Key Points
-
Presents an overview on the use and pharmacology of anticoagulant medications.
-
Explores the current evidence-based management of patients on novel oral anticoagulants during oral surgical treatments.
-
Outlines recommendations for practice for the management of patients on novel oral anticoagulants in primary and secondary care settings.
Abstract
Background Haemostasis is crucial for the success of oral surgical treatment as bleeding problems can cause complications both pre- and post-operatively. Patients on anticoagulant drugs present a challenge due to their increased risk of bleeding.
Aims To review the evidence for the management of oral surgery patients on novel oral anticoagulant therapy.
Methods A literature review was conducted in May 2016 of free-text and MESH searches (keywords: apixaban, dabigatran, rivaroxaban and dental extractions) in the Cochrane Library, PubMed and CINAHL. Trial registers, professional bodies for guidelines and OpenGrey for unpublished literature were also searched. Studies were selected for appraisal after limits were applied (adult, human and English only studies) and inclusion/exclusion criteria imposed.
Results Five studies were identified for critical appraisal using the CASP tools. These were a combination of systematic reviews and case series. Two case series were excluded due to low quality evidence. Curtin et al., Davis et al. and Constantinides et al. together with guidelines from the Scottish Dental Clinical Effectiveness Programme, have highlighted a protocol in managing these patients in a dental surgical setting.
Conclusion Patients on novel anticoagulant therapy requiring dental surgery can be managed appropriately either without discontinuation of therapy or a delay in dose. For those patients at higher risks of postoperative bleeding complications, it is advised to liaise with the specialist physician.
Similar content being viewed by others
Background
Warfarin (a coumarin derivative) is the most widely used anticoagulant in the world. It is a vitamin K antagonist and inhibits vitamin K dependent synthesis of clotting factors (VII, IX, X and prothrombin II) affecting formation of fibrin clot. These factors are synthesised in the liver in precursor form and activated by carboxylation of specific glutamic acid residues which require vitamin K in its reduced form as a cofactor. Warfarin more specifically acts by inhibiting the reduction that converts the epoxide form of vitamin K to its reduced form by competitive antagonism due to molecular similarity between warfarin and vitamin K.1
In the UK it is estimated that at least 1% of the population and 8% of the over-80s are taking it regularly.2 It was first used in 1955 to treat American president Dwight D. Eisenhower for a coronary event. It is currently used in:
-
1
Prevention of venous thrombosis and embolism in rheumatic heart disease and atrial fibrillation (AF)
-
2
Treatment and prophylaxis of deep vein thrombosis (DVT) and pulmonary embolism (PE)
-
3
Stroke prophylaxis
-
4
AF and valvular heart disease (International Normalised Ratio [INR] target 23)
-
5
Mechanical heart valves (INR target 34)
However, in recent years the advent of novel oral anticoagulants (NOACs), comprising:
-
Factor Xa inhibitors: rivaroxaban (Xarelto), apixaban (Eliquis), edoxaban (Lixiana) and direct thrombin (factor IIa) inhibitor: dabigatran (Pradaxa), have been used as an alternative to warfarin to treat patients with non-valvular AF, and in the prevention of stroke and systemic embolism.
NOACs were first developed in order to improve the characteristics of an ideal oral anticoagulant (Table 1).
Rivaroxaban
Rivaroxaban is an oxazolidinone derivative and a highly selective direct Factor Xa inhibitor with good oral bioavailability. Inhibition of Factor Xa interrupts the intrinsic and extrinsic pathway of the haematological coagulation cascade (Fig. 1), inhibiting both thrombin formation and development of thrombi. Rivaroxaban does not inhibit thrombin and therefore has no effects on platelets.3 It is a drug which is taken once daily in 10 mg, 15 mg or 20 mg doses. It has a rapid onset of action of approximately 2.5–4 hours, and a half-life of 5–9 hours (increased in older patients). It is contra-indicated in patients with creatinine clearance of <15 ml/min, whereby creatinine clearance is an assessment of the rate and efficiency of kidney filtration. It can be measured by serum or urine creatinine, but most commonly by the amount of creatinine present in a urine sample collected over 24hours. Normal values for men is 97–137 ml/min and 88–128 ml/min for females (although this can be reduced in patients older than 50 years). Reduced creatinine clearance values can be indicative of kidney disease or damage (for example due to heart failure or cancer).
