Abstract
A case of extensive heterotopic ossification involving the left hip in a 16 year old girl who sustained non traumatic spinal paralysis at T4 ASIA scale A. This case demonstrates the practical difficulties facing clinicians involved in the rehabilitation of this paraplegic patient who required intervention before full maturation of her left hip heterotopic ossification (HO). The patient was developing a rapidly progressive fixed scoliosis and severe difficulty in achieving a proper seating posture. In addition there was difficulty with the application of a suitable orthosis to try and limit the progression of scoliosis as a result of the HO. Discussants will comment on heterotopic ossification in general and the course of action in this particular case.
Similar content being viewed by others
Case presentation
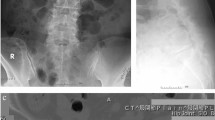
A 16-year-old girl developed sudden interscapular pain with an abrupt loss of sensation and movement in the lower extremities whilst cycling to school. She was taken by a passer-by to a local hospital where she was found to be completely paraplegic with a sensory level at T4. MRI investigation showed an epidural haematoma at T4; a decision was made to treat her conservatively. She developed a convulsive episode, which was treated with phenytoin, however, severe side effects necessitated cessation of the phenytoin therapy. No further recurrence of the convulsive episode was noted. She was transferred 6 weeks later to the local spinal rehabilitation unit and then re-transferred to our spinal treatment centre 4 months later. An important reason for the request of transfer, was irreconcilable differences between the patient and her family and the treating physician, regarding the best management approach to the massive heterotopic ossification that she developed anterior to her left hip joint. On arrival at the spinal treatment centre, she was found to be a young lady with complete T4 ASIA Grade A paraplegia. There were upper motor neurone signs with hyperreflexia and spasticity affecting the lower extremities. There were signs of early scoliosis in her thoraco-lumbar spine. The left hip was held in the extended position due to a large hard mass extending from the iliac crest down to the upper third of the thigh, causing fixation of the left hip joint in the extended position. This appeared to have worsened the scoliosis with concavity to the left when she was put in the sitting position in her wheelchair. It was impossible to flex the left hip at that level to maintain a normal sitting posture (Figures 1, 2, 3 and 4).
Radiological investigations clearly showed the massive heterotopic ossification from the left iliac fossa down to the proximal third of the left thigh. There was also a firm swelling affecting the anterior lower third of the right thigh. Radiological investigation however, showed no evidence of calcification. The patient was started on disodium etidronate with close monitoring of urinary electrolytes and blood chemistry.
The firm swelling just above the right knee resolved with return to normal texture of the soft tissue. It continued to be of normal texture throughout the patient's follow-up period. This was assumed to be due to the effect of the disodium etidronate. The etidronate however, appeared to have no influence on the heterotopic ossification of the left hip. The clinical examination and the therapist's assessment indicated that it was impossible to progress with the rehabilitation program in the presence of this massive HO. By then, the ossification had been in existence for approximately eight months.
Question to the discussants: what would be your next step?
Professor Jay V Subbarao
Before we proceed with discussion of management of this patient, we should establish goals for our management plan. I am listing some of them.
-
1)
Identify factors that increase the risk of HO formation.
-
2)
Establish maturity of HO formation in the right hip and that there are no other active sites.
-
3)
Implement preventive measures to minimise comorbidities.
-
4)
Enhance patient's rehabilitation potential to enable her to function independently in a community setting.
-
1)
Management of mature HO has limited options. Treatment with disodium etidronate (DE) or radiation of mature HO.1 However the latter is not common practice. I will consider a three-phase bone scan even at this stage to rule out any subclinical hyperemia superimposed over the mature HO. If the bone scan reveals increased activity, I will consider treatment with DE for longer duration. It appears that this patient has previously responded favourably for medication management for the lesion on the right thigh.
-
2)
Surgery for HO We reported good outcome from wedge resection of HO at the hip but the indication was primarily to enable the patient to be able to sit in the wheelchair.2 Wide resection of HO often leads to extensive bleeding, wound infection, prolonged immobility and in rare instances necessitates hip disarticulation or higher level amputations. We recommend that treatment with DE be continued post operatively until there is no clinical activity or indicated isotope uptake in the bone scan. Postoperative plain radiographs always show new bone formation but that by itself does not suggest recurrence.
