associated receptors (GP130, GMRA, GMRB, CCR5, VEGFR2, NRP1, VEGFR3, NRP2) in the basal, HER2 (human epidermal growth factor receptor 2) positive, luminal A and luminal B subtypes using high throughput data from tumor samples in The Cancer Genome Atlas (TCGA) and Molecular Taxonomy of Breast Cancer International Consortium (METABRIC). IL6 and CCL5 gene expression are basal breast cancer specific, whereas high gene expression of GP130 was observed in luminal A/B. VEGFA/C and CSF2 mRNA are overexpressed in HER2 positive breast cancer, with VEGFA and CSF2 also overexpressed in basal breast cancer. Further study of the specific protein function of these factors within their associated cancer subtypes may yield personalized biomarkers and treatment modalities.
Similar content being viewed by others
Introduction
Breast cancer is the most frequently diagnosed cancer among women in the United States1. Primary breast tumors are divided in four main molecular subtypes: Basal (also known as, triple negative), HER2 (human epidermal growth factor receptor 2) positive, Luminal A and Luminal B. Each of these subtypes has characteristic traits and expected patient outcome. For example, basal breast cancer is the most aggressive and metastatic subtype. Basal breast tumors do not express typical breast cancer cell receptors, such as the estrogen receptor (ER), the progesterone receptor (PR) and does not overexpress the human epidermal growth factor receptor 2 (HER2) that are activated in the other subtypes2. Thus, current hormonal therapies and HER2 inhibition cannot be used to treat basal breast cancer. Moreover, therapeutic resistance is common when treating tumors from other subtypes with hormonal therapies3. Therefore, new therapeutics that target additional molecular factors in breast tumors are needed. Optimal therapeutics would target the factors that promote tumor growth and metastasis resulting from interactions between cancer cells, stromal cells and extracellular matrix.
Secreted factors from each of the diverse cells in a tumor regulate inter-cellular signaling between tumor cells and the microenvironment to promote breast cancer growth and metastasis4. Specifically, the secreted factors cytokines, chemokines and growth factors contribute to distinct modes of metastasis and subsequent mortality5. Cytokines represent soluble proteins secreted by mammalian cells that are important in cell signaling. Among them, cytokines related to inflammatory signals are involved in many human diseases. For example, in cancer, inflammation induces tumor growth, tumor drug resistance and metastasis6. Chemokines have been studied in immunology and are known to serve as immune cell-recruiting and cell-trafficking factors7. Though chemokines are a subset of cytokines, they are categorized as distinct secreted factors for this study, as they can play a role in tumor cell motility and recruitment, which are critical for metastatic dissemination. Growth factors are essential secreted factors for cancer cell proliferation, maintenance, migration and adhesion8. Angiogenic and lymphangiogenic growth factors can regulate angiogenesis and lymphangiogenesis in both primary tumors and pre-metastatic niches9,10.
Because of their critical role activating the signaling processes responsible for tumor maintance and progression, tumor secreted factors (“tumor secretome”) can serve as targets to inhibit the primary tumor growth11. The specific secreted factor in an individual tumor would provide the most promising therapeutic target in that individual’s disease. Therapeutics that thus target the secretome have the greatest potential for translation to the clinic when the factor they target are common to multiple tumors from each molecular subtype.
We previously reported that the secreted factors IL6, CSF2, CCL5, VEGFA and VEGFC are pivotal orchestrators of basal breast cancer growth and metastasis4,12. Specifically, this previous study reported that basal breast cancer cells secrete interleukin 6 (IL6), a cytokine, which conditions (educates, reprograms) lymphatic endothelial cells (LEC) within pre-metastatic organs and primary tumors to secrete the chemokine CC-chemokine ligand 5 (CCL5) and the growth factor, vascular endothelial growth factor A (VEGFA)4. This group of secreted factors including a cytokine, a chemokine and a growth factor make a self-reinforcing paracrine loop to promote basal breast cancer metastasis. LEC-derived CCL5 recruits CCR5-positive cancer cells into the lymphatic vessels and triggers tumor dissemination. LEC-derived VEGFA interacts with blood endothelial cells (BEC) of the vasculature enhancing vascular permeability in the lungs and promoting angiogenesis in the lymph nodes. These are important steps for tumor cell extravasation and colonization. VEGFC is a lymphangiogenic growth factor, secreted by cancer cells and stromal cells to promote lymphatic vessel growth in primary tumors13. We also demonstrated a crosstalk between basal breast cancer cells and BEC/LEC that was important for primary tumor growth12. We showed that the secretomes of the BEC and LEC are perturbed in distinct ways, influencing primary tumor growth, pericyte infiltration and angiogenesis in different ways12.