Thereafter in 2011, the United States Food and Drug Administration (US FDA) approved rivaroxaban for prophylaxis and treatment of DVT, which may lead to PE, in adults undergoing hip and knee replacement surgery4 and for stroke prevention in people with non-valvular AF.5 In 2012, the National Institute for Health and Clinical Excellence (NICE) recommended rivaroxaban for the prevention and treatment of venous thromboembolism (VTE).6
Apixaban
Apixaban, like rivaroxaban is a direct Factor Xa inhibitor and similarly modulates the formation of the prothrombinase complex. Apixaban does not inhibit thrombin and has no effects on platelets. It is a drug which is taken twice daily in 2.5 mg or 5 mg doses. It has a rapid onset of approximately 1–3 hours, and its half-life is 12 hours. It is contra-indicated in patients with creatinine clearance of <15 ml/min. It was approved by NICE in February 2013 for the prevention of stroke and systemic embolism in people with non-valvular AF.
Other NOACs have become available to use, such as Edoxaban (Lixiana®) which was approved by NICE in September 2015 for the same indications. There is limited data on this drug at present therefore it will not form part of the literature search within this article.
Dabigatran
Dabigatran is administered orally as the prodrug dabigatran etexilate, which is rapidly and completely converted to dabigatran after ingestion, through esterase-catalysed hydrolysis in plasma.7 It is a selective and reversible direct thrombin (factor IIa) inhibitor, which binds to the active site of the free and clot-bound thrombin molecule, so it cannot transform fibrinogen into fibrin. Dabigatran has an indirect effect on platelet formation by reducing the thrombin mediated activation of platelets.8 It is a drug which is taken twice daily in 110 mg or 150 mg doses, depending on the patient's renal function. It has a quick onset of approximately 0.5–4 hours, and its half-life is 12–15 hours (increased in patients with reduced renal functions). It is contra-indicated in patients with creatinine clearance of <30 ml/min due to a risk of overdose. Dabigatran was approved by NICE in March 2012 as a treatment to prevent stroke and systemic embolism in people with non-valvular AF. Anticoagulation is determined with the use of:
-
aPTT (activated partial thrombin time) provides a qualitative indication of anticoagulation but is not suitable for quantification of effect
-
TT (thrombin time) has a linear dose response relationship with dabigatran
-
Ecarin clotting time allows direct measurement of dabigatran activity but is not widely used.
Dabigatran has little effect on INR. In October 2015 the US FDA approved idarucizumab, a monoclonal antibody fragment (Praxbind, Boehringer Ingelheim Pharmaceuticals, Inc., Germany) as a reversal agent for patients on Dabigatran in emergency surgery, or in life-threatening or uncontrolled bleeding.8
Careful patient selection is important before considering prescribing NOACs. Patients are prescribed NOACs for prevention of stroke and systemic embolism with non-valvular AF, and at least one or more of the following:
-
Have had a stroke or transient ischaemic attack (TIA) in the past
-
Are aged 75 or older
-
Have high blood pressure
-
Have diabetes
-
Have heart failure with symptoms.
NOACs should be avoided in patients with severe renal impairment, clinically significant active bleeding, pregnancy and breast feeding, hepatic impairment or liver disease expected to have any impact on survival, concomitant treatment with systemic ketoconazole, cyclosporin, itraconazole, tacrolimus, voriconazole and dronedarone.
The current management of these patients, as with patients on other anticoagulant and antiplatelet therapy, is clinician dependent. Different surgeons provide different pre-operative advice regarding cessation or delaying of these drugs. This can provide a number of difficulties:
-
Confusion among patients regarding preoperative preparation
-
Inconsistencies among operating staff
-
Attendance at hospital accident and emergency departments with postoperative haemorrhage
-
Delays in treatment as clinicians attempt to contact physicians regards drug management.
The aim of this paper is to clarify, with the aid of evidence-based literature, protocols for the management of patients on NOACs.
Method
A literature review was conducted in May 2016 of free-text and MESH searches with the keywords: apixaban, dabigatran, rivaroxaban and dental extractions, in the Cochrane Library, PubMed and CINAHL. Trial registers, professional bodies for guidelines and OpenGrey for unpublished literature were also searched. Singular and plural forms of words, synonyms, acronyms, different spellings, brand and generic names, truncation, and lay and medical terminology were all used in the PICO analysis. Boolean operators 'OR', 'AND' and 'NOT' were all applied. Studies were selected for appraisal after limits applied (adult, human and English only studies and inclusion/exclusion criteria imposed).