-
3)
Seating System This patient's seating system should be reassessed periodically and a custom moulded insert with partially reclining back may improve her posture in the wheelchair. However, the wheelchair propulsion from this position is not very energy efficient. Proper posture maintenance is critical for prevention of pressure ulcers and spinal deformities.
-
4)
Spasticity The relationship between spasticity and HO is well documented. While direct contribution of spasticity in HO formation is not established, recurrence and severity of HO in patients with severe spasticity is reported. As such we should closely modulate the spasticity management in this young lady.
-
5)
Seizure The etiology of seizure (fit) in this otherwise healthy young individual needs to be identified. With the history of sudden onset epidural hematoma and seizures, multiple AV malformations should be ruled out. The seizures will add additional limitations in function and social reintegration for this young girl. For example driving restrictions and participation in recreational activities. If necessary she may need ongoing medication management for seizure control.
-
6)
What could have been done? There are reports of HO control with DE therapy orally and or intravenously.3 Similarly low dose radiation has been reported to control HO and avoid recurrence following surgery. We have not recommended prophylactic DE therapy for individuals with SCI for prevention of HO. We experienced good results with early intervention by way of medication management and joint mobilisation. We depend on the three-phase bone scan to monitor the progression of HO and increased vascularity. We initiate passive range of movement exercises within 2 weeks after starting therapy, while avoiding forcible stretching to minimise clinical or microscopic haemorrhage, which can lead to new HO formation. Judicious range of movement in the early stages of HO may enable the patient to retain function in the involved joint even though there is radiological evidence of massive HO formation.4 We have reported two cases with pseudoarthrosis in HO and the patient retained function of the joint involved in spite of extensive HO formation.5 I do not have experience with management of patients with radiation because it is not commonly used in our centre. I have not recommended manipulation of the involved joints in the SCI patients because they are at a high risk for pathologic fracture.4
Professor Kresimir Banovac
As a next step in the treatment of this patient I would recommend surgery. We do not have medication to treat heterotopic ossification (HO) at such late stage of development. The only treatments available today are for early stages of HO formation after SCI.
It is important to emphasise that this patient will need medical treatment after surgery to prevent regrowth of HO. Although there is no accepted protocol for postoperative prophylaxis after HO removal, on the basis of our present knowledge about this condition, the most acceptable protocol would be:
-
1)
First use NSAID's alone and
-
2)
Later add etidronate.
In the general population NSAIDs significantly reduce the incidence of HO after acetabulum fractures and total hip replacement.6 Similarly NSAIDs given early after SCI reduce the incidence of HO.7
I would recommend using indomethacin SR 75 mg in the first 6 weeks after surgery, or one of the COX-2 inhibitors for the same period of time. The effect of etidronate would be on the bone forming cells – osteoblasts that `escape' from inhibitory action of NSAIDs. The addition of etidronate would inhibit mineralisation of the bone matrix. Again, there is no protocol for postoperative use of etidronate, but one could start administration 2 weeks following surgery for a period of 3 months at a dose of 20 mg/kg/day. This approach has been effective in some of our patients.
Mr WS El Masry
This most unfortunate young lady sustained double jeopardy, the first being a non traumatic paraplegia of vascular origin over which she had no control. Secondly, massive heterotopic calcification of the iliopsoas muscle, the size and effects of which could have been minimised.
There is no easy way to manage this girl's problem, however, I will tentatively describe the rationale of the management, the main goals of her management and the sequence of investigation and treatment procedures to achieve them.
In my opinion no effort should be spared in trying to achieve comfortable seating in a wheelchair. In order to achieve this she will need to be able to flex her hips and her knees to 90 degrees. She should also be able, when lying in bed, to lie comfortably including in the supine position. In order to achieve this she should be able to have both her hips and knees extended.