In addition to having a pivotal role in basal breast cancer growth and metastasis, the secreted factors implicated in our previous study (IL6, CSF2, CCL5, VEGFA and VEGFC) may also serve critical roles in other subtypes of breast cancers. In this case, inhibitors of these factors and the pathways they regulate could be used to treat a wider array of breast cancers. High throughput genomic data can indicate the molecular profile of these factors to infer such candidate targets from the secretome. Therefore, in this study we identify the relative gene expression of IL6, CSF2, CCL5, VEGFA and VEGFC and their receptors (GP130, GMRA, GMRB, CCR5, VEGFR2, NRP1, VEGFR3 and NRP2, Fig. 1), in multiple breast cancer subtypes (Basal, HER2+, Luminal A and Luminal B) using high-throughput genomic data of primary tumors from the Cancer Genome Atlas (TCGA)14 and Molecular Taxonomy of Breast Cancer International Consortium METABRIC15. The goals of this study are: (a) to understand how these key pro-metastatic factor genes are expressed in breast cancer subtypes, (b) to examine how their associated receptor genes are expressed in the subtypes and (c) to evaluate whether these gene expression profiles can predict the survival rates within each breast cancer subtype.
Results
Selection of secreted factors associated with metastasis
Figure 1 shows the ligand and receptor interactions between the factors we previously associated with metastasis4 and have selected for analysis in this current study (listed in Table 1). Specifically, this figure summarizes the relationship between these factors and adjacent blood endothelial cells (BEC) and lymphatic endothelial cells (LEC) from our previous study. Primary tumor samples used for genomic profiling contain a mixture of tumor cells and cells from the microenvironment, including adjacent BEC and LEC. We test whether the putative regulatory relationships between ligands and their associated receptor(s) are represented in mRNA expression of such primary tumors by correlating mRNA expression of each ligand with its associated receptor(s). Correlation analyses are run on large cohorts of gene expression data from 638 primary tumors in TCGA (Table 2) and from 897 primary tumors in METABRIC (Table 2), with sample characteristics in Supplemental Tables 1 and 2, respectively.
In TCGA, CSF2, CCL5 and VEGFC are all significantly correlated to their target receptors (GMRA and GMRB; CCR5; and VEGFR3 and NRP2, respectively, Table 2). VEGFA is significantly correlated to only one of its receptors (VEGFR2), but not to the other target receptor NRP1. IL6 is significantly anti-correlated with its target receptor (GP130). The significant anti-correlation between IL6 and GP130 and correlation between VEGFC and NRP2 and CSF2 and targets GMRA and GMRB are all confirmed in gene expression data from METABRIC (Table 2). However, the correlation between VEGFC and target receptor VEGFR3 fails to meet statistical significance. We are also unable to confirm associations with CCL5 with CCR5 or VEGFA with VEGFR2 because the array used in METABRIC does not contain probes that measure gene expression of CCR5 or VEGFA.
IL6 is overexpressed in basal breast cancer while its receptor GP130 is overexpressed in luminal breast cancer
We compared expression of the ligand IL6 and its target receptor GP130 in each of the breast cancer subtypes. IL6 is significantly overexpressed in the basal subtype relative to other subtypes in both TCGA (p-value of 5 × 10−8) and METABRIC (p-value of 1 × 10−9) data (Fig. 2a,b, respectively). On the other hand, the target receptor GP130 is significantly overexpressed in both luminal subtypes (Fig. 2c for TCGA and 2d for METABRIC with corresponding one-sided p-values below 2 × 10−16 in both datasets). Survival analyses were run for these genes using only METABRIC, due to the relatively long patient follow-up times in that dataset. We observed a trend towards longer survival times based upon GP130 (Supplemental Fig. 3) expression in the luminal A subtype (p-value of 0.06) not observed in the other subtypes; no significant trend was observed for IL6 (Supplemental Fig. 4).
Overexpression of CSF2 target receptors GMRA and GMRB are associated with survival in basal and HER2+ breast cancer
In TCGA, CSF2 is significantly overexpressed in basal and HER2+ breast cancer relative to luminal subtypes (Fig. 3a, p-values of 1 × 10−8 and 0.03, respectively). This discrepancy in p-values is consistent with a higher log fold change in basal relative to luminal breast cancer (0.7) than HER2+ relative to luminal breast cancer (0.3). A similar trend is confirmed in METABRIC (Fig. 3b), with a p-value of 1 × 10−8 with log fold change of 0.1 in basal breast cancer relative to luminal and p-value 0.006 with log fold change of 0.05 in HER2+ relative to luminal. However, in both datasets target receptor GMRA was only overexpressed in basal breast cancer relative to all other subtypes (Fig. 3c,d with p-values of 2 × 10−4 for TCGA and 7 × 10−10 for METABRIC). Similar association with basal breast cancer was observed for the other target receptor, GMRB (Fig. 3e,f and p-values of 1 × 10−4 for TCGA and 9 × 10−4 for METABRIC).