Results
A review of the literature has identified five studies and one guideline for general dental practitioners in the Scottish Dental Clinical Effectiveness Programme (SDCEP). Of the five studies, two were excluded (case studies).
Curtin et al.11 highlight the lack of guidance for patients on these medications requiring dental extractions from manufacturers. General recommendations for rivaroxaban and apixaban include drug cessation for 24–48 hours before surgery dependent on the bleeding risk of the procedure. This should be followed by recommencing the drug as soon as haemostasis has been achieved. The recommendations stipulate the need to make an individual assessment with an account for the risk of bleeding versus systemic embolism. For dabigatran, manufacturer recommendations stipulate the need to measure renal function to indicate preoperative drug cessation,12 with the drug restarted soon after haemostasis. The paper highlights the adoption of this protocol by the Thrombosis Guidelines Group, which recommends dental surgical procedures should be performed 12 hours after the last dose of dabigatran, extractions performed with minimal trauma and with the use of postoperative local haemostatic measures.
NICE Clinical Knowledge Summaries advise that extraction of up to three teeth, periodontal or implant surgery is considered to have 'no clinically important bleeding risk' and recommend any procedures be carried out before the next dose of NOAC is due or 18–24 hours after the last dose (which may require missing a dose of the twice daily NOACs; dabigatran and apixaban). The drugs can be restarted six hours after haemostasis has been achieved with the use of local haemostatic measures.
Constantinides et al.7 is a systematic review of the literature. The RELY (Randomised Evaluation of Long-Term Anticoagulation Therapy) trial in 2009 highlighted the efficacy of dabigatran against warfarin. The study included 18,113 patients who were taking dabigatran for AF, 4,591 whom underwent invasive procedures (10% of which included dental procedures). The anticoagulant was stopped in these patients according to renal function. The incidence of major bleeding risk peri-operatively for invasive surgical procedures was similar for patients on dabigatran and warfarin (3.8% for 110 mg–5.1% for 150 mg dabigatran; 4.6% warfarin). However, in patients on 110 mg dabigatran twice daily there was a statistically reduced rate of major bleeding.
There was an increased risk of bleeding in those requiring emergency surgery or bridging anticoagulation. Similarly, there was 1.2% risk of thromboembolic event in both anticoagulant therapies.
The paper suggests the level of anticoagulation achieved by dabigatran is similar to warfarin at an INR of 2–3. To minimise bleeding risk (where dabigatran is continued) the recommendation is to perform surgery as late as possible after the last dose and use local haemostatic measures postoperatively. In the case of elective surgery (multiple surgical extraction), there should be consideration of drug cessation which is reliant on:
-
Patient's renal function
-
The risk of bleeding (Table 2).
Table 2 Factors affecting bleeding risk
Constantinides et al.7 also highlight that TT or aPTT performed before surgical treatment can indicate, if normal, that the anticoagulant effect of dabigatran has resolved. Due to rapid onset of the drug, dabigatran can be commenced after formation of a stable clot or as soon as reasonably possible due to the increased risk of stroke should it be discontinued.
In 2010, the ROCKET-AF study discovered a significant reduction in the number of TIAs and systemic embolic events with rivaroxaban compared with warfarin in patients with AF. The rate of major bleeding associated with an invasive procedure was 2.3% and was similar with the two anticoagulants.
As with dabigatran, the authors conclude the same protocol be followed for rivaroxaban, with discontinuation to be discussed with the patient's physician. Therefore, for uncomplicated dental extractions rivaroxaban can be continued in patients with normal renal function (where local haemostatic measures are used). Where there is an increased risk of bleeding or impaired haemostasis, like dabigatran, rivaroxaban should be discontinued 24 hours before surgery (with need for increased discontinuation if there is reduced renal function). Due to its rapid onset of action, continuation should be 24–48hours after surgery.
The ARISTOTLE trial (apixaban versus warfarin) showed similar results of bleeding (1.6% versus 1.9%) for dental extractions, colonoscopy, and ophthalmologic surgery. Constantinides et al.7 conclude there is limited data to make reliable suggestions with regards to management of these patients, but to follow the protocol outlined above until further studies can be performed.
Davis et al.13 reviews the literature in relation to dabigatran in patients requiring oral surgery. The paper considers a Cochrane review comparing NOACs with low molecular weight heparin and warfarin, which showed no statistically significant increased risk of bleeding (although studies were flawed in the classification of bleeding). As per Constantinides et al.,7 the anticoagulation effects of dabigatran are comparable to warfarin with an INR of between 2–3. The authors recommend for simple extractions that the risk of postoperative bleeding is low with local haemostatic measures. For multiple/surgical extractions or significant oral and maxillofacial procedures, clinicians should consider discontinuation of dabigatran before the procedure with timing to be determined by the patients renal function. In patients where discontinuation is not appropriate and extensive oral surgery procedures are planned, bridging to low molecular weight heparin is advised.
