Abstract
Recent evidence suggest that antagonism of adenosine A2A receptors represent an alternative therapeutic approach to Parkinson's disease (PD). Coactivation of A2A and the glutamate subtype 5 metabotropic receptors (mGlu5) synergistically stimulates DARPP-32 phosphorylation and c-fos expression in the striatum. This study therefore tested the effects of a joint blockade of these receptors to alleviate the motor dysfunction in a rat model of PD. 6-Hydroxydopamine infusions in the striatum produced akinetic deficits in rats trained to release a lever after a stimulus in a reaction time (RT) task. At 2 weeks after the lesion, A2A and mGlu5 receptors selective antagonists 8-(3-chlorostyryl)caffeine (CSC) and 2-methyl-6-(phenylethynyl)-pyridine (MPEP) were administered daily for 3 weeks either as a single or joint treatment. Injections of CSC (1.25 mg/kg) and MPEP (1.5 mg/kg) separately or in combination reduced the increase of delayed responses and RTs induced by 6-OHDA lesions, while the same treatment had no effect in controls. Furthermore, coadministration of lower doses of 0.625 mg/kg CSC and 0.375 mg/kg MPEP noneffective as a single treatment promoted a full and immediate recovery of akinesia, which was found to be more efficient than the separate blockade of these receptors. These results demonstrate that the combined inactivation of A2A and mGlu5 receptor potentiate their beneficial effects supporting this pharmacological strategy as a promising anti-Parkinsonian therapy.
Similar content being viewed by others
INTRODUCTION
The dopamine (DA) precursor L-DOPA has been the most effective treatment for Parkinson's disease (PD). While improving the motor symptoms (akinesia, tremor, and rigidity) in the first years of treatment, in more than 50% of the patients the daily therapy produces severe invalidating side effects (on–off episodes, fluctuations, dyskinesia, cognitive dysfunction). Therefore, a treatment modulating the dopaminergic transmission yet targeting indirectly the dopaminergic receptors might represent a challenging therapeutic alternative. Adenosine A2A receptor (A2A) antagonists provide anti-Parkinsonian benefit in nonhuman primate model of PD (Kanda et al, 1998; Grondin et al, 1999; Morelli and Wardas, 2001) and have recently been evaluated in patients with L-DOPA-treated PD (Hauser et al, 2003; Baja-Jimenez et al, 2003). In contrast to the widespread distribution of other adenosine receptor subtypes (A1, A2B, and A3), the A2A receptor subtypes shows a quite specific localization in the basal ganglia largely restricted to the striatum (Svenningsson et al, 1999; Fredholm et al, 2001). As shown by in situ hybridization and binding studies (Martinez-Mir et al, 1991; Schiffmann et al, 1991; Svenningsson et al, 1998), the A2A receptor is coexpressed with DA D2 receptors in the striatopallidal GABAergic neurons, which contain enkephalin and originate in the so-called striatal efferent indirect pathway (Fink et al, 1992). Behavioral data support the strong A2A–D2 receptor interactions to explain the enhancement of the anti-Parkinsonian effects of DA agonists in rodent models of PD (Pinna et al, 1996; Fenu et al, 1997; Koga et al, 2000; Hauber et al, 2001).
In addition to the A2A–D2 receptors interaction, altered balance between DA- and glutamate neuronal systems may also underlie the pathophysiology of PD (Albin et al, 1989; Wichmann and DeLong, 1997). A growing number of studies in animal models of PD suggest that counteracting glutamatergic hyperactivity by pharmacological blockade of glutamate transmission in the basal ganglia represents the most recent challenge in the treatment of Parkinsonian patients (Rouse et al, 2000). Owing to their high level of expression in the basal ganglia structures: striatum, the internal pallidum and substantia nigra pars reticulata (Testa et al, 1994; Tallaksen-Greene et al, 1998), the group I metabotropic glutamate receptors play a major role in the regulation of these nuclei (Rouse et al, 2000). Indeed, recent studies in rats have emphasized the anti-Parkinsonian action of the selective mGluR antagonist of subtype 5 (mGlu5 receptor) 2-methyl-6-(phenylethylnyl)-pyridine (MPEP) in 6-OHDA-lesioned rats (Spooren et al, 2000; Breysse et al, 2002, 2003).
New findings provide evidence that coactivation of A2A and mGlu5 receptors produce synergistic effect on DARPP-32 phosphorylation, a signal transduction molecule that is selectively enriched in medium-spiny striatal neurons (Nishi et al, 2003) and potentiate c-fos striatal expression (Ferré et al, 2002). However, the functional evidence of these positive interactions on specific motor deficits such as akinesia occurring early in the course of PD remains unknown. Here we provide evidence that subthreshold doses of the highly selective A2A receptor antagonist, 8-(3-chlorostyryl)caffeine (CSC), when administered in combination to the mGlu5 receptor antagonist MPEP, alleviate motor executive deficits in an operant task in rats. Partial bilateral 6-OHDA lesions of the striatum, which have previously been found to produce long-lasting deficits in movement initiation in a reaction time (RT) task, were used as a model of the early stage of PD (Amalric et al, 1995a; Breysse et al, 2002, 2003).
MATERIALS AND METHODS
RT Task
Animals
Male Wistar rats (n=90, Charles River, Lyon, France), weighing 110–120 g at their arrival in the laboratory, were housed two per cage in a temperature and light-controlled room (0700–1900). Animals were maintained in food-deprived conditions (15–20 g laboratory chow per rat), to keep them at about 85% of the free-feeding weight. Water was available ad libitum. All procedures were conducted in accordance with the requirements of the French ‘Ministère de l’agriculture et de la pêche' Décret no. 87–848, October 19, 1987.
Behavioral procedure
Rats were conditioned in standard operant chambers (23 × 22 × 30 cm; Campden Instruments, Cambridge, UK). Each operant box was equipped with a retractable lever, a food magazine and, above the lever, a cue light (a 2.8 W bulb) corresponding to the trigger-conditioning stimulus (CS). The lever required a force of 0.8 N for switch closure. A ceiling-located red house-light was automatically switched on at the beginning of each session. Boxes were located in a wooden soundproof cabinet with a low-level noise fan. The operant chambers were controlled by a PC and data collected by an interface device (Paul Fray, Ltd). As previously detailed (Amalric et al, 1995a), rats were trained to press the lever down until the CS onset occurring randomly after four equally generated intervals (500, 750, 1000, or 1250 ms). Rats had to release the lever as fast as possible to be rewarded by a food pellet (45 mg; Phymep, Paris, France). RT, measured as the time elapsing from the CS onset to the lever release, averaged 300 ms by the end of the training phase. Daily sessions ended after 100 trials, and the performance was evaluated by recording the number of correct (rewarded) and incorrect (nonrewarded) responses. Incorrect responses are classified into ‘premature’ (a lever release before the CS onset), or ‘delayed’ when the lever is released with RTs exceeding 600 ms. In order to achieve a level of 70% of rewarded trials, rats are required to be trained for approximately 3 months of daily sessions. At the end of the training phase, rats were tested for 6 consecutive days to collect the preoperative baseline values. After a 7-day postoperative recovery period, rats were tested again for 24 sessions until postoperative day 31.