From the scans available, it appears that the heterotopic calcification affects mainly the iliopsoas muscle. Although this muscle is a hip flexor, this patient's disability is caused by her inability to flex the hip. This hip extension deformity could be accounted for by one or two mechanisms. The most likely is that because the iliopsoas muscle is completely calcified (which must have happened during bedrest, probably in the supine position with extension of the hip), the calcified iliopsoas is acting as a rigid splint preventing flexion of the hip. The other possible but less likely mechanism could be excess spasticity of the hip extensors.
My first line of investigation would be to assess how much of the deformity is related to spasticity of the hip extensors and how much is due to the heterotopic calcification of the iliopsoas muscle.
In order to adequately establish which mechanism is involved, the patient will require a general anaesthetic. Manipulation under anaesthesia should also be attempted at the same time. Under the same anaesthetic the range of movement in the knee and ankle joint should also be assessed.
In the likely event manipulation of the hip does not result in adequate flexion, I would proceed to carrying out surgical debulking of the iliopsaos muscle. The patient will require biphosphonate as well as non-steroidal anti-inflammatory drugs for a least a year following the procedure. The patient ought to be aware that this is likely to be a difficult operation and that she may require blood transfusion because of the likelihood of bleeding during the surgical procedure. Post operatively an intensive rehabilitation programme will be required in order to prevent recurrence of the deformity by unopposed spasticity of the hip extensors.
In my opinion no effort should be spared in trying to achieve for her comfortable seating in a wheelchair.
Susan B Bergman
The issue of heterotopic bone formation in a growing child with a spinal cord injury is a complex one. Certainly, a fixed hip deformity will add to the risk of progression of her scoliosis. As the physical therapists have noted, it will also affect her seating position and limit her wheelchair mobility.
I am not sure if the initial course of etidronate included any non-steroidal anti-inflammatory agents along with it. If not, a place to start would be a trial of indomethacin along with the etidronate.
The next step would be to assess the metabolic activity of the heterotopic bone. This is important in assessing whether she is a candidate for excision of bone mass. If the bone is metabolically active then the risk is of actually increasing the bone after a resection. Metabolic activity of the bone mass can be assessed by checking serum alkaline phosphatase levels as well as obtaining triple phase bone scan.
If the bone is no longer metabolically active, then she may be a candidate for surgical resection of the heterotopic bone, especially because it bridges the hip joint and limits her seating and mobility. She should also be evaluated by a radiation specialist to see whether pre or post operative radiation might be helpful to shrink the mass.
Mr F Jamil
It was becoming increasingly obvious that the scoliosis was rapidly moving from flexibility in the recumbent decubitus position to non-flexibility within less than 9 months of the onset of paralysis. In addition, after discussion with the therapy team it was believed that no further therapy was going to be effective without restoring some form of flexibility to the left hip joint. It was therefore agreed by the whole team, by the patient and her relatives that we could not wait for the full maturity of her left hip HO before tackling the problem surgically.
The surgery was carried out through a boomerang incision 2 cm above and parallel to the inguinal ligament from just above the anterior superior iliac spine to 2 cm lateral to the pubic tubercle and curving down vertically for about 10 cm in the middle of the femoral triangle. The key to the surgery was exploration of the bulk of the ossified mass, which was largely in the region of the iliacus and extended down and parallel to the psoas muscle, and tapered about 4 cm below the anterior capsule of the hip joint. This was achieved by dividing the inguinal ligament and the internal oblique and transverse muscles that originate from the outer third of the inguinal ligament, and ligation of the deep circumflex iliac artery. This allowed for extra-peritoneal exposure of the whole mass by retracting away the peritoneum supero-medially. The femoral artery was isolated on vascular slings for continuous identification. All tributaries arising from the femoral artery and going in the direction of the mass were ligated. As it was impossible to access the deep feeding vessels to the bony mass, the decision was made to de-bulk it first from the inside which was achieved by excising of anterior periostium and continually removing the ossified tissue from the mass until the entire ossified mass was removed from the side wall of the ilium and the front of the left hip joint. On completion of the mass removal the posterior periostium of the mass was excised relatively easily and all the posterior feeding vessels were identified by putting some degree of traction on the edge of the periostium. There was a clear demarcation zone between the posterior periostium of the mass and the anterior hip joint capsule. The heterotopic ossification surrounding the upper third of the femur was not disturbed as, on completion of the excision of the cephalad mass it was possible to flex the left hip to 120 degrees on the operating table. The total blood loss was approximately 1200 ml. Her post-operative course was extremely smooth with no wound complications. Passive movement of the hip joint was carried out throughout the healing period. Three weeks following the surgery the patient was put in a specially moulded orthosis and was transferred into a wheelchair where she was able to bend forward, and also pick up objects from the floor.