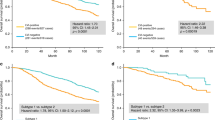
CSF2 expression was not significantly associated with survival in any subtypes (Supplemental Fig. 5). Nonetheless, higher GMRA expression significantly associated with better survival in basal breast cancer (Supplemental Fig. 6, p-value of 0.02) and GMRB expression trended towards higher survival in HER2+ breast cancer (Supplemental Figure 7, p-value of 0.08).
CCL5 overexpression is associated with basal breast cancer and with survival in HER2+ breast cancer
Similar to CSF2, chemokine CCL5 is significantly overexpressed in basal over luminal breast cancer in both TCGA (Fig. 4a, p-value of 9 × 10−8) and METABRIC (Fig. 4b, p-value below 2 × 10−16). CCL5 is also significantly overexpressed in HER2+ breast cancer relative to luminal in METABRIC (p-value of 9 × 10−9) with a similar trend that failed to reach statistical significance in TCGA (p-value of 0.09). Likewise, its target receptor CCR5 is significantly overexpressed only in basal breast cancer in TCGA (Fig. 4c, p-value of 0.02). We are unable to confirm these relationships in METABRIC because there was no associated probe for this gene on the array measuring expression in this study. Nonetheless, increased CCL5 expression was associated with better survival in HER2+ breast cancer (Supplemental Figure 8, p-value of 0.01).
VEGFA is associated with HER2+ breast cancer and its target VEGFR2 with survival in basal breast cancer
In TCGA data, VEGFA expression is highest in HER2+ breast cancer (Fig. 5a, p-value of 5 × 10−3 relative to other subtypes). It is also overexpressed in basal breast cancer relative to luminal breast cancer (p-value of 5 × 10−9). These relationships could not be confirmed in METABRIC because no probe measures VEGFA gene expression.
Although expression of the target receptor VEGFR2 was not associated with any subtype in TCGA data (Fig. 5b), it was significantly overexpressed in HER2+ breast cancer in METABRIC (Fig. 5c, p-value of 4 × 10−3). The other target receptor, NRP1, was not differentially expressed in any breast cancer subtypes in TCGA (Fig. 5d), but was overexpressed in basal breast cancer relative to other subtypes in METABRIC (Fig. 5e, p-value of 2 × 10−4). Moreover, increased VEGFR2 expression was significantly associated with better survival in basal breast cancer (Supplemental Figure 9, p-value of 0.008). No significant associations with survival were observed in any subtype for NRP1 (Supplemental Figure 10).
VEGFC is significantly overexpressed in HER2+ breast cancer
VEGFC is significantly overexpressed in HER2+ breast cancer relative to basal breast cancer in TCGA (Fig. 6a, p-value of 0.005) and in HER2 + breast cancer relative to all other subtypes in METABRIC data (Fig. 6b, p-value of 4 × 10−6). It is also overexpressed in both luminal subtypes relative to basal breast cancer in TCGA (p-value of 0.003), not confirmed in the METABRIC data. We observe significant overexpression of target receptor VEGFR3 in the luminal A subtype in TCGA (Fig. 6c, p-value of 2 × 10−3), while we observe significant overexpression of VEGFR3 in basal breast cancer in METABRIC (Fig. 6d, p-value of 9 × 10−3). NRP2, which is not significantly differentially expressed in any subtype in TCGA (Fig. 6e) but is significantly overexpressed in basal breast cancer in METABRIC (Fig. 6f, p-value of 9 × 10−8). Moreover, we do not observe any significant survival differences based upon expression of genes in this pathway (Supplemental Figures 11–13 for VEGFC, VEGFR3 and NRP2, respectively).
Discussion
In this study, we characterized gene expression of multiple secreted factors and their receptors, in all the breast cancer subtypes (Basal, Her2, Luminal A and Luminal B) by using large genomic studies (TCGA and METABRIC). The factors and receptors analyzed were IL6, CSF2, CCL5, VEGFA, VEGFC, GP130, GMRA, GMRB, CCR5, VEGFR2, NRP1, VEGFR3 and NRP2, because we found their protein expression to be critical to basal breast cancer metastasis in previous studies4,12. In this study, we found that that IL6 and CCL5 gene expression are basal breast cancer specific. High gene expression of GP130 is observed in luminal A/B. VEGFA/C and CSF2 mRNA are overexpressed both basal and HER2+ breast cancer relative to luminal subtypes.
