Abstract
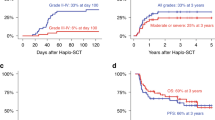
In order to determine if peripheral blood stem cells (PBSC) collected after priming with G-CSF in AML in first complete remission (CR) can be used for autologous transplantation and to evaluate the efficacy of early intensification therapy as in vivo purging, we studied 35 consecutive patients with AML in first CR. After standard induction and consolidation chemotherapy, 24 of them were treated with one (10 patients) or two (14 patients) cycles of high-dose cytarabine plus etoposide prior to PBSC collection. G-CSF was used as the priming agent. Of the 35 patients scheduled for peripheral blood stem cell transplantation (PBSCT), three relapsed before transplantation, and the 32 remaining underwent PBSCT. High-dose therapy consisted of either total body irradiation plus cyclophosphamide or busulphan plus cyclophosphamide. The median number of CD34+ cells infused was 3.24 × 106/kg (range 0.15–14). The median times to reach a PMN count of 0.5 × 109/l and a platelet count of 50 × 109/l were 12 (8–28) and 30 (11–345) days, respectively. There was no transplant-related mortality. Twelve patients relapsed between 2 and 21 months post-PBSCT. With a median follow-up of 28 months, actuarial disease-free survival (DFS) is 52.41 ± 9% in the intent-to-treat group and 57.4 ± 9.8% in patients who underwent PBSCT. The probability of DFS is significantly higher for patients who receive early intensification therapy prior to both PBSC collection and PBSCT as compared with patients that do not: 68.8 ± 10.27% vs 35.5 ± 12.6%, P = 0.0418. These results indicate the feasibility of PBSCT in AML using G-CSF-mobilized PBSC. The use of intensification treatment as ‘purging in vivo’ prior both to collection of PBSC and PBSCT significantly reduces the risk of relapse in this group of patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Martín, C., Torres, A., León, A. et al. Autologous peripheral blood stem cell transplantation (PBSCT) mobilized with G-CSF in AML in first complete remission. Role of intensification therapy in outcome. Bone Marrow Transplant 21, 375–382 (1998). https://doi.org/10.1038/sj.bmt.1701102
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1701102
Keywords
This article is cited by
-
Autologous peripheral blood stem cell transplantation with BCVAC conditioning in childhood acute myeloid leukemia
Bone Marrow Transplantation (2004)
-
The stem cell mobilizing capacity of patients with acute myeloid leukemia in complete remission correlates with relapse risk: results of the EORTC-GIMEMA AML-10 trial
Leukemia (2003)
-
Autologous stem cell transplantation for advanced acute myeloid leukemia
Bone Marrow Transplantation (2002)
-
Factors influencing hematopoietic recovery after autologous blood stem cell transplantation in patients with acute myeloblastic leukemia and with non-myeloid malignancies
Bone Marrow Transplantation (2002)
-
Double reinforcement with fludarabine/high-dose cytarabine enhances the impact of autologous stem cell transplantation in acute myeloid leukemia patients
Bone Marrow Transplantation (2001)