Drugs
6-OHDA (Sigma Aldrich, St Quentin Fallavier, France) was dissolved in ascorbic acid solution (0.1 mg/ml in 0.9% saline). 1,3,7-trimethyl-8-(3-chlorostyryl)caffeine (CSC), (Sigma-RBI, France) was suspended in a solution of methylcellulose (0.3%) and distilled water. MPEP hydrochloride (a generous gift of F Gasparini, Novartis, Basel, Switzerland) was dissolved in distilled water. Both compounds were injected intraperitoneally (i.p.) in a volume of 1 ml/kg.
Dopaminergic lesion
Rats were anesthetized with a solution (i.m. administered) of xylazine (15 mg/kg) and ketamine (100 mg/kg) and then positioned in a stereotaxic apparatus (David Kopf Instruments, Tujunga, CA, USA) with the incisor bar set at −3.0 mm below the interaural line. 6-OHDA (12 μg/3 μl; Sigma Aldrich, Lyon, France) or vehicle solution was bilaterally infused into the striatum (from bregma AP +0.2 mm, L ±3.5 mm, and DV −4.8 mm (Paxinos and Watson, 1986). Infusion rate of 0.3 μl/min was achieved via 30-gauge cannulae connected (by a Tygon tubing) to a 10 μl Hamilton syringe mounted on a microdrive pump (CMA/100; CMA, Stockholm, Sweden). To allow a better diffusion of the toxin from the injection site, injectors were left in place for a further 5 min.
Experimental Procedure
6-OHDA lesion
The effects of 6-OHDA lesions were evaluated on RT performance from postoperative days 8 to 13 in three groups of rats (n=16, 19, and 24, respectively). 6-OHDA-lesioned rats were then subjected to different pharmacological treatment in a chronic fashion (eg daily injected for 3 weeks from postoperative days 14 to 31).
Chronic CSC treatment
Lesioned animals were CSC injected (CSC 0.625 mg/kg, n=8 and CSC 1.25 mg/kg, n=8) and tested 20 min later in the RT task. The effects of CSC chronic treatment were further tested in two sham-operated (CSC 0.625, n=7; CSC 1.25, n=5) control groups under the same experimental conditions. Doses were selected on the basis of previous studies, showing no effect on basic motor measurement (Jacobson et al, 1993).
Chronic MPEP treatment
MPEP was injected in two groups of 6-OHDA-lesioned animals (MPEP 0.375 mg/kg, n=10 and MPEP 1.5 mg/kg, n=9) and tested immediately afterwards. The effect of the highest dose of MPEP (1.5 mg/kg) was further tested in a sham-control group (n=6), since no effects were found with the lowest dose (MPEP 0.375 mg/kg) in 6-OHDA rats. Doses of MPEP were selected on the basis of our own previous study (Breysse et al, 2002).
Chronic MPEP+CSC cotreatment
CSC and MPEP were coinjected (CSC and MPEP, respectively, 20 min later and immediately before the task) and tested in a chronic fashion as above (days 14–31 after surgery). Rats were divided into three subgroups depending on the dose of CSC and MPEP (CSC 0+MPEP 0, n=7; CSC 0.625+MPEP 0.375, n=8; CSC 1.25+MPEP 1.5, n=9). The effects of chronic CSC–MPEP coadministration were also tested in two sham-operated groups (CSC 0.625+MPEP 0.375, n=7; CSC 1.25+MPEP 1.5, n=6).
Statistical Analysis
Data were collected during pre- and postoperative period of six sessions each and during the 3 weeks chronic treatment (total of the 18 daily sessions) and analyzed on all the task-dependent variables (Statview 5.0, SAS Institute Inc., Cary, NC, USA). Number of correct, premature, and delayed responses were collapsed across days by block of 6 days each (eg weeks) and the effects of the treatment (lesion and pharmacological effects) were overall analyzed by a two-way repeated measure ANOVA, with one between-subject factor (subgroups) and two within-subject factors treatment (five blocks) and days (six sessions per block). Effects of single CSC or MPEP treatment and CSC+MPEP cotreatment were analyzed by separate repeated measures ANOVA, with one between-subject factor (6-OHDA and sham) and a two within-subject factors (blocks and days) for all the above dependent variables. One-way ANOVA followed by post hoc tests (Fisher's PLSD test) when appropriate were used for multiple pairwise comparisons within each group. Analysis on RTs were performed on selective sessions pre- (day 4)and postoperatively (on days 13, 16, 22, and 28 corresponding to periods entitled post, weeks I, II, and III). Responses with RTs shorter than 100 ms or concomitant to the cue onset were discarded since true detection of the cue was unlikely to have occurred. Furthermore, the RT limit of 600 ms taken as the criterion in control session (90% of the trials) was increased to 900 ms to take into account delayed RT occurring after 6-OHDA lesions. Furthermore, to analyze whether rats used the conditional probability of the stimulus occurrence and decreased their RTs as a function of the length of the foreperiod (delays preceding the stimulus onset), RTs were averaged by delay in all subjects and submitted to a one-way ANOVA with two within-subjects factor: the four various intervals and the pre- and postoperative sessions. To evaluate the effects of CSC (0.625 mg/kg) and MPEP (0.375 mg/kg) cotreatment on motor preparatory processes, the RTs distribution was plotted as a percentage of the total number by 50 ms bins ranging from 100 to 900 ms, in individual sessions on preoperative day 4 and postoperative days 13, 16, 22, and 28.
Histology
After completion of the behavioral testing, rats were killed by decapitation and brains were stored at −80°C until cryostat sectioning. Brains coronal 12 μm sections were collected (−20°C) at the level of the striatum using a cryostat apparatus (Leica CM3050). The extent of 6-OHDA lesions was verified by autoradiographic labeling of DA uptake sites utilizing as ligand the [3H]mazindol procedure in randomly selected subjects of each group. Binding of [3H]mazindol was measured according to the procedure described elsewhere (Javitch et al, 1985). Briefly, sections were firstly air-dried and rinsed for 5 min at 4°C in 50 mM Tris buffer with 120 mM NaCl and 5 mM KCl. Then, the sections were incubated for 40 min with 15 nM [3H]mazindol (NEN DuPont; specific activity 17 Ci/mM) in 50 mM Tris buffer containing 300 mM NaCl and 5 mM KCl added with 0.3 mM desipramine to block the noradrenaline transporter. The possible unspecific binding was determined by incubating some sections in the same solution plus 30 mM benztropine. Sections were rinsed twice for 3 min in the incubation medium without mazindol and for 10 s in distilled water and were air-dried. Finally, the sections were left in contact for 21 days to a specific 3H-sensitive film screen (Raytest, Courbevoie, France) to generate autoradiographs that were further quantified with a β imager (Fuji-Bas 5000). The lack of mazindol labeling was first determined in the dorsolateral part of the striatum (between interaural coordinates AP, 10.7–8.2 mm according to the atlas of Paxinos and Watson, 1986) in lesioned rats and compared with control animals. An overall evaluation of the DA depletion was further assessed on the whole striatum as previously described (Breysse et al, 2003).
RESULTS
After completion of the training phase, all animals reached a preoperative level averaging 70, 25, and 5% of correct, premature, and delayed responses, respectively. The overall ANOVA showed that no significant differences were found among all groups before surgery (group effect on correct, premature, and delayed responses (F11,74=0.53, F11,74=0.41, and F11,74=0.96, respectively, all NS).