IL6 mRNA expression is higher in basal breast cancer when compared to other subtypes of breast cancer. Basal breast cancer is considered as aggressive and metastatic and effective therapeutic treatments are very limited. IL6 protein has been studied in breast cancer16; it promotes formation of cancer stem cells17. Mesenchymal stem cell derived IL6 protein promotes breast cancer cell migration and invasion18. IL6 protein is also involved in drug resistance in breast cancer19. Studies of protein expression in basal breast tumors during lymph node metastasis in mouse models have shown that IL6 was highly expressed in lymph node positive basal breast tumors, compared to lymph node negative basal breast20. IL6 protein can activate a STAT3 (signal transducer and activator of transcription 3) pathway. Binding of IL6 protein to the GP130 receptor triggers STAT3 phosphorylation by JAK221. Recent bioinformatics study showed that STAT3-associated genes can be a prognostic marker in basal breast cancer22. Although we did not observe an association between IL6 gene expression and survival, the association of IL6 gene expression with basal breast cancer and its protein function documented in other previous studies suggest that IL6 protein expression may serve as a therapeutic and diagnostic marker for basal breast cancer growth and metastasis.
Surprisingly, we observed that GP130, a functional receptor gene for IL6 signal transduction, has lower mRNA expression in basal breast cancer, compared to luminal breast cancer. At the same time, IL6 mRNA was not highly expressed in luminal breast cancer, but enriched in basal subtype. This was unexpected because autocrine signaling of IL6-GP130-STAT3 in basal cancer cells is well-studied23,24,25. This discrepancy may be attributed to differences between gene expression and protein expression or function. Specifically, the membrane receptor GP130 mRNA must be translated into protein and then bind IL6 protein to function as a signal transducer. Thus, functional studies at the protein level are needed. Nonetheless, lower GP130 gene expression is consistent with reduced GP130 protein expression observed in a recent study by Lee et al.26. Specifically, this study showed that multiple cancer cells (e.g., lymphoma, adenocarcinoma, breast and prostate cancer) maintain activated STAT3 persistently via SIP-S1PR1 signaling, without IL6-GP130 signaling26. Sphingosine-1-phosphate receptor-1 (S1PR1), a receptor for the sphingosine-1-phosphate (S1P), is elevated in STAT3-positive tumors. S1P-S1PR1-induced STAT3 activation is persistent, in contrast to transient STAT3 activation by IL6 protein. This may suggest that basal breast tumor with lower mRNA expression of GP130 may employ other pathways, such as S1P-S1PR127. Since paracrine roles of IL6 protein are relatively less understood, our data suggest that IL6 mRNA expressed by basal tumor cells can play a role in paracrine activators for other types of breast cancer cells (e.g., luminal) or stromal cells. It has been reported that HOXB13 protein mediates tamoxifen resistance and invasiveness in luminal breast cancer by suppressing estrogen receptor (ER) and inducing IL6 protein expression28. This study demonstrates that IL6 signaling promotes aggressiveness in luminal breast cancer cells making them more basal-like. We also showed that IL6 protein expressed by basal cancer cells activated other stromal cells (e.g., lymphatic endothelial cells) to promote tumor metastasis. Paracrine roles of the IL6 protein are still less understood, warranting further studies, particularly in the luminal subtype of breast cancer and in other stromal cells in basal breast cancer.
In addition to IL6, CCL5 mRNA expression is highest in basal breast cancer, which is consistent with our experimental study showing that IL6 protein expressed by basal cancer cells conditions LEC to overexpress CCL5 protein4. That previous study also reported a significant correlation between CCL5 and IL6 gene expression in lymph node positive basal breast cancer samples from TCGA; there was no correlation for lymph node negative samples. We note that our previous study associated CCL5 protein expression in the lungs and lymph nodes with metastatic potential, but not normal LECs or cancer cells. Whereas that study analyzed protein expression in isolated cell types, the present study analyzes gene expression in primary tumors. The primary tumor samples in this study are from not purified cancer cells. As a result, this study cannot quantify the expression of CCL5 in distinct cell types. Therefore, further study is required to establish the relative expression of CCL5 in distinct cell types or metastatic sites suggested in our previous study. Nonetheless, the primary samples contain a mixture of cells so that the gene expression profiling may also characterize expression from LECs that are located in the tumor and express CCL5. We therefore hypothesize that IL6 and CCL5 gene expression within basal cancer tumor samples may determine their metastatic potential.