Disodium etidronate was continued for approximately 6 months following surgery. A post-operative follow-up of more than 2 years indicated no further recurrence of the HO (Figure 5a–e). No post surgery irradiation or either pre or post surgery NSAID's were used.
Comments
Heterotopic ossification (HO) is a major complication that affects patients with spinal cord disorders and can lead to serious management problems for clinicians that are involved in the rehabilitation of such patients. Its reported incidence is between 16–53%.8,9 Significant co-existent risk factors included completeness of the paralysis, spasticity and presence of pressure sores. Age has also been reported to be a risk factor. Risk factors appear to be additive; when all risk factors co-existed the risk of HO increased to 92%.8 The incidence in paediatric patients with spinal cord paralysis in a large series of 152 patients was approximately 10%.10 In non-traumatic myelopathy the incidence of HO is approximately 6%.11
The aetiology and patho-physiology are largely unknown but one of the many theories suggests that aggressive physiotherapy and stretches leading to muscle rupture with consequent intra-muscular bleeding, along with activation of toti-potential cells that have osteoblastic activity, might be responsible. Snoecx even used the sonographic evidence of psoas muscle discontinuity with fluid collection as a predictor of subsequent development of HO of the hip in a spinal cord injured patient.12 Stover and co-workers however, studied 250 consecutive patients with early immature HO. They used a program of progressive passive range of movement and motion exercises (one side as a control in patients with bilateral hip involvement), and concluded that there was no evidence of adverse effects of exercises in increasing inflammation with subsequent ossification. Also the frequent psuedo-arthrosis that developed in the actively treated site allowed for adequate function and range of movement.13
The diagnosis, in addition to the clinical features of firmness, swelling, redness, limb swelling, (mimicking deep venous thrombosis) due to encroachment on venous drainage of the limb, plain radiography, 3-phase bone scan showing marked vascular blush and blood pool,14 and elevated 24 h prostaglandin E2 (PGE2),15 can be used as predictors of the onset of HO.
Kim and co-workers reported that the computerised quantitative radionuclide uptake ratio can be used to help in predicting progression despite radiological appearance of maturation. A reduction in the radionuclide uptake ratio of the affected compared to the non-affected side to two or less when the initial uptake ratios was 3–5 or, a reduction in the uptake ratio to three or less when the initial values were five or more, indicated stabilisation of heterotopic ossification.16
The management of heterotopic ossification includes a combination of range of motion, diphosphonate, NSAIDs, radiation therapy and surgery. While experts in the field vary in their emphasis on the combination of treatment, most of them agree that etidronate is an integral part of the medical therapy and that it plays a significant role in the prevention of HO activity before the onset of bone maturation. In one study of 63 patients with paralysis as a result of spinal cord injury, 57% of the patients developed early signs of heterotopic ossification. A regimen of IV etidronate in a dose of 300 mg per day for 3 days followed by 20 mg/kg/day orally for 6 months was used. On follow-up of 10.6±4.5 months after initiation of the therapy, 97% of the treated patients had no radiographic evidence of HO.17 Freebourn and co-workers reported a case of a 33-year-old male with T8 complete paraplegia who underwent successful surgical wedge excision of heterotopic ossification despite apparent immaturity of the HO,18 however, they used a combination of radiotherapy and NSAIDs post-operatively.
In the case discussed above a young female who developed non-traumatic spinal paralysis at T4 with upper motor neurone signs and excessive spasticity below the level of the paralysis, developed heterotopic ossification in the left hip and early HO above the right knee. She was treated with disodium etidronate. The treatment resulted in complete disappearance of the swelling above the right knee but had no influence on the HO of the left hip. She was treated by surgical excision of the entire mass with its osteoid tissue and periostium. I believe that factors that helped achieve a satisfactory outcome were:
-
1
Adequate pre-operative planning including angiography to identify major feeding vessels.
