Abstract
Study design: Assessment of sodium output in spinal injury patients.
Objectives: The purpose was to examine the effects of sodium loading acutely by an infusion, long term by sodium supplements, to acutely injured spinal patients on a fixed sodium intake. This was compared with another group of acutely injured patients who were on a hospital diet of between 50 and 150 mmol of sodium daily.
Setting: The National Spinal Injuries Centre, Stoke Mandeville Hospital, Aylesbury, Bucks HP21 8AL, UK.
Methods: A total of 53 studies were carried out on 52 patients between 1962 and 1964. In all, 49 patients were studied during the first 10 days after injury as follows: a control group of 39 patients received no supplementary sodium, two received NaCl infusion, two NaCl tablets orally, and six received NaCl infusion followed by NaCl tablets orally. Four patients were studied for more than 15 days after injury (one of these had been studied in the acute stage); they received NaCl infusion and one (42d) received in addition NaCl tablets for four subsequent days.
Results: In all patients urinary sodium excretion was minimal on day 2 and increased thereafter. On days 2–6, it was significantly lower in patients with a complete transection of the cervical cord than in patients with lower lesions. In the early studies, nine patients excreted less than 40% of the administered load within 24 h. In four of these patients excretion was 10% or less. In the later studies, three of the four patients excreted at least 80% of the infused Na+ on the same day.
Conclusion: Sodium retention in the patient with cord injury is a response to trauma. The different responses seen in patients with different levels of cord transection are not due to direct changes in the innervation of the kidney but to compensation for sympathetic insufficiency, blood pressure being maintained by the secretion of aldosterone, vasopressin and other hormones. The decreased urinary output seen acutely after cord transection is not due to renal failure and the patient's condition can be made dangerously worse by attempts to create a diuresis.
Similar content being viewed by others
Introduction
Oliguria, associated with dramatic changes in fluid balance and marked pulmonary oedema, is well recognised after acute spinal cord trauma.1,2,3,4,5,6,7 Overtransfusion, with resultant pulmonary oedema, still occurs at receiving hospitals. A personal survey of all the Spinal Units in the UK in 19978 indicated that they were admitting at least one patient with a cervical cord transection every 2–3 months with pulmonary oedema caused by overtransfusion at the receiving hospital. A repeat survey in 20019 indicated that this problem, although less frequent, is still occurring. There has been no recent research on this problem.
Soni et al10 found 28 episodes of hyponatraemia in 19 patients from excessive intravenous infusion.
The study most recently published11 comprised controlled water loading and confirmed that the oliguria was due to water retention and independent of changes in blood pressure or renal function.
The present study in 1962–1964 attempted to determine Na+ status and ability to handle Na+ loads in a group of acutely injured tetraplegic and paraplegic patients. It is reported now because of the lack of any comparable study and the lack of suitable patients due to late transfer to specialised units because of reduced funding and the fear of MRSA and VRSA infection.
Patients and methods
Patients
A total of 52 patients were studied between 1962 and 1964, 49 of them during the first 10 days following injury (Table 1a, b, c). All were traumatic cases admitted early after injury to the National Spinal Injuries Centre, a secondary place of referral. The 49 patients in the main group were admitted on days 1–5 (median: day 1) and studied for 3–10 (median 7) days.
Neurological condition was determined by clinical examination. None had evidence of sustained hypertension, intrinsic or obstructive renal disease or urinary infection. No patient was on medication known to affect renal sodium handling. All patients who could take fluid by mouth were admitted to the study. None had ileus.
A facility to weigh patients was not available.
Methods
The investigation comprised control studies and sodium supplements.
Control studies
Group 1: a control group of 39 patients with a Na+ intake of 50–150 mmol/day.
Sodium supplements
Group 2: a total of 14 patients received supplementary Na+ as follows:
Early studies
A. Three received NaCl infusion only (Table 2)
B. Six received NaCl infusion followed by NaCl tablets orally (Table 2)
C. Two received NaCl tablets only orally (Table 3)
Late studies
D. Four patients, one of whom (DT) had been studied previously under (B) above, had studies commencing 15, 32, 42 and 700 days after injury. All these patients received NaCl infusion; one of them (42 d) received, in addition, NaCl tablets for four subsequent days (Table 2).