In this study higher CCL5 gene expression is associated with better prognosis in HER2+ breast cancer samples, but not basal breast cancer. The survival data are in contrast to association of CCL5 protein expression with metastatic potential in basal breast cancer. Nonetheless, the role of CCL5 in HER2+ breast cancer metastases warrants further study. For example, HER2+ breast cancer shows high rate of brain metastasis, compared to other subtypes29,30 and shows severe drug resistance31. Our previous study found that both of these phenotypes are consistent with CCL5 overexpression. Moreover, recently, a STAT3-CCL5 loop was studied in drug resistance in luminal cancer19 and distal metastasis in basal breast cancer4. As was the case for GP130, differences may be attributed to discrepancies between measurements of mRNA expression and protein function. Discrepancy between CCL5 gene expression and survival in HER2+ breast cancer may also arise from confounding clinical factors in the survival analysis that are independent of either therapeutic resistance or metastatic site. Associations of CCL5 expression with time to metastasis or metastatic site may be more consistent with the metastatic potential established in previous studies. However, adequate clinical data for these analyses are not available for either METABRIC or TCGA. Future prospective studies are required to establish the link between CCL5 expression, metastatic potential and survival in breast cancer subtypes. The CCL5 protein may alternatively play a different role in HER2+ breast cancer and must be studied in tumor-drug resistance.
VEGFA and VEGFC are angiogenic and lymphangiogenic growth factors, respectively. We showed that mRNA expression for these growth factors is highest in HER2+ breast cancer compared to other subtypes and that VEGFR2 mRNA expression predicted survival in HER2 patients. It has been shown that HER2 and angiogenesis signaling pathways exhibit molecular crosstalk32. In that study, higher microvascular density (enhanced angiogenesis) in human breast tumor samples predicted higher co-expression of HER2 and ER33. Angiogenesis impairment in Id-deficient mice completely suppressed HER2/neu-dependent breast tumors34, suggesting a role of angiogenic and lymphangiogenic growth factors in supporting tumor growth and hematogenous metastasis. Nonetheless, higher mRNA expression is associated with better prognosis in HER2+ breast cancer, similar to inconsistences between the metastatic potential and survival of HER2+ breast cancer for CCL5. NRP1 was overexpressed in basal breast cancer relative to other subtypes in METABRIC (Fig. 5e). It has been reported that expression of both VEGF and semaphorin genes are altered in basal breast cancer35. Semaphorin proteins are ligands of NRP proteins and exhibit anti-angiogenic and anti-lymphangiogenic property36. A pattern of high VEGFA expression with low expression of secreted semaphorins was associated with 60% of basal breast tumors35. Though VEGFC mRNA expression in HER2+ breast cancer is less well-understood, recent study showed that HER2/neu expression correlates with VEGFC and lymphangiogenesis in lymph node-positive breast cancer37. Molecular crosstalk between VEGFC mRNA expression and HER2 / HER2-dependent transcription factors remains to be investigated in future studies.
We also found that GMRA and GMRB, possible receptors for CSF2 (GM-CSF), to have high gene expression in basal breast cancer. Their high mRNA expression in HER2+ breast cancer was correlated with better survival. Roles of GM-CSF signaling in breast cancer are still controversial. GM-CSF is known as either an anti-tumorigenic host immune booster38,39 or anti-angiogenic factor40 or pro-metastatic factor41. These suggest that targeting CSF2 signaling must be considered carefully and needs to be further clarified with more mechanistic studies.
In summary, we analyzed expression of pro-metastatic factor genes in breast cancer subtypes and showed correlation between factor/receptor gene expression and patient survival rates using TCGA and METABRIC datasets. From the study, we found that IL6 and CCL5 are overexpressed in basal breast cancer, suggesting their potential as therapeutic targets. It remains to be determined if VEGFA and its receptor VEGFR2 and VEGFC and its receptor VEGFR3 and CSF2 and its receptor GMRA/GMRB can also serve as therapeutic targets for HER2+ breast cancer since the associations we found were modest. High levels of gene expression of IL6 receptor, GP130, in luminal A and B warrant further studies of paracrine roles of IL6 in luminal cancer. Other cell types such as tumor-associated macrophages can contribute to secretion of IL6 in tumor microenvironment; this has been observed in other tumor types42,43,44. In our previous study, we showed by immunohistochemistry that CCL5 protein expression was co-localized with LECs in the lungs in tumor-bearing mice, however, normal mice without tumors did not show CCL5 expression in LEC4. However, the primary tumor samples profiled in both TCGA and METABRIC contain a mixture tumor cells and cells in the microenvironment. Therefore, future screening studies of the protein expression of these factors on microdissected tissues must be performed to assess regulatory relationships within the different subtypes for treatment selection. Future prospective studies of associating CCL5, VEGFR2 and CSF2 expression with metastases could mitigate the confounding factors that may be contributing to contradictory associations in the survival analyses.
