Abstract
BACKGROUND:
Infants of diabetic mothers (IDMs) are at an increased risk for thromboembolic disease. The mechanism(s) to explain this association is unclear. We hypothesized that the pathophysiology of thrombosis in IDMs is multifactorial and likely involves interactions among genetic and acquired factors affecting the procoagulant, anticoagulant and fibrinolytic pathways.
OBJECTIVE:
To compare the prevalence of common prothrombotic risk factors in a cohort of IDMs to a matched control group.
PATIENTS/METHODS:
Full-term infants born to mothers with diet controlled (A1-IDM) (N=17), insulin requiring diabetes (ID-IDM) (N=20) and healthy term infants (controls) (N=20) matched for mode of delivery had cord blood collected at delivery. Samples were analyzed for the following: factor V Leiden (FVL), prothrombin 20210A (P20210A), methylenetetrahydrofolate reductase C677 T (MTHFR), Factor VIII (FVIII), Protein C (PC), Lipoprotein(a) (Lp(a)) and plasminogen activator inhibitor-1 (PAI-1).
RESULTS:
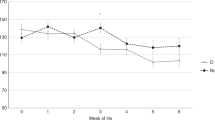
None of the infants had a clinically apparent thrombotic event. IDM mothers and their infants were clinically similar to controls except for a higher prevalence of hypoglycemia (30 vs 0%; p=0.005). There was no significant difference in the prevalence of the common genetic risk factors (FVL, P20210A, MTHFR) FVIII, or PAI-1 levels. Elevated Lp(a) levels were seen more frequently in IDMs than Controls (40 vs 20%) but this difference was not statistically significant. The PC activity (%) was significantly decreased in the IDM group compared to controls, 35±12 vs 44±9 (p<0.005). A1-IDM had lower PC activity compared to ID-IDM (p=0.05) and controls (p=0.001).
CONCLUSIONS:
PC deficiency is likely one mechanism to explain thrombosis in IDMs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Edstrom CS, Christensen RD . Evaluation and treatment of thrombosis in the neonatal intensive care unit. Clin Perinatol 2000;27 (3):623–641.
Oppenheimer EH, Esterly JR . Thrombosis in the newborn: comparison between infants of diabetic and nondiabetic mothers. J Pediatr 1965;67 (4):549–556.
Green DW, Mimouni F, Khoury J . Decreased platelet counts in infants of diabetic mothers. Am J Perinatol 1995;12 (2):102–105.
Ambrus CM, Ambrus JL, Courey N, et al. Inhibitors of fibrinolysis in diabetic children, mothers, and their newborn. Am J Hematol 1979;7 (3):245–254.
Easa D, Coen RW . Coagulation studies in infants of diabetic mothers. Am J Dis Child 1979;133 (8):851–852.
Stuart MJ, Sunderji SG, Allen JB . Decreased prostacyclin production in the infant of the diabetic mother. J Lab Clin Med 1981;98 (3):412–416.
Dadak C, Hoche C, Ulrich W, Sinzinger H . Prostacyclin synthesis in human umbilical vessels]. Wien Klin Wochenschr 1982;94 (20):550–553.
Nappi C, Cerbone AM, Papa R, et al. Increased retraction of fibrin clots by endothelial cells of infants of diabetic mothers. Biol Res Pregnancy Perinatol 1985;6 (3):141–142.
Seligsohn U, Lubetsky A . Genetic susceptibility to venous thrombosis. N Engl J Med 2001;344 (16):1222–1231.
Linfert DR, Rezuke WN, Tsongalis GJ . Rapid multiplex analysis for the factor V Leiden and prothrombin G20210A mutations associated with hereditary thrombophilia. Conn Med 1998;62 (9):519–525.
Schneider DM, von Tempelhoff GF, Herrle B, Heilmann L . Maternal and cord blood hemostasis at delivery. J Perinat Med 1997;25 (1):55–61.
Borenstein M, Rothstein H, Chen J, In: Sample Power 1.2 ed. Chicago, IL: SPSS Inc.; 1997.
Manco-Johnson MJ, Abshire TC, Jacobson LJ, Marlar RA . Severe neonatal protein C deficiency: prevalence and thrombotic risk. J Pediatr 1991;119 (5):793–798.
Edstrom CS, Christensen RD, Andrew M . Developmental aspects of blood hemostasis and disorders of coagulation and fibrinolysis in the neonatal period. In: Christensen RD, editor. Hematologic Problems of the Neonate. Philadelphia: W.B. Saunders Company; 2000. p. 239–272.
Wing-Harkins DL, Dellinger GW, Lynch C, Mihas AA . Eosinophilic gastro-enteritis associated with protein-losing enteropathy and protein C deficiency. J Int Med Res 1996;24 (1):155–163.
Fisher Jr CJ, Yan SB . Protein C levels as a prognostic indicator of outcome in sepsis and related diseases. Crit Care Med 2000;28(9 Suppl):S49–56.
Bellart J, Gilabert R, Fontcuberta J, Carreras E, Miralles RM, Cabero L . Coagulation and fibrinolysis parameters in normal pregnancy and in gestational diabetes. Am J Perinatol 1998;15 (8):479–486.
Vukovich TC, Schernthaner G . Decreased protein C levels in patients with insulin-dependent type I diabetes mellitus. Diabetes 1986;35 (5):617–619.
Jenkins AJ, Best JD . The role of lipoprotein(a) in the vascular complications of diabetes mellitus. J Intern Med 1995;237 (4):359–365.
Acknowledgements
We thank all the nurses in the Labor and Delivery at Hartford Hospital and midlevel practitioners in the Neonatal Intensive Care Unit at Connecticut Children's Medical Center, whose assistance was invaluable.
Author information
Authors and Affiliations
Additional information
The project was supported by a fellowship research grant from the Department of Neonatology, University of Connecticut.
Presented, in part, as a poster at the Society for Pediatric Research meeting, Baltimore, MD, May, 2002.
Rights and permissions
About this article
Cite this article
Sarkar, S., Hagstrom, N., Ingardia, C. et al. Prothrombotic Risk Factors in Infants of Diabetic Mothers. J Perinatol 25, 134–138 (2005). https://doi.org/10.1038/sj.jp.7211222
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211222
This article is cited by
-
Bilateral renal venous thrombosis and adrenal hemorrhage: sequential prenatal US with postnatal recovery
Pediatric Radiology (2007)