Procedure
Patients were recumbent. Their bladders were drained by intermittent catheterisation; all the urine passed was collected. On the day of injury, any urine present in the bladder was included with day 1. Blood pressure was measured daily. Venous blood was sampled when required for clinical management. Drugs were administered for chest and urinary tract infections. Diuretics, steroids and anticoagulants were not administered; this was not then routine practice.
Control studies: Group 1
If bowel sounds were present on admission, patients received 30 ml of iced water hourly for 24 h and then, starting with cups of tea, progressed to a light diet within 48 h.
If bowel sounds were absent, patients received sips of fluid until the bowel sounds returned. They were on a light diet within 48 h and were receiving a normal hospital diet of 50–150 mmol Na+ daily.
Sodium supplements: Group 2
In the high-salt period, a controlled Na+ diet, 20 mmol Na+ daily was given plus NaCl tablets, 196 mmol/day.
Diet:
The fixed Na+ diet was given during the first 10 days; the majority started on day 2 or later (Table 3).
Infusion:
NaCl infusions of 115–500 mmol/day were administered over a period of 24 h between days 1 and 4; one commenced on day 1, three on day 2, two on day 3 and three on day 4 (Table 2).
Laboratory analyses
[Na+], potassium [K+], [urea] and [creatinine] in serum and urine were determined by standard laboratory methods. In total, 38 patients had at least one serum [Na+] and [K+] determination; 24 had daily measurements.
Urinary aldosterone was determined daily in four patients by a paper chromatographic method12 (the best available at the time).
Creatinine clearance was determined on 24 h specimens. A total of 35 patients had at least one determination; 23 had serial determinations.
Differences between groups of data were tested for statistical significance by means of the Wilcoxon rank sum test.
In contrast with water loading, Na+ loading is not a standard test. Normal responses published in several studies13 are used here as a basis for comparison.
Reference ranges for Na+ and K+ excretion were taken as 130–250 and 75–100 mmol/day, respectively. Generally accepted reference ranges for serum [Na+], [K+] and for urinary urea output were used.
Illustrative case (Figure 1)
Patient DT. Patient with a C6 cord transection. Filled bar=input of Na+, empty bar=output of Na+. In the face of a large Na+ load, both by infusion and orally, she retained Na+ avidly until the study was discontinued on the 10th day. This was in contrast to her behaviour at 34 days when the Na+ input was returned within 24 h
In a car accident, DT, a fit young woman aged 21 years, felt a jolt and experienced pain in her neck and numbness all over her body. She was admitted to the NSIC some 8 h after injury with a complete cord transection at C6.
Her first catheterisation was at 16:15 h on day 1. She was transfused 308 mmol of Na+ over the next 24 h, only excreting 9.2%.
Bowel sounds were present and on day 3 she commenced a diet with less than 2 g Na+, supplemented by 4.5 g Na+ giving a total of 196 mmol of Na+.
She remained on an intake of 196 mmol Na+/day until day 10 and then began a normal hospital diet of 50–150 mmol Na+/day. On day 34, repeat infusion was undertaken and creatinine clearance was 83.8 ml/min.
In the face of the acute infusion challenge she excreted only 28.3 mmol Na+, and in the face of a regular daily oral intake of 196 mmol of Na+, she did not excrete more than 70 mmol/day until day 7 when she excreted 115 mmol. Cumulatively, she had received over 1000 mmol of NaCl before beginning to excrete it. She was thus retaining Na+ in the face of that high load. Blood pressure and renal function were normal.
On day 1 she excreted less than 10% of the Na+ infused, whereas a month later, when she was infused 308 mmol, she excreted 289 mmol and another 97 mmol the next day and behaved like a normal subject.
Results
Group 1: control studies
In the absence of Na+ loading, urinary Na+ output was minimal on day 2, increasing thereafter. It was significantly lower in patients with complete cervical cord transections than in patients with lower lesions on days 1–8 (P<0.05) (Figure 2). In patients with thoracic and lumbar lesions, it was also significantly lower in patients with associated injuries than in those with none on days 1, 3–5, (P<0.05) until day 7 (Figure 2). In only 33 of 39 acute patients were full blood pressure and serum [Na+] readings available.