Methods
Primary breast cancer gene expression data in TCGA
Analyses of TCGA data14 are performed on primary breast cancer tumor samples with both RNA-sequencing data and clinical annotations. Level 3 normalized gene expression (RNA Seq V2) is obtained from cBioPortal using the CRAN CGDS-R package (version 1.1.30)45. Gene expression data is log2 transformed and subset to the genes of interest in Fig. 1. The following aliases identified from the Bioconductor package org.Hs.eg.db (version 2.14.0) are used to match the gene annotations used in the TCGA alignment and normalization pipeline according to Table 2.
Clinical data for each TCGA sample is downloaded directly from the TCGA Data Portal. ER and PR status are assessed using the consensus of clinical tests and summarized in “breast carcinoma estrogen receptor status” and “breast carcinoma progesterone receptor status”, respectively. HER2 status is obtained from IHC in the variable labeled “lab proc her2 neu immunohistochemistry receptor status.” Samples missing data for any one of these tests are excluded from analysis, leaving a total of 638 samples with RNA-sequencing data. Breast cancer samples are defined as “Basal” if all three markers are negative, “HER2+” if only HER2 is positive, “Luminal A” if either ER or PR are positive but not HER2 and “Luminal B” if HER2 is positive in addition to either ER or PR. Supplementary Table 1 summarizes the clinical attributes of each of the 638 samples by these subtypes.
Primary breast cancer gene expression data in METABRIC
Gene expression data from METABRIC15 are obtained from the public domain training data. Normal samples are excluded from analysis and subtypes are defined using the PAM50 class available in the clinical data. Supplementary Table 2 summarizes the clinical attributes of the 897 primary tumors by these subtypes. We compute survival times from the difference between diagnosis and follow-up dates. Patients are considered to have an event if they died of their disease, as indicated with the label “d-d.s” in the “last follow up status” variable.
We link METABRIC gene identifiers of the genes of interest in Fig. 1. In each case, we select probes indicated as having “Perfect” evidence in the annotation. We select the probe that with the lowest p-value for differential expression between subtypes for genes with multiple probes based upon the differential expression analysis described below, listed in Table 2.
Differential expression analysis
For both TCGA and METABRIC, one-sided t-tests are applied to each gene to compare expression of samples in each subtype to samples from all other subtypes. P-values are adjusted using the Benjamini-Hotchberg procedure to account for multiple hypothesis testing. In the case of METABRIC, differential expression and survival statistics are reported for the probe that has the lowest p-value in any subtype relative to the other subtypes for each gene. All analyses are performed in R, version 3.1.1.
Survival analysis
Due to the relatively limited follow-up time in TCGA, survival analyses are performed only for METABRIC data. The function “survdiff” in the CRAN package survival (2.37.7) applies the G-rho family of tests to compare survival curves for samples with high expression to samples with low expression to each gene in Fig. 1 that is also measured in METABRIC. We distinguish samples as having high or low expression of a gene relative to the distribution of expression values in the subtype that has lowest average expression of that gene. Specifically, a sample is defined as having high expression of a gene if its expression is at least one standard deviation above its mean expression in the subtype with lowest average expression. We do not perform analysis on combinations of genes and subtypes that have fewer than 10 samples with high or low expression.
Additional Information
How to cite this article: Fertig, E. J. et al. Analysis of gene expression of secreted factors associated with breast cancer metastases in breast cancer subtypes. Sci. Rep. 5, 12133; doi: 10.1038/srep12133 (2015).
References
DeSantis, C., Ma, J., Bryan, L. & Jemal, A. Breast cancer statistics, 2013. CA Cancer J Clin 64, 52–62 (2014).
Lehmann, B. D. et al. Identification of human triple-negative breast cancer subtypes and preclinical models for selection of targeted therapies. J Clin Invest 121, 2750–2767 (2011).
Eroles, P., Bosch, A., Bermejo, B. & Lluch, A. Mechanisms of resistance to hormonal treatment in breast cancer. Clin Transl Oncol 12, 246–252 (2010).