Chronic Pharmacological Treatment in Control Animals
The overall ANOVA performed on the number of correct, delayed, and premature responses during pre- and postoperative periods after MPEP or CSC treatment in the five sham-operated groups revealed no significant interaction group × treatment × days (F80,520=0.9, 1.04, and 0.8 ns for correct, delayed, and premature responses, respectively), no main group effect (F4,26=1.04, 2.51, and 0.71) nor main treatment effect (F4,104=0.53, 0.68, and 0.25). The performances of the sham-operated animals remain stable for the whole duration of testing up to 4 weeks after surgery (Figure 1). Subsequent analysis performed in the CSC–control group showed that the animals did not modify their correct or incorrect (delayed and premature) responses whatever the dose of CSC tested (treatment effect, F4,40=0.22, 0.30, and 0.11, respectively, all NS) (illustrated in Figure 1a for the highest dose of CSC). Moreover, correct and incorrect responses were not affected by 1.5 mg/kg MPEP chronic treatment in sham-operated animals (Figure 1b). No significant main treatment effects were found (F4,20=0.20, 0.21, and 0.13, all NS, respectively for correct, delayed, and premature). The lowest dose of 0.375 mg/kg was therefore not further tested in this group. In addition, when injected concomitantly (ie combination of lower or higher doses of CSC and MPEP), CSC and MPEP chronic treatment did not affect the performance of sham-operated animals (main treatment effect, F4,44=0.81, 0.59, and 0.36, all NS, respectively correct, delayed, and premature responses).
Effects of chronic blockade of A2A receptors with CSC 1.25 mg/kg (a) or mGlu5 receptors with MPEP 1.5 mg/kg (b) treatment on correct (CR) and delayed (DL) responses in sham-operated animals. The vertical axes represent the mean number of responses±SEM per block of six sessions for the two variables measured. The various blocks correspond to: pre (preoperative days 6–1), post (from days 8 to 13 after surgery) and three blocks (one per week) corresponding to postoperative days 14–19, 20–25, and 26–31, respectively.
Chronic Pharmacological Treatment in 6-OHDA Groups
Histological results
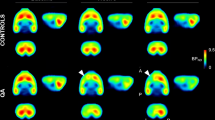
The extent of 6-OHDA-induced dopaminergic depletion is illustrated by the loss of the striatal [3H]mazindol binding in a representative subject (Figure 2a). DA denervation, measured by quantitative analysis of [3H]mazindol labeling in the depleted areas reached a level ranging from 57 to 77% (mean 66±2) in the dorsal area of the striatum as compared to sham-operated animals (p<0.01, nonpaired t-test). As previously shown (Amalric et al, 1995b; Breysse et al, 2003), the dopaminergic lesions were found to extend on the whole antero-posterior part of the striatum and were restricted to the dorsolateral area rostrally (Figure 2a). An average of 40–50% of DA denervation of the whole striata, which fits with the previously reported decrease in endogenous striatal DA contents assessed by HPLC, was found (Amalric et al, 1995b). Animals belonging to the 6-OHDA groups found to be inconsistently depleted (eg asymmetric lesion or DA depletion below 25%, n=4) were excluded from the statistical analysis.
(a) Binding of [3H]mazindol to dopamine uptake sites at the striatal level. Film autoradiograms showed the antero-posterior extent of the DA denervation in a representative 6-OHDA-lesioned animal. The lack of DA uptake binding shows the extent of the DA lesion restricted to the dorsal striatum. Values give the distance in millimeters from the interaural zero according to the atlas of Paxinos and Watson (1986). (b) Effects of chronic vehicle coinjection on correct (CR) and delayed (DL) responses after 6-OHDA lesion. The vertical axes represent the mean number of responses±SEM per block of six sessions. Pre (days 6–1), post (day 8–13 after 6-OHDA lesions) and 3 weeks of daily treatment corresponding to postoperative days 14–19, 20–25, and 26–31, respectively. *Significant difference from preoperative performance (p<0.05, PLSD Fisher's test after significant ANOVA).
Behavioral results
While surgery did not affect the postoperative performance in the sham-operated groups, the striatal 6-OHDA injections significantly altered correct responding in all lesioned groups over time (overall group × treatment × days interaction F120,960=1.24, p<0.05). A significant group × treatment × days interaction was also found on the number of delayed responses (F120,960=1.33, p<0.05) with no change in premature responding (F120,960=0.9, NS). As illustrated in Figure 2b, 6-OHDA lesions decreased the number of correct responses by significantly enhancing delayed responses (lesion effect, F1,48=78.52 and F1,48=123.46, respectively, p<0.01). The effects of the lesion were long lasting since no recovery was observed for up to 31 days postlesion in the vehicle-injected group (presurgery vs third week, all p<0.01 and postsurgery vs third week, all NS, for correct and delayed responses; Fisher's PLSD test). 6-OHDA lesions also produced a lengthening of RTs (main lesion effect F1,48=226.13, p<0.01) with no differences among lesioned groups as seen on postlesion period in Figure 6a, b (no group effect F6,48=0.26, NS). Correct RTs ranging from 308±11.43 to 328±8.8 ms in the various groups preoperatively were increased in a range of 403±15.9 to 427±11.10 ms 14 days after 6-OHDA lesions (all pre- vs postlesion RTs were significantly different, p<0.001, Fisher's PLSD test). Indeed, the typical RTs distribution (illustrated in the group cotreated with subthreshold doses of CSC and MPEP in Figure 7a) revealed that the lesions induced an important rightward shifting of the distribution curve towards higher values of RTs.
(a) Mean RT (ms)±SEM for one preoperative session (day 4; prelesion) and four postoperative sessions corresponding to the lesion effect without treatment (day 13; postlesion) and at different timing after daily treatment with CSC 0.625, 1.25 mg/kg or MPEP 0.375, 1.5 mg/kg (days 16, 22, and 28 corresponding, respectively, to first, second, and third weeks of treatment). (b) Mean RT (ms)±SEM for one preoperative session (day 4; prelesion) and four postoperative sessions corresponding to the lesion effect without treatment (day 13; postlesion) and at different timing after combined administration of CSC and MPEP at different doses (CSC 0 mg/kg+MPEP 0 mg/kg; CSC 0.625 mg/kg+MPEP 0.375 mg/kg and CSC 1.25 mg/kg+MPEP 1.5 mg/kg) as shown in (a) *,°Significant difference from preoperative and the first block of postoperative performance, respectively (p<0.05, PLSD Fisher's test after significant ANOVA).
(a) Distributions of RTs before (open bars) and after striatal 6-OHDA lesions (solid bars). RTs distribution are illustrated before treatment (upper graph) and after 1, 2, or 3 weeks of chronic daily treatment with MPEP 0.375 mg/kg and CSC 0.625 mg/kg (lower graphs). Each bar represents the RT frequency (percentage) by 50 ms bins from 100 to 900 ms. (b) RTs (ms) are averaged at each foreperiod preceding the visual cue onset before (diamond, dashed line) and after 6-OHDA lesions (upper graph) and following chronic daily treatment with MPEP 0.375 mg/kg and CSC 0.625 mg/kg (lower graphs, square, and solid lines).