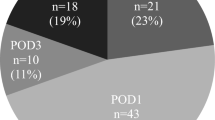
Na+ output in control patients on a hospital diet of between 50 and 150 mmol Na+. Means and standard deviations are shown. Patients with the highest Na+ excretion are those with thoracic and lumbar lesions without associated injuries. There was a marked retention of Na+ in the thoracic and lumbar patients with associated injuries. Patients with a complete cervical cord transection without associated injuries persistently showed the lowest Na+ excretion. There were no cervical patients with associated injuries
Group 2: sodium supplements
Infusions: these include early and late studies
Early studies: The nine patients studied within 4 days of injury excreted less than 40% within 24 h of infusion. In four patients, it was 10% or less (Table 2, Figure 3). Late studies: In three of the four patients studied 15 or more days after injury at least 80% of the Na+ infused was excreted on the same day (Table 2, Figure 3).
NaCl tablets in acute patients
Figure 4 shows the percentage of known Na+ intake excreted by patients replete with Na+, having received NaCl tablets for 4 or more days. From day 6 they excreted more Na+ than controls but this was still below the intake. This sodium retention was most marked in patients with complete cervical transactions.
Patients with thoracic and lumbar lesions excreted more Na+ from an earlier stage than the patients with complete cervical transactions. Urinary Na+ output in all groups was more than in control patients.
Level of lesion and associated injuries
Patients with complete cervical lesions had significantly lower Na+ excretion than those with lower lesions on days 2–5 (P<0.001; Figure 2); associated injuries led to lower excretion (P<0.05, days 3–5) and lower serum [Na+] (Table 4 and Figure 2). Complete cervical cases had much lower serum [Na+] than other patients without associated injuries (Table 4).
There were no significant differences between groups in creatinine clearance (mean 126 (SD 35.6) ml/min). It was below 80 ml/min in four patients. Na+ loading had no effect on this or on serum [K+], whose mean value was 4.73 (SD 0.74) mmol/l, with 81% of values within reference range. Urinary urea excretion increased from day 2 to day 5; associated injuries led to an increase (P<0.001) in days 4–10.
Aldosterone excretion in four control patients with no associated injuries or extra Na+ was higher on days 2–6 in cervical patients than in paraplegics (Figure 5). Blood pressures were lowest in those with incomplete cervical lesions (Table 4).
Discussion
In 1962, the National Spinal Injuries Centre was the only such unit in the South of England receiving patients with acute traumatic spinal cord transactions.
No patient admitted to the study had ileus, renal failure, raised serum [K+] or urea, or a creatinine clearance outside the accepted range.
There was no Intensive Care Unit. Patients were admitted directly to the wards of the Centre and studied. The median day of admission was day 1.
The distribution of the injuries, ages, causes and levels is comparable with other series.
No cervical patient showed a severe associated injury. This was not compatible with life at that time (between 1962 and 1964).
Accuracy of urine collection was assured. Day 1 urine collections may have included some urine produced preinjury.
The standard research procedure, then as now, to study Na+ balance, is to place patients on a low Na+ diet (<20 mmol per day) and then load them in two ways: short term by infusion of 308 mmol in 2 l and long term by adding 196 mmol Na+ per day to the diet.
The initial decreased Na+ excretion was not due to reduced Na+ intake as a result of poor appetite. In the small number of cases in whom a Ryle's tube was passed, there was no aspirate, indicating that fluids and salt were being satisfactorily absorbed. Patients with complete transections of the cervical cord were just as fit as the others; absence of associated injuries made them less likely to be suffering from surgical shock.
There have been few studies on bowel function in the stage of spinal shock. Water absorption is known to be normal11 and drug absorption in the form of anticoagulants is normal and effective, demonstrated by the fall in prothrombin time. The implication is that food and salt would also be absorbed.
Patients who received NaCl tablets orally for 4 or more days would have been replete in Na+, so there would have been no ‘lag’ in the response to loading. In the patients with complete cervical lesions, fractional Na+ excretion remained significantly less than unity at the end of the 10 days of observation. Cumulatively, Na+ retention was very large during this period. Patients with other lesions had fractional Na+ excretion close to unity by day 3, indicating that tetraplegics had an impaired ability to handle a Na+ load. Paraplegics with associated injuries showed responses that were intermediate between complete tetraplegics and paraplegics without associated injuries.