Lee, E. et al. Breast cancer cells condition lymphatic endothelial cells within pre-metastatic niches to promote metastasis. Nat Commun 5, 4715 (2014).
Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–674 (2011).
Elinav, E. et al. Inflammation-induced cancer: crosstalk between tumours, immune cells and microorganisms. Nat Rev Cancer 13, 759–771 (2013).
Rot, A. & von Andrian, U. H. Chemokines in innate and adaptive host defense: basic chemokinese grammar for immune cells. Annu Rev Immunol 22, 891–928 (2004).
Athale, C. A. & Deisboeck, T. S. The effects of EGF-receptor density on multiscale tumor growth patterns. J Theor Biol 238, 771–779 (2006).
Li, T., Yang, J., Zhou, Q. & He, Y. Molecular regulation of lymphangiogenesis in development and tumor microenvironment. Cancer Microenviron 5, 249–260 (2012).
Cao, Y. et al. Forty-year journey of angiogenesis translational research. Sci Transl Med 3, 114rv113 (2011).
Chen, S. T. et al. Breast tumor microenvironment: proteomics highlights the treatments targeting secretome. J Proteome Res 7, 1379–1387 (2008).
Lee, E., Pandey, N. B. & Popel, A. S. Lymphatic endothelial cells support tumor growth in breast cancer. Sci Rep 4, 5853 (2014).
Stacker, S. A. et al. Lymphangiogenesis and lymphatic vessel remodelling in cancer. Nat Rev Cancer 14, 159–172 (2014).
Cancer Genome Atlas Network, Comprehensive molecular portraits of human breast tumours. Nature 490, 61–70 (2012).
Curtis, C. et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature 486, 346–352 (2012).
Dethlefsen, C., Hojfeldt, G. & Hojman, P. The role of intratumoral and systemic IL-6 in breast cancer. Breast Cancer Res Treat 138, 657–664 (2013).
Iliopoulos, D., Hirsch, H. A., Wang, G. & Struhl, K. Inducible formation of breast cancer stem cells and their dynamic equilibrium with non-stem cancer cells via IL6 secretion. Proc Natl Acad Sci U S A 108, 1397–1402 (2011).
De Luca, A., Lamura, L., Gallo, M., Maffia, V. & Normanno, N. Mesenchymal stem cell-derived interleukin-6 and vascular endothelial growth factor promote breast cancer cell migration. J Cell Biochem 113, 3363–3370 (2012).
Yi, E. H. et al. STAT3-RANTES autocrine signaling is essential for tamoxifen resistance in human breast cancer cells. Mol Cancer Res 11, 31–42 (2013).
Roberti, M. P. et al. Protein expression changes during human triple negative breast cancer cell line progression to lymph node metastasis in a xenografted model in nude mice. Cancer Biol Ther 13, 1123–1140 (2012).
Wang, S. W. & Sun, Y. M. The IL-6/JAK/STAT3 pathway: potential therapeutic strategies in treating colorectal cancer (Review). Int J Oncol 44, 1032–1040 (2014).
Tell, R. W. & Horvath, C. M. Bioinformatic analysis reveals a pattern of STAT3-associated gene expression specific to basal-like breast cancers in human tumors. Proc Natl Acad Sci U S A 111, 12787–12792 (2014).
Ara, T. et al. Critical Role of STAT3 in IL-6-Mediated Drug Resistance in Human Neuroblastoma. Cancer Res 73, 3852–3864 (2013).
Ashizawa, T. et al. Clinical significance of interleukin-6 (IL-6) in the spread of gastric cancer: role of IL-6 as a prognostic factor. Gastric Cancer 8, 124–131 (2005).
Xiong, H. et al. Roles of STAT3 and ZEB1 proteins in E-cadherin down-regulation and human colorectal cancer epithelial-mesenchymal transition. J Biol Chem 287, 5819–5832 (2012).
Lee, H. et al. STAT3-induced S1PR1 expression is crucial for persistent STAT3 activation in tumors. Nat Med 16, 1421–1428 (2010).
Taga, T. IL6 signalling through IL6 receptor and receptor-associated signal transducer, gp130. Res Immunol 143, 737–739 (1992).
Shah, N. et al. HOXB13 mediates tamoxifen resistance and invasiveness in human breast cancer by suppressing ERalpha and inducing IL-6 expression. Cancer Res 73, 5449–5458 (2013).
Hicks, D. G. et al. Breast cancers with brain metastases are more likely to be estrogen receptor negative, express the basal cytokeratin CK5/6 and overexpress HER2 or EGFR. Am J Surg Pathol 30, 1097–1104 (2006).