A2A receptor blockade in 6-OHDA-lesioned rats
CSC treatment induced a significant main effect on correct responses (F4,72=12.59, p<0.01; Figure 3), delayed responses (F4,72=22.34, p<0.01), whereas no effect on premature responses was found (main treatment effect, F4,72=0.16, NS). Post hoc analysis further revealed that while the lowest dose of CSC (0.625 mg/kg) did not modify the 6-OHDA-induced alterations of correct (decreased) and delayed (increased) responses (Figure 3a), CSC 1.25 mg/kg significantly enhanced the number of correct responses by the second week of treatment (postsurgery vs second and third week, p<0.05, Fisher's PLSD test, Figure 3b). The mean correct score measured at the last week of treatment was not significantly different from prelesion scores (significant difference between presurgery and first and second weeks only, p<0.01, Fisher's PLSD test). A progressive decrease of delayed responses allowed a full recovery of the preoperative performances after 3 weeks of CSC 1.25 mg/kg treatment (postsurgery vs first, second, and third week, p<0.05, preoperative vs first and second week, p<0.05, but not third week, Fisher's PLSD test). Furthermore, while CSC 0.625 mg/kg did not reduce the increased RTs following 6-OHDA lesions at any time postlesion, a progressive reduction of RTs was observed after CSC 1.25 mg/kg (postsurgery vs first, second, and third week, p<0.05, Fisher's PLSD test; Figure 6a).
Effects of chronic A2A receptors with CSC 0.625 mg/kg (a) or 1.25 mg/kg (b) treatment on correct (CR) and delayed (DL) responses after 6-OHDA lesion. Vertical axes represent the mean number of responses±SEM per block of six sessions. Pre (days 6–1), post (day 8–13) and 3 weeks of daily treatment with CSC corresponding to postoperative days 14–19, 20–25, and 26–31, respectively. *,°Significant difference from preoperative and the first block of postoperative performance, respectively (p<0.05, PLSD Fisher's test after significant ANOVA).
mGlu5 receptor blockade in 6-OHDA-lesioned rats
MPEP-injected animals (0.375 and 1.5 mg/kg) showed a significant effect on correct (main treatment effect, F4,84=9.25, p<0.01) and delayed (main treatment, F4,84=23.01, p<0.01) but not premature responses (F4,84=0.56, NS, as illustrated in Figure 4a, b). Post hoc analysis further revealed that the lowest dose of MPEP did not affect the number of correct and delayed responses (presurgery vs first, second, and third week, all p<0.01, Fisher's PLSD test; Figure 4a), while MPEP 1.5 mg/kg progressively counteracted the effect of the lesion (Figure 4b). A full recovery of preoperative performances was found on correct performance at the last week of testing (post vs third week, p<0.01, Fisher's PLSD test). The mean correct score measured at the last week of treatment was not significantly different from prelesion scores (significant difference between presurgery and first and second weeks only, p<0.01, Fisher's PLSD test). MPEP 1.5 mg/kg treatment rapidly decreased delayed responses over time to reach preoperative level of performance by the second week of treatment (postsurgery vs second and third week, p<0.05, preoperative vs first week only, p<0.01, Fisher's PLSD test). In addition, as illustrated in Figure 6a, MPEP 1.5 mg/kg but not 0.375 mg/kg significantly decreased mean RTs during the 3-week treatment (postsurgery vs first, second, and third week, p<0.05, Fisher's PLSD test).
Effects of chronic mGlu5 receptors blockade with MPEP 0.375 mg/kg (a) or 1.5 mg/kg (b) on correct (CR) and delayed (DL) responses after 6-OHDA lesion. Vertical axes represent the mean number of responses±SEM per block of six sessions. Pre (days 6–1), post (day 8–13) and 3 weeks of daily treatment with MPEP corresponding to postoperative days 14–19, 20–25, and 26–31, respectively. *,°Significant difference from preoperative and the first block of postoperative performance, respectively (p<0.05, PLSD Fisher's test after significant ANOVA).
Combined A2A and mGlu5 receptors blockade in 6-OHDA-lesioned rats
The coadministration of CSC and MPEP, whatever the combination of doses used (ie low vs high doses) significantly affected correct and delayed responses (significant main treatment effect F4,84=16.11 and F4,84=31.32, respectively, all p<0.01). Post hoc analysis on CSC and MPEP coinjected groups further revealed that the treatment had effectively, but differentially, increased the number of correct responses (Figure 5a, b). The highest doses combination (CSC 1.25 mg/kg+MPEP 1.5 mg/kg) only partially restored the level of prelesion performance (postsurgery vs third week, p<0.05, but presurgery vs third week, p<0.01, Fisher's PLSD test, Figure 5b). The cotreatment also rapidly diminished the number of delayed responses (postsurgery vs first, second, and third week, all p<0.01, Fisher's PLSD test) however without reaching the level of preoperative performances (presurgery vs first, second, and third week, p<0.05, Fisher's PLSD test). Conversely, the lowest doses combination of CSC (0.625 mg/kg) and MPEP (0.375 mg/kg), which were ineffective in a single administration, significantly abolished the deficits produced by 6-OHDA lesions by gradually increasing the number of correct responses inducing a complete recovery of the preoperative performances by the end of the second week of treatment (postsurgery vs first, second, and third week, all p<0.01, Fisher's PLSD test). Furthermore, the mean preoperative correct responses of 69±2.9 were significantly increased to 73±2.5 at the last week of treatment (presurgery vs third week, p<0.05, Fisher's PLSD test; Figure 5a). The number of delayed responses after low doses CSC–MPEP cotreatment was found to be significantly different from postoperative sessions (postsurgery vs first, second, and third week, all p<0.01; Fisher's PLSD test). In particular, a full recovery of preoperative level of delayed responses was observed as early as the second week of treatment (no significant difference presurgery vs second and third week, NS, Fisher's PLSD test). Post hoc analysis further confirmed that CSC–MPEP coadministration significantly counteracted the lengthening of RTs induced by the lesion (postsurgery vs first, second, and third week, all p<0.01 for both treatments; Fisher's PLSD test, see Figure 6b). Furthermore, as illustrated in Figure 7a, the initial rightward shifting towards longer values of RTs after 6-OHDA lesions was completely reversed by low doses of CSC–MPEP treatment and the RTs distributions at the pre- and postoperative third week of treatment were found to overlap each other. As predicted by the assumption that rats would use the conditional probability of the stimulus occurrence, RTs were found to be faster as the delays increased thus revealing appropriate preparatory levels (Figure 7b). The overall ANOVA with repeated measures on time and delays indicated a significant interaction between blocks × foreperiods (F12,84=2.03, p<0.05), a significant main effect of foreperiods (F3,21=74.27, p<0.01) and a significant main effect of time (F4,28=17.85, p<0.01). In the preoperative session, a delay-dependent decrease of RTs was observed (F3,21=24.59, p<0.01), which was not modified after 6-OHDA lesions (F3,21=43.83, p<0.01) showing that the motor preparatory processes were not altered by the lesion. CSC–MPEP cotreatment at low doses reduced the enhanced RTs at each foreperiod without altering the delay-dependent speeding of RTs (Figure 7b).
Effects of combined administration of the A2A receptor antagonist CSC and the mGlu5 receptors antagonist MPEP at different doses ((a) CSC 0.625 mg/kg+MPEP 0.375 mg/kg and (b) CSC 1.25 mg/kg+MPEP 1.5 mg/kg) on correct (CR) and delayed (DL) responses after 6-OHDA lesion. Vertical axes represent the mean number of responses±SEM per block of six sessions. Pre (days 6–1), post (day 8–13) and 3 weeks of daily treatment with CSC and MPEP corresponding to postoperative days 14–19, 20–25, and 26–31, respectively, *,°Significant difference from preoperative and the first block of postoperative performance, respectively (p<0.05, PLSD Fisher's test after significant ANOVA).