Plasma [Na+] represents the resultant of Na+ and water balances as well as changes in volumes of body fluid compartments. Following trauma, plasma [Na+] may fall if water retention exceeds Na+ retention, and conversely. The lower serum [Na+] in the complete cervical patients was therefore probably a result of water retention.
The small number of acute patients who received infusion showed avid Na+ retention and confirmed that the Na+ was not being excreted. In the first 4 days, less than 10% of the Na+ infused was excreted by four of the nine patients and the remaining five never excreted more than 38% (Table 2). Those with complete cervical transections retained more than those with incomplete cervical transections. Patients with low lesions and severe associated injuries also had avid Na+ retention.
In the late studies on Na+ infusion, excretion of more than 80% of the infused load in three of the four patients was a presumed normal response.13 The fourth patient may have been Na+ depleted before receiving the infusion since on the days of receiving NaCl tablets, Na+ excretion increased greatly. In normal control studies, when Na+ loads are given following Na+ deprivation, several days may be required for the rate of excretion to respond fully unless the patients are previously well hydrated.
This avid Na+ retention in the face of loading was also reflected in the control group of 39 acute patients on a normal hospital diet containing 50–150 mmol Na+ and without supplementary Na+. The decreased excretion persisted for the duration of the study (up to 10 days). It was most avid in the first few days and particularly marked in patients with complete cervical transections.
Possible mechanisms to explain these striking changes in the Na+ regulation are:
-
a)
A catastrophic fall in blood pressure following a cord transection, which would thus not be sufficient to perfuse the kidneys, particularly in cervical patients. There was no such fall in blood pressure immediately after cord transection in our series. Creatinine clearance was normal. In a normal subject the blood flow to the kidneys is well maintained by autoregulation of renal perfusion at levels of systolic blood pressure over 90 mmHg; in our series, the blood pressure was maintained at this level. Thus, these patients had adequate perfusion of their kidneys.
-
b)
Abnormal homoestasis due to increased hormonal secretion: limited studies on four control patients showed aldosterone excretion to be raised and, as part of the study, a marked antidiuretic effect was demonstrated, presumed due to increased secretion of vasopressin.11 These findings are not unique. Abnormal aldosterone secretion has been recorded. Rossier et al14 found raised aldosterone excretion in tetraplegic patients in the acute stage. In the later stages, abnormalities have been found in the regulation of aldosterone excretion by Claus Walker;15 Matthias et al16 found raised aldosterone levels. Aldosterone is only one of the factors involved in Na+ handling and some studies have been made on atrial natriuretic hormone.17
Renal retention of Na+ is well documented in patients following trauma or major surgery18,19 but it usually only lasts for 48 hours. In our patients, Na+ retention was most marked in those with complete cervical transections and, by contrast, lasted for up to 10 days.
There was a difference between patients with complete and incomplete cervical transections. We believe that it is not a direct, but an indirect effect upon the blood supply to the kidney that affects the Na+ handling. Following spinal cord transection, particularly in the cervical region, there is a tendency for the blood pressure to fall but, as a compensatory defence mechanism, vasopressin (antidiuretic hormone), aldosterone and atrial natriuretic peptides are secreted in an effort to increase the circulating volume and maintain blood pressure. This is supported by our previous findings11 and by the increased levels of atrial natriuretic peptides in tetraplegic patients.20
We believe that we have demonstrated that there is a problem particularly in tetraplegic patients that warrants further investigation. We hope that this study will point the way.
The therapeutic implications of these findings is that salt and water retention occurring acutely after cord transection may have a homeostatic effect on the body and lead to pulmonary oedema.5,6,7
The situation can be made worse by attempts to create a diuresis. The ensuing adult respiratory distress syndrome may necessitate the patient being placed on a ventilator until the fluid has been cleared. Vigilance must be exercised when infusing patients with saline, particularly complete tetraplegics immediately after injury, because of the danger of fluid overload.
References
Pare A . The Works of Ambroise Pare. R Cotes & W Du-gard: London: 1649, pp 435–436.
Holmes G . Spinal Injuries of Warfare. The clinical symptoms of gunshot injuries of the spine. Br Med J 1915; ii: 815–821.