Azim, H. A. & Azim, H. A., Jr. Systemic treatment of brain metastases in HER2-positive breast cancer: current status and future directions. Future Oncol 8, 135–144 (2012).
Campone, M., Frenel, J. S., Andre, F., Bachelot, T. & Juin, P. [Tumor resistance to HER2 inhibitors: the drug sedimentation concept]. Bull Cancer 99, 665–672 (2012).
Alameddine, R. S., Otrock, Z. K., Awada, A. & Shamseddine, A. Crosstalk between HER2 signaling and angiogenesis in breast cancer: molecular basis, clinical applications and challenges. Curr Opin Oncol 25, 313–324 (2013).
Vamesu, S. Angiogenesis and co-expressed of ER and c-erbB-2 (HER2/neu) protein in primary breast cancer patients: an analysis of 158 needle core biopsies. Rom J Morphol Embryol 49, 469–478 (2008).
de Candia, P. et al. Angiogenesis impairment in Id-deficient mice cooperates with an Hsp90 inhibitor to completely suppress HER2/neu-dependent breast tumors. Proc Natl Acad Sci U S A 100, 12337–12342 (2003).
Bender, R. J. & Mac Gabhann, F. Expression of VEGF and semaphorin genes define subgroups of triple negative breast cancer. PLoS One 8, e61788 (2013).
Sakurai, A., Doci, C. L. & Gutkind, J. S. Semaphorin signaling in angiogenesis, lymphangiogenesis and cancer. Cell Res 22, 23–32 (2012).
Schoppmann, S. F. et al. HER2/neu expression correlates with vascular endothelial growth factor-C and lymphangiogenesis in lymph node-positive breast cancer. Ann Oncol 21, 955–960 (2010).
Emens, L. A. GM-CSF-secreting vaccines for solid tumors. Curr Opin Investig Drugs 10, 1315–1324 (2009).
Emens, L. A. et al. A phase I vaccine safety and chemotherapy dose-finding trial of an allogeneic GM-CSF-secreting breast cancer vaccine given in a specifically timed sequence with immunomodulatory doses of cyclophosphamide and doxorubicin. Hum Gene Ther 15, 313–337 (2004).
Eubank, T. D. et al. Granulocyte macrophage colony-stimulating factor inhibits breast cancer growth and metastasis by invoking an anti-angiogenic program in tumor-educated macrophages. Cancer Res 69, 2133–2140 (2009).
Park, B. K. et al. NF-kappaB in breast cancer cells promotes osteolytic bone metastasis by inducing osteoclastogenesis via GM-CSF. Nat Med 13, 62–69 (2007).
Wan, S. et al. Tumor-associated macrophages produce interleukin 6 and signal via STAT3 to promote expansion of human hepatocellular carcinoma stem cells. Gastroenterology 147, 1393–1404 (2014).
Xu, H. et al. Tumor-associated macrophage-derived IL-6 and IL-8 enhance invasive activity of LoVo cells induced by PRL-3 in a KCNN4 channel-dependent manner. BMC Cancer 14, 330 (2014).
Sung, S. Y. et al. Loss of let-7 microRNA upregulates IL-6 in bone marrow-derived mesenchymal stem cells triggering a reactive stromal response to prostate cancer. PLoS One 8, e71637 (2013).
Gao, J. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal 6, pl1 (2013).
Acknowledgements
This work was supported by the National Institutes of Health grants R01 CA138264 (ASP) and K25CA141053 (EJF).
Author information
Authors and Affiliations
Contributions
E.J.F., E.L., N.B.P. and A.S.P. designed the study. E.J.F. performed all statistical analyses. All authors wrote and revised the manuscript.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Fertig, E., Lee, E., Pandey, N. et al. Analysis of gene expression of secreted factors associated with breast cancer metastases in breast cancer subtypes. Sci Rep 5, 12133 (2015). https://doi.org/10.1038/srep12133
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep12133
This article is cited by
-
Intratumor heterogeneity and cell secretome promote chemotherapy resistance and progression of colorectal cancer
Cell Death & Disease (2023)
-
Cancer secretome: finding out hidden messages in extracellular secretions
Clinical and Translational Oncology (2022)
-
MicroRNA-200c restoration reveals a cytokine profile to enhance M1 macrophage polarization in breast cancer
npj Breast Cancer (2021)
-
miR-29b-3p promotes progression of MDA-MB-231 triple-negative breast cancer cells through downregulating TRAF3
Biological Research (2019)
-
Locally advanced rectal cancer transcriptomic-based secretome analysis reveals novel biomarkers useful to identify patients according to neoadjuvant chemoradiotherapy response
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.