DISCUSSION
In the present study, we show that subthreshold doses of the adenosine A2A receptor selective antagonist CSC administered concomitantly with the selective mGlu5 antagonist MPEP have a potent beneficial effect on the motor deficits produced by striatal bilateral 6-OHDA injections. In the present model of PD, the partial striatal dopaminergic denervation increased delayed responses and RTs, suggesting a deficit in movement initiation (eg akinesia) similar to that observed in the early stage of Parkinsonism (Gauntlett-Gilbert and Brown, 1998; Breysse et al, 2002). These akinetic deficits were fully reversed by either a single treatment of CSC or MPEP at the higher doses tested or by a combined treatment with ineffective doses of each compound.
Adenosine A2A Receptors Antagonism as Anti-Parkinsonian Strategy
Selective A2A antagonists were previously found to be active in different models of PD. In rats with unilateral 6-OHDA lesions of the dopaminergic nigrostriatal pathway, the contralateral turning behavior induced by DA agonists is potentiated by antagonists of A2A receptors (Jiang et al, 1993; Pinna et al, 1996; Fenu et al, 1997; Stromberg et al, 2000; Koga et al, 2000). Conversely, A2A receptor agonists prevented the rotational behavior produced by apomorphine (Morelli et al, 1994). Recent evidence suggest that the antagonism of striatal A2A receptors may represent an alternative therapeutic approach to PD and systemic or intrastriatal infusions of selective A2A receptor antagonists, CSC or MSX-3, respectively, were found to reverse the cataleptic response induced by DA receptors blockade (Hauber et al, 1998, 2001). When tested in monkeys treated with 1-methyl-4-phenyl-1,2,5,6,-tetrahydropyridin (MPTP), the A2A antagonist KW-6002 produced a significant improvement in motor disability (Kanda et al, 1998) and potentiated L-DOPA-mediated effects (Grondin et al, 1999). The present results further demonstrate that the selective A2A receptor antagonists CSC also potently reverse the akinetic deficits produced in partially DA denervated rats. The possibility that CSC may produce its effect by blockade of A1 receptors may not be ruled out because it is selective but not specific to A2A receptors. However, CSC was found to be 520-fold selective in binding assays at rat brain A2A vs A1 receptors (Zocchi et al, 1996; Jacobson et al, 1993) and very efficient in displacing in nanomolar concentration the selective A2A agonist [3H]CGS21680 from rat striatal membranes (Ki 54 nM). Interestingly, preliminary studies show that the selective A2A antagonist KW-6002 is able to improve the akinetic deficits produced by 6-OHDA lesions in the same RT task (R Coccurello and M Amalric, unpublished observations). Consequently, it is very likely that CSC exerts its effect via the blockade of A2A receptors.
One potential drawback of the clinical use of the DA-mimicking properties of adenosine antagonists is related to the possible development of tolerance (Fredholm et al, 1999). Development of tolerance, as well as the potential occurrence of the so-called ‘inversion effect’ (eg the repeated administration of an antagonist can induce agonist-like effects), which might follow a long-lasting treatment, has severely limited the clinical usefulness of adenosine antagonists. The reversal of the akinetic deficits showed in the present study by a 3-week treatment with CSC constitute the first demonstration that the chronic A2A receptors blockade is able to improve motor control without eliciting any side effects nor tolerance. This result is consistent with the idea that tolerance following repeated caffeine or theophylline treatment (Fredholm et al, 1999) mostly involves adenosine A1 receptors and indirectly the D1 DA receptors (Fredholm et al, 1999; Halldner et al, 2000).
Metabotropic Glutamate 5 Receptors Antagonism as Anti-Parkinsonian Strategy
We confirm here that blocking mGlu5 receptors by chronic MPEP treatment is also able to reverse akinesia. Systemic or intrastriatal administration of group I mGluR (subtypes 1 and 5) antagonists reversed catalepsy induced by a DA receptor blockade or DA depletion (Konieczny et al, 1998; Dawson et al, 2000; Ossowska et al, 2001). In unilateral and bilateral 6-OHDA models of PD, a chronic but not acute treatment with MPEP induced ipsilateral circling behavior and produced a full recovery of akinesia in the RT task (Spooren et al, 2000; Breysse et al, 2002). The selectivity of MPEP action on mGluR5 has recently been questioned since it could act as an allosteric potentiator of mGluR4 (Mathiesen et al, 2003) and exert its effects through this group III mGluRs subtype. Although this nonselective action cannot be ruled out the range of doses of MPEP below 10 μM used in the present study possess a better affinity for mGluR5 than for mGluR4 (Anderson et al, 2002). Nevertheless, as previously shown (Breysse et al, 2002) the range of doses alleviating 6-OHDA-induced deficits without inducing side effects is relatively narrow. To circumvent this problem we have therefore investigated the possible advantages of a coadministration of selective adenosine A2A and mGlu5 receptor antagonists.
Functional Interaction Between A2A and mGlu5 Receptors
Our results show that CSC and MPEP coadministration is able to rapidly reduce the proportion of delayed responses and shorten RTs in comparison to a single treatment and that such improvement is not accompanied by any manifestations of abnormal movements. This finding indicates that the combined blockade of A2A and mGlu5 receptors is even more effective in reversing akinesia than each treatment administered separately. The animals treated with subthreshold doses of A2A and mGlu5 receptors antagonists exhibit the most efficient (eg faster) and complete reinstatement of the preoperative level of performance by the end of the second week of chronic treatment. The pronounced reduction of the number of delayed responses is also mirrored by the significant increase of correct responses as compared to the preoperative performances. In contrast, when CSC and MPEP were combined at doses effective in a single treatment, the progressive amelioration of the akinetic deficits observed during the first 2 weeks of cotreatment did not show any further improvement during the last week of treatment.
Adenosine A2A receptor mRNA is highly expressed in the striatum, nucleus accumbens, olfactory tubercle, and the globus pallidus (Jarvis et al, 1989) where group I mGlu receptors (including subtypes 1 and 5) are also strongly expressed (Testa et al, 1994). In addition, group I mGlu receptors are present in the subthalamic nucleus (STN) and the substantia nigra pars reticulata (SNr) (Tallaksen-Greene et al, 1998; Testa et al, 1994). In the striatum, adenosine A2A receptors are predominantly expressed by γ-amino butyric acid (GABA)-enkephalin striatopallidal neurons, where they colocalize with DA D2 receptors (Fink et al, 1992; Martinez-Mir et al, 1991) and are also present in 25% of cholinergic interneurons (Schiffmann et al, 1991; Fredholm et al, 2001). Interestingly, mGlu5 receptors show a striking similar localization in the striatopallidal GABAergic projection neurons and interneurons in primates (Smith et al, 2000), so providing a morphological basis for the possible existence of functional interactions between striatal A2A and mGlu5 receptors. The simultaneous chronic blockade of A2A and mGlu5 receptors with doses that were fully effective in separate administration might have induced a competing action at the level of a common signal transduction pathway. After 2 weeks of chronic coincident blockade, the effect achieved by each antagonist on its own appears to be saturated and neither a further improvement nor a successive deterioration could be observed. Alternatively, the concurrent blockade of each receptor may have produced a competing action on a final common output pathway of the basal ganglia.