Guttmann L . Surgery. In: Cope Z (ed) History of the Second World War. Her Majesty's Stationery Office; London: 1953, p 463.
Guttmann L, Frankel HL . The value of intermittent catheterisation in the early management of traumatic paraplegia and tetraplegia. Paraplegia 1966; 4, 63.86.
Wolman L . The disturbance of circulation in traumatic paraplegia in acute and late stages: a pathological study. Paraplegia 1964; 2: 213–226.
Cheshire DJE, Coates DA . Respiratory and metabolic management in acute tetraplegia. Paraplegia 1966; 4: 1–23.
Meyer GA et al. Hemodynamic responses to acute quadriplegia with or without chest trauma. J Neurosurg 1971; 34: 168–177.
Silver JR . Personal Survey, 1997.
Silver JR . Personal Survey, 2001.
Soni BN et al. A retrospective study of hyponatremia in tetraplegic–paraplegic patients with a review of the literature. Paraplegia 1994; 32: 597–607.
Silver JR, Doggart JR, Burr RG . The reduced urinary output after spinal cord injury: a review. Paraplegia 1995; 33: 721–725.
Smith I . Chromatographic Techniques. Heinemann: London: 1958, p 242.
Bevan DR . The sodium story: effects of anaesthesia and surgery on intrarenal mechanisms concerned with sodium homeostasis. Proc R Soc Med 1973; 66: 1215–1220.
Rossier AB, Favre H, Valloton MB In: Lee BY, Ostrander LE, Cochran G van B, Shaw WW (eds). Body Composition and Endocrine Profile in the Spinal Cord Injured Patient. Saunders; Philadelphia: 1991, pp 163–170.
Claus-Walker J, Spencer WA, Carter RE, Halstead LS . Electrolytes and rennin–angiotensin–aldosterone axis in traumatic quadriplegia. Arch Phys Med Rehab 1977; 58: 283–286.
Mathias CJ et al. Plasma catecholamines, plasma renin activity and plasma aldosterone in tetraplegic man, horizontal and tilted. Clin Sci Mol Med 1975; 49: 291–299.
Le Quesne LP, Cochrane JPS, Fieldman NR . Fluid and electrolyte disturbances after trauma: the role of adrenocortical and pituitary hormones. Br Med Bull 1985; 41: 212–217.
Le Quesne LP, Lewis AAG . Postoperative water and sodium retention. Lancet 1953; 1: 153–158.
Moore FD . Metabolic Care of the Surgical Patient. Saunders: Philadelphia: 1959, pp 32–35.
Sutters et al. The cardiovascular, endocrine and renal response of tetraplegic and paraplegic subjects to dietary sodium restriction. J Physiol 1992; 457: 515–523.
Acknowledgements
We thank RG Burr for his assistance in the preparation of this paper and Professor Ivor Mills, Emeritus Professor of Medicine, University of Cambridge, for his assistance throughout the study. Aldosterone determinations were kindly carried out in the Clinical Biochemistry Laboratory, Royal Victoria Hospital, Belfast, by arrangement with the late Mr DW Neill. Dr Silver would like to thank Action for the Crippled Child (Polio Research Fund) for their financial assistance with this study. We certify that all applicable institutional and governmental regulations in force between 1962 and 1964 concerning the ethical use of human volunteers were followed during the course of this research.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Silver, J., Doggart, J. Reduced sodium output following acute spinal injury. Spinal Cord 42, 191–198 (2004). https://doi.org/10.1038/sj.sc.3101578
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101578
Keywords
This article is cited by
-
Re: A study of predictors for hyponatraemia in patients with cervical spinal cord injury
Spinal Cord (2018)
-
Response to ‘Hyponatremia in spinal cord injury patients: new insight into differentiating between the dilution and depletion forms’
Spinal Cord (2015)
-
Reply ‘Hyponatremia in spinal cord injury patients: new insight into differentiating between the dilution and depletion forms’
Spinal Cord (2015)
-
Changes in renal function during acute spinal cord injury: implications for pharmacotherapy
Spinal Cord (2013)
-
Spinal cord injury sequelae alter drug pharmacokinetics: an overview
Spinal Cord (2011)