-
2
Meticulous haemostasis including ligation of the lymphatics that crossed the field of the surgery.
-
3
The use of antibiotic powder in the surgical cavity.
-
4
Vacuum closed system drainage until drainage was minimal.
-
5
Peri-operative prophylactic antibiotics and continuation of antibiotic treatment for approximately 7 days.
No other therapy, apart from etidronate, was used post-operatively.
References
Schaeffer MA, Sosner J . Heterotopic ossification: Treatment of established bone with radiation therapy Arch Phys Med Rehabil 1995 76: 284–286
Subbarao JV, Nemchausky BA, Gratzer M . Resection of heterotopic ossification and Didronel therapy-regaining wheelchair independence in the spinal cord injured patient J Am Paraplegia Soc 1987 10: 3–7
Banovac K, Gonzalez F, Wade N, Bowker JJ . Intravenous disodium etidronate therapy in spinal cord injury patients with heterotopic ossification Paraplegia 1993 31: 660–666
Subbarao JV, Garrison SJ . Heterotopic ossification: Diagnosis Management current concepts controversies J Spinal Cord Medicine 1999 22: 273–283
Subbarao JV . Pseudoarthrosis in heterotopic ossification in spinal cord injured patients Am J Phys Med Rehabil 1990 69: 88–90
Schmidt SA et al.. The use of Indomethacin to prevent the formation of heterotopic bone after total hip replacement J Bone Joint Surg 1988 70A: 834–838
Banovac K, Williams JM, Patrick LD, Haniff YM . Prevention of heterotopic ossification after spinal cord injury with Indomethacin Spinal Cord 2001 39: 370–374
Hamilton Lal S, Heinemann BB, Betts A . Risk factors for heterotopic ossification in spinal cord injury Arch Phys Med Rehabil 1989 70: 387–390
Dai L . Heterotopic ossification of the hip after spinal cord injury Chin Med J (Engl) 1998 111: 1099–1101
Garland DE et al. Spinal cord insults and heterotopic ossification in the pediatric population Clin Orthop 1989 245: 303–310
Taly AB et al. Hererotopic ossification in non-traumatic myelopathies Spinal Cord 1999 37: 47–49
Snoecx N, De-Muynck M, Van Laere M . Association between muscle truama and heterotopic ossification in spinal cord injured patients: reflections on their casual relationship and the diagnostic value of ultrasonagraphy Paraplegia 1995 33: 464–468
Stover AL, Hataway CJ, Zeiger HE . Heterotopic ossification in spinal cord injured patients Arch Phys Med Rehabil 1975 56: 199–204
Freed JH, Hahn H, Menter R, Dillon T . The use of the three phase bone scan in the early diagnosis of heterotopic ossification (HO) and in the evaluation of Didronel therapy Paraplegia 1982 20: 208–216
Schurch B, Capaul M, Vallotton MB, Rossier AB . Prostaglandin E2 measurements: their value in the early diagnosis of heterotopic ossification in spinal cord injury patients Arch Phy Med Rehabil 1997 78: 687–691
Kim SW, Wu SY, Kim RC . Computerised quantiative radionuclide assessment of heterotopic ossification in spinal cord injury patients Paraplegia 1992 30: 803–807
Banovac K, Gonzalez F . Evaluation and management of heterotopic ossification in patients with spinal cord injury Spinal Cord 1997 35: 158–162
Freebourn TM, Barber DB, Able AC . The treatment of immature heterotopic ossification in spinal cord injury with combination surgery, radiation therapy and NSAID Spinal Cord 1999 37: 50–53
Acknowledgements
Publication of this article has been supported in part by a grant from Procter & Gamble Pharmaceutical Limited. My gratitude to Marie Jones, Department of Medical Photography, Salisbury District Hospital, Salisbury for her technical support in the production of this paper.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Jamil, F., Subbarao, J., Banaovac, K. et al. Management of immature heterotopic ossification (HO) of the hip. Spinal Cord 40, 388–395 (2002). https://doi.org/10.1038/sj.sc.3101305
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101305