According to the current model of the basal ganglia functional organization (Albin et al, 1989), the degeneration of nigrostriatal DA neurons produces an upregulation of the striatopallidal GABA pathway (indirect pathway). The increased pallidal GABAergic activity induce the disinhibition of the STN and the SNr, which are overactive in Parkinsonian conditions (Awad et al, 2000) and thought to be responsible of the reduced thalamocortical activity (DeLong, 1990). Therefore, it is rational to hypothesize that both A2A and mGlu5 receptors antagonist may alleviate the increased activity of the striatal neurons projection to the GP which, in turn, would result in the stimulation of thalamic glutamatergic projections to the cortex and then to the striatum. Electrophysiological studies have reported that adenosine A2A receptors may control the GABA-evoked overflow in striatum and globus pallidus (Corsi et al, 1999; Kirk and Richardson, 1994; Mayfield et al, 1993), and synergistically increase the pallidal GABA levels when agonists acting at both A2A/mGlu5 receptors are coinjected (Diaz-Cabiale et al, 2002). The systemic injection of CSC is known to reverse the catalepsy produced by the bilateral blockade of D2 DA receptors in the striatum with sulpiride (Hauber et al, 2001) and to decrease contralateral rotation induced by intrastriatal and intrasubthalamic nucleus administration of a nonselective groups I and II mGlu receptors agonist, 1S,3R-ACPD (Feeley-Kearney and Albin, 1995). Furthermore, intrastriatal administration of selective antagonists of group I mGlu receptors (AIDA) inhibited the haloperidol-induced muscle rigidity (Wolfarth et al, 2000). Recent evidence have shown that agonists acting at A2A and group I mGlu receptors were able to reduce either separately or in costimulation the high-affinity state of the DA D2 receptor binding sites (Ferré et al, 1999). A functional antagonistic relationship of D2 with A2A and mGlu5 receptors is further supported by a recent study showing that the mGlu5 receptor agonist, CHPG, inhibit the D2-induced turning behavior in unilateral 6-OHDA-lesioned animals, an effect greatly potentiated by a joint administration with the A2A receptor agonist CGS 21680 (Popoli et al, 2001). It might then be suggested that the complete recovery of DA-induced deficits observed in the present study after a concomitant blockade of mGlu5 and A2A receptors result from a normalization of the overactive striatopallidal GABA pathway.
An influence of MPEP on extrastriatal mGlu5 receptors is, however, possible since this compound was found to inhibit the neuronal activity of the STN, increased after stimulation of group I mGluRs (Awad et al, 2000; Rouse et al, 2000). Interestingly, with the same model of partial DA denervation as used in the present study, we have recently shown that MPEP chronic treatment alleviate the akinesia via a normalization of the neuronal metabolic activity in the STN and the SNr, which was profoundly increased by the lesion (Breysse et al, 2003). Therefore, we hypothesized that a simultaneous blockade of A2A receptors in the striatum and pallidum and mGlu5 receptors in the STN and SNr may potentiate their action in reducing the overactive outflow of the basal ganglia output structures and contribute to the regulation of the motor disability related to the Parkinsonian conditions. However, a subtle equilibrium in the degree of the blockade of these two receptors appears to be crucial since the combination of each compound at doses that were effective alone is showed to less efficiently counteract the akinetic deficits. This is in line with the fact that an altered balance between the direct and indirect output pathways of the basal ganglia may produce competing effects on motor output (DeLong, 1990).
Interestingly, only a chronic treatment either with CSC or MPEP was found to greatly ameliorate the Parkinsonian deficits. The acute injection of each compound administered separately or in combination was without effect. The present findings consistently confirm the beneficial effects of a chronic MPEP treatment on the Parkinsonian deficits (Breysse et al, 2002). These results also demonstrate for the first time that a chronic A2A blockade, via the administration of its selective antagonist CSC, is effective against the 6-OHDA-induced akinetic deficits. In view of the recent demonstration that A2A and mGlu5 receptors can form heteromeric complexes (Ferré et al, 2002) as well as coaggregate and cointernalize with the DA D2 receptors after their prolonged stimulation (Hillion et al, 2002), the idea of a reciprocal adaptation of these receptors subtypes appear to be further corroborated. It seems therefore conceivable that intramembrane interactions implying common final pathways between striatal A2A and mGlu5 receptors could have been involved in the functional synergism underlying the efficient recovery of the akinesia observed in the present study. A specific mechanism by which this functional relationship may occur at the molecular level would be to activate the signal transduction molecule DARPP-32 (DA- and cyclic AMP-regulated phosphoprotein of mol. wt of 32 kDa), which has been shown to be abundantly expressed in all striatal medium spiny neurons (Walaas and Greengard, 1984; Ouimet et al, 1998) and to play an essential modulatory role in DA transmission (Fienberg et al, 1998). A coactivation of adenosine A2A and mGlu5 receptors has been recently revealed to be responsible of the synergistic potentiation of the state of phosphorylation of DARPP-32 (Nishi et al, 2003) and c-fos expression (Ferré et al, 2002) in striatal neurons. The functional cross talk that links mGlu5 and A2A receptors may therefore underlie the behavioral recovery observed in the present study.
The described synergic effects produced by each drug, ineffective on its own, raises therefore the opportunity to promote selectively, yet indirectly, the dopaminergic transmission and to control over time the hyperactivity of the output structures of the striatopallidal pathway, in lack of specific side effects. The present study demonstrates that a balanced combination between single, ineffective doses of highly selective mGlu5 and A2A antagonists might really represent a novel nondopaminergic therapeutic approach for the treatment of the PD invalidating motor deficits.
References
Albin RL, Young AB, Penney JB (1989). The functional anatomy of basal ganglia disorders. Trends Neurosci 12: 366–375.
Amalric M, Baunez C, Nieoullon A (1995a). Does the blockade of excitatory amino acid transmission in the basal ganglia simply reverse reaction time deficits induced by dopamine inactivation? Behav Pharmacol 6: 508–519.
Amalric M, Moukhles H, Nieoullon A, Daszuta A (1995b). Complex deficits on reaction time performance following bilateral intrastriatal 6-OHDA infusion in the rat. Eur J Neurosci 7: 972–980.
Anderson JJ, Rao SP, Rowe B, Giracello DR, Holtz G, Chapman DF et al (2002). [3H]Methoxymethyl-3-[(2-methyl-1,3-thiazol-4-yl) ethynyl]pyridine binding to metabotropic glutamate receptor subtype 5 in rodent brain: in vitro and in vivo characterization. J Pharmacol Exp Ther 303: 1044–1051.
Awad H, Hubert GW, Smith Y, Levey AI, Conn PJ (2000). Activation of metabotropic glutamate receptor 5 has direct excitatory effects and potentiates NMDA receptor currents in neurons of the subthalamic nucleus. J Neurosci 20: 7871–7879.
Baja-Jimenez W, Sherzai A, Dimitrova T, Favit A, Bibbiani F, Gillespie M et al (2003). Adenosine A2A receptor antagonist treatment of Parkinson's disease. Neurology 61: 293–296.
Breysse N, Amalric M, Salin P (2003). Metabotropic glutamate 5 receptor blockade alleviates akinesia by normalizing activity of selective basal-ganglia structures in Parkinsonian rats. J Neurosci 23: 8302–8309.
Breysse N, Baunez C, Spooren W, Gasparini F, Amalric M (2002). Chronic but not acute treatment with a metabotropic glutamate 5 receptor antagonist reverses the akinetic deficits in a rat model of parkinsonism. J Neurosci 22: 5669–5678.
Corsi C, Melani A, Bianchi L, Pepeu G, Pedata F (1999). Effect of adenosine A2A receptor stimulation on GABA release from the striatum of young and aged rats in vivo. Neuroreport 16: 3933–3937.
Dawson L, Chadha A, Megalou M, Duty S (2000). The group II metabotropic glutamate receptor agonist, DCG-IV, alleviates akinesia following intranigral or intraventricular administration in the reserpine-treated rat. Br J Pharmacol 129: 541–546.
DeLong MR (1990). Primate models of movement disorders of basal ganglia origin. Trends Neurosci 13: 281–285.
Diaz-Cabiale Z, Meritxell V, Del Arco A, O'Connor W, Harte MK, Müller CE et al (2002). Metabotropic glutamate mGlu5 receptor-mediated modulation of the ventro-pallidal GABA pathway in rats. Interactions with adenosine A2A and dopamine D2 receptors. Neurosci Lett 324: 154–158.
Feeley-Kearney JA, Albin RL (1995). Adenosine A2 receptor-mediated modulation of contralateral rotation induced by metabotropic glutamate receptor activation. Eur J Pharmacol 287: 115–120.
Fenu S, Pinna A, Ongini E, Morelli M (1997). Adenosine A2A receptor antagonism potentiates L-DOPA-induced turning and c-Fos expression in 6-hydroxydopamine-lesioned rats. Eur J Pharmacol 321: 143–147.
Ferré S, Karcz-Kubicha M, Hope BT, Popoli P, Burguen J, Gutierrez MA et al (2002). Synergistic interaction between adenosine A2A and glutamate mGlu5 receptors: Implications for striatal neuronal function. Proc Natl Acad Sci USA 99: 11940–11945.
Ferré S, Popoli P, Rimondini R, Reggio R, Kehr J, Fuxe K (1999). Adenosine A2A and group I metabotropic glutamate receptors synergistically modulate the binding characteristics of dopamine D2 receptors in the rat striatum. Neuropharmacology 38: 129–140.
Fienberg AA, Hiroi N, Mermelstein PG, Song W, Snyder GL, Nishi A et al (1998). DARPP-32: regulator of the efficacy of dopaminergic neurotransmission. Science 281: 838–842.
Fink JS, Weaver DR, Rivkees SA, Peterfreund RA, Pollack A, Adler EM et al (1992). Molecular cloning of the rat A2 adenosine receptor: selective co-expression with D2 dopamine receptors in rat striatum. Molec Brain Res 14: 186–195.
Fredholm BB, Battig K, Holmen J, Nehlig A, Zvartau EE (1999). Actions of caffeine in the brain with special reference to factors that contribute to its widespread use. Pharmacol Rev 51: 83–133.
Fredholm BB, Ijzerman AP, Jacobson KA, Klotz KN, Linden J (2001). Nomenclature and classification of adenosine receptors. Pharmacol Rev 53: 527–552.
Gauntlett-Gilbert J, Brown VJ (1998). Reaction time deficits and Parkinson's disease. Neurosci and Biobehav Rev 22: 865–881.
Grondin R, Bedard PJ, Hadj Tahar A, Gregoire L, Mori A, Kase H (1999). Antiparkinsonian effect of a new selective adenosine A2A receptor antagonist in MPTP-treated monkeys. Neurology 52: 1673–1677.
Halldner L, Lozza G, Lindstrom K, Fredholm BB (2000). Lack of tolerance to motor stimulant effects of a selective adenosine A2A receptor antagonist. Eur J Pharmacol 406: 345–354.
Hauber W, Nagel J, Sauer R, Muller CE (1998). Motor effects induced by a blockade of adenosine A2A receptors in the caudate-putamen. Neuroreport 9: 1803–1806.
Hauber W, Neuscheler P, Nagel J, Muller CE (2001). Catalepsy induced by a blockade of dopamine D1 or D2 receptors was reversed by a concomitant blockade of adenosine A2A receptors in the caudate-putamen of rats. Eur J Neurosci 14: 1287–1293.
Hauser RA, Hubble JP, Truong DD (2003). Randomized trial of the adenosine A2A receptor antagonist istradefylline in advanced Parkinson's disease. Neurology 61: 297–303.
Hillion J, Canals M, Torvinen M, Casado V, Scott R, Terasmaa A et al (2002). Coaggregation, cointernalization and codesensitization of adenosine A2A receptors and dopamine D2 receptors. J Biol Chem 277: 18091–18097.
Jacobson KA, Nikodijevic O, Padgett WL, Gallo-Rodriguez C, Maillard M, Daly JW (1993). 8-(3-Chlorostyryl)caffeine (CSC) is a selective A2-adenosine antagonist in vitro and in vivo. FEBS Lett 323: 141–144.
Jarvis MF, Schulz R, Hutchison AJ, Do UH, Sills MA, Williams M (1989). [3H]CGS 21680, a selective A2 adenosine receptor agonist directly labels A2 receptors in rat brain. J Pharmacol Exp Ther 251: 888–893.
Javitch JA, Strittmatter SM, Snyder SH (1985). Differential visualization of dopamine and norepinephrine uptake sites in rat brain using 3Hmazindol autoradiography. J Neurosci 5: 1513–1521.
Jiang H, Jackson-Lewis V, Muthane U, Dollison A, Ferreira M, Espinosa A et al (1993). Adenosine receptor antagonists potentiate dopamine receptor agonist-induced rotational behavior in 6-hydroxydopamine-lesioned rats. Brain Res 613: 347–351.
Kanda T, Jackson MJ, Smith LA, Pearce RK, Nakamura J, Kase H et al (1998). Adenosine A2A antagonist: a novel antiparkinsonian agent that does not provoke dyskinesia in parkinsonian monkeys. Ann Neurol 43: 507–513.
Kirk IP, Richardson PJ (1994). Adenosine A2A receptor-mediated modulation of striatal [3H]GABA and [3H]acetylcholine release. J Neurochem 62: 960–966.
Koga K, Kurokawa M, Ochi M, Nakamura J, Kuwana Y (2000). Adenosine A2A receptor antagonists KF17837 and KW-6002 potentiate rotation induced by dopaminergic drugs in hemi-Parkinsonian rats. Eur J Neurosci 408: 249–255.
Konieczny J, Ossowska K, Wolfarth S, Pilc A (1998). LY354740, a group II metabotropic glutamate receptor agonist with potential antiparkinsonian properties in rats. Naunyn Schmiedebergs Arch Pharmacol 358: 500–502.
Martinez-Mir MI, Probst A, Palacios JM (1991). Adenosine A2 receptors: selective localization in the human basal ganglia and alterations with disease. Neuroscience 42: 697–703.
Mathiesen JM, Svendsen N, Brauner-Osborne H, Thomsen C, Ramirez MT (2003). Positive allosteric modulation of the human metabotropic glutamate receptor 4 (hmGluR4) by SIB-1893 and MPEP. Br J Pharmacol 138: 1026–1030.
Mayfield RD, Suzuki F, Zahniser NR (1993). Adenosine A2A receptor modulation of electrically evoked endogenous GABA release from slices of globus pallidus. J of Neurochem 60: 2334–2337.
Morelli M, Fenu S, Pinna A, Di Chiara G (1994). Adenosine A2 receptors interact negatively with dopamine D1 and D2 receptors in unilaterally 6-hydroxydopamine-lesioned rats. Eur J Pharmacol 251: 21–25.
Morelli M, Wardas J (2001). Adenosine A2A receptor antagonists: potential therapeutic and neuroprotective effects in Parkinson's disease. Neurotoxicity Res 3: 545–556.
Nishi A, Liu F, Matsuyama S, Hamada M, Higashi H, Nairn AC et al (2003). Metabotropic mGlu5 receptors regulate adenosine A2A receptor signaling. Proc Natl Acad Sci USA 100: 1322–1327.
Ossowska K, Konieczny J, Wolfarth S, Wieronska J, Pilc A (2001). Blockade of the metabotropic glutamate receptor subtype 5 (mGluR5) produces antiparkinsonian-like effects in rats. Neuropharmacology 41: 413–420.
Ouimet CC, Langley-Gullion KC, Greengard P (1998). Quantitative immunocytochemistry of DARPP-32-expressing neurons in the rat caudato-putamen. Brain Res 808: 8–12.
Paxinos G, Watson C (1986). The Rat Brain in Stereotaxic Coordinates, (Edition 2) Academic Press: Sydney.
Pinna A, Di Chiara G, Wadas J, Morelli M (1996). Blockade of A2A adenosine receptors positively modulates turning behaviour and c-fos expression induced by D1 agonists in dopamine-denervated rats. Eur J Neurosci 8: 1176–1181.
Popoli P, Pezzola A, Torvinen M, Reggio R, Pintor A, Scarchilli L et al (2001). The selective mGlu5 receptor agonist CHPG inhibits quinpirole-induced turning in 6-hydroxydopamine-lesioned rats and modulates the binding characteristics of dopamine D2 receptors in the rat striatum. Neuropsychopharmacology 25: 505–513.
Rouse ST, Marino MJ, Bradley SR, Awad H, Wittmann M, Conn PJ (2000). Distribution and roles of metabotropic glutamate receptors in the basal ganglia motor circuit: implications for treatment of Parkinson's disease and related disorders. Pharmacol Ther 88: 427–435.
Schiffmann SN, Jacobs O, Vaderhaeghen JJ (1991). Striatal restricted adenosine A2 receptor (RDC8) is expressed by enkephalin but not by substance P neurons: an in situ hybridization histochemistry study. J Neurochem 57: 1062–1067.
Smith Y, Charara A, Hanson JE, Paquet M, Levey AI (2000). GABA(B) and group I metabotropic glutamate receptors in the striatopallidal complex in primates. J Anat 196: 555–576.
Spooren WP, Gasparini F, Bergmann R, Kuhn R (2000). Effects of the prototypical mGlu(5) receptor antagonist 2-methyl-6- (phenylethynyl)-pyridine on rotarod, locomotor activity and rotational responses in unilateral 6-OHDA-lesioned rats. Eur J Pharmacol 406: 403–410.
Stromberg I, Popoli P, Muller CE, Ferre S, Fuxe K (2000). Electrophysiological and behavioural evidence for an antagonistic modulatory role of adenosine A2A receptors in dopamine D2 receptor regulation in the rat dopamine-denervated striatum. Eur J Neurosci 12: 4033–4037.
Svenningsson P, Le Moine C, Fisone G, Fredholm BB (1999). Distribution, biochemistry and function of striatal adenosine A2A receptors. Prog Neurobiol 59: 355–396.
Svenningsson P, Lindskog M, Rognoni F, Fredholm BB, Greengard P, Fisone G (1998). Activation of adenosine A2A receptor and dopamine D1 receptors stimulates cyclic AMP-dependent phosphorylation of DARPP-32 in distinct population of striatal projection neurons. Neuroscience 84: 223–228.
Tallaksen-Greene SJ, Kaatz KW, Romano C, Albin RL (1998). Localization of mGluR1-like immunoreactivity and mGlur5-like immunoreactivity in identified populations of striatal neurons. Brain Res 780: 210–217.
Testa CM, Standaert DG, Young AB, Penney JB (1994). Metabotropic glutamate receptor mRNA expression in the basal ganglia of the rat. J Neurosci 14: 3005–3018.
Walaas SI, Greengard P (1984). DARPP-32, a dopamine- and adenosine 3′ : 5′-monophosphate-regulated phosphoprotein enriched in dopamine-innervated brain regions. I. Regional and cellular distribution in the rat brain. J Neurosci 4: 84–98.
Wichmann T, DeLong MR (1997). Physiology of the basal ganglia and pathophysiology of movement disorders of basal ganglia origin. In: Watts RL (eds). Movement Disorders: Neurological Principles and Practice. McGraw-Hill: New York. pp 87–97.
Wolfarth S, Konieczny J, Lorenc-Koci E, Ossowska K, Pilc A (2000). The role of metabotropic glutamate receptor (mGluR) ligands in parkinsonian muscle rigidity. Amino Acids 19: 95–101.
Zocchi C, Ongini E, Conti A, Monopoli A, Negretti A, Baraldi PG et al (1996). The non-xanthine heterocyclic compound SCH 58261 is a new potent and selective A2A adenosine receptor antagonist. J Pharmacol Exp Ther 276: 398–404.
Acknowledgements
This research was supported by the Centre National de la Recherche Scientifique, the Fondation de France (MA) and a franco-italian Galilée program by the Ministère des Affaires Etrangères and the CRUI. RC was supported by the CNR (Italy) and NB by the Fondation pour la Recherche Medicale and Institut Lilly. The authors are grateful to Dr Fabrizio Gasparini (Novartis Pharma AG, Basel, Switzerland) for the generous gift of MPEP.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Coccurello, R., Breysse, N. & Amalric, M. Simultaneous Blockade of Adenosine A2A and Metabotropic Glutamate mGlu5 Receptors Increase their Efficacy in Reversing Parkinsonian Deficits in Rats. Neuropsychopharmacol 29, 1451–1461 (2004). https://doi.org/10.1038/sj.npp.1300444
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300444
Keywords
This article is cited by
-
Promising biomarkers and therapeutic targets for the management of Parkinson's disease: recent advancements and contemporary research
Metabolic Brain Disease (2023)
-
The mGlu5 Receptor Protomer-Mediated Dopamine D2 Receptor Trans-Inhibition Is Dependent on the Adenosine A2A Receptor Protomer: Implications for Parkinson’s Disease
Molecular Neurobiology (2022)
-
Adenosine A2A receptor inhibition reduces synaptic and cognitive hippocampal alterations in Fmr1 KO mice
Translational Psychiatry (2021)
-
PDZ Scaffold Protein CAL Couples with Metabotropic Glutamate Receptor 5 to Protect Against Cell Apoptosis and Is a Potential Target in the Treatment of Parkinson's Disease
Neurotherapeutics (2019)
-
Group I metabotropic glutamate receptors in the primate motor thalamus: subsynaptic association with cortical and sub-cortical glutamatergic afferents
Brain Structure and Function (2019)