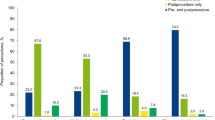
Finally, the Scottish Dental Clinical Effectiveness Programme14 have described a protocol for the dental management of patients on NOACs. Dental procedures are categorised according to 'low risk of postoperative bleeding complications' and 'high risk of postoperative bleeding complications'. For the low risk procedures, the NOACs need not be discontinued or delayed. For high risk procedures, it is suggested that patients delay or miss a dose (dependent on NOAC taken). For example, if a patient on rivaroxaban requires a high risk procedure, it may not be necessary to stop the medication at all, as it is taken once daily, as long as the procedure is performed as late as possible after the last dose. If a patient on apixaban requires a high risk procedure, it may be necessary to miss the morning/evening dose of the medication (Table 3). It is thereafter advised that NOACs may be continued no sooner than four hours after haemostasis has been achieved.
Discussion
Despite the limited evidence and lack of robust long-term clinical data on the effects of NOACs on postoperative bleeding following dental extractions, the literature review has highlighted that patients on NOACs can be managed appropriately with local haemostatic measures postoperative to dental extractions. Discontinuation of these drugs should only be considered in conjunction with the prescribing physician, due to the individual pharmacokinetic variability which is dependent on liver/renal function, sex, weight, age, drug interference and genetics. These factors will influence whether a drug should be interrupted or continued, as well as the potential risks of thromboembolic event which are considered on a case by case basis.
All papers conclude that the management of these patients should include the following (Table 4):
-
Assess the surgical and patient factors (Table 2)
-
Categorise the procedure into low, moderate or high risk of postoperative bleeding
-
For minor surgical procedures there is no need to discontinue the anticoagulant medication as the risk of thrombotic event outweighs the risk of post-operative haemorrhagic complications
-
If possible, perform the surgery as long as possible after the last dose
-
Consider local factors (such as inflammation of soft tissues)
-
Application of local haemostatic measures, including pressure application with gauze, use of gelatin sponge/oxidised-cellulose mesh (for example, Surgicel), suturing and the use of 5% tranexamic mouthwash four times daily for five days postoperatively (where available)
-
For intermediate surgical procedures (multiple extractions, surgical extractions) it is necessary to stop, miss a dose or delay the NOAC dose
-
For major surgical procedures (head and neck surgery, extensive oral and maxillofacial procedures), NOAC cessation is dependent on the patient's renal function and followed by discussion with the patient's physician/cardiologist (who may consider bridging anticoagulation). It may be necessary to ensure the effect of the drug is reduced by pre-operative aPTT or TT, which if still raised may require an increased period of drug cessation
-
Assessment of the risk of thromboembolic event, with high risk patients including any mitral valve prosthesis, stroke, cardio-embolic event, venous thromboembolism <3 months, severe thrombophilia or active cancer (diagnosed <6 months or undergoing treatment). Lower risk patients include aortic-valve prosthesis in patients without AF/prior to stroke, and venous thromboembolism >12 months (with no other risk factors).
Recommendations for practice
Limited data is available regarding the management of dental patients on NOACs, and remains a concern among clinicians. Further studies are encouraged to determine the true risks of bleeding after oral surgical procedures and to provide an evidence-based approach in their management.
Based on the findings of the articles appraised and pharmacological profiling of the drugs discussed, the following recommendations can be made (Table 4):
-
Ensure a detailed and current medical history is noted
-
Explain the risks and benefits of performing any dental treatment in patients on NOACs whether therapy is/is not continued
-
Assessment of surgical complexity (clinical and radiographic) that would suggest simple extraction (for example periodontally compromised teeth) versus surgical extraction (for example bulbous root morphology)
-
Appointments for extractions to be made in the morning and early in the week so that postoperative bleeding complications can be arrested before the weekend
-
Bleeding should be managed with local haemostatic measures in this group of patients, such as gelatin sponge/oxidised cellulose mesh, sutures and gauze pressure packs
-
Consider staged extractions for the control of intra-operative bleeding
-
Avoid the concomitant use of drugs that may interfere with peak plasma concentrations of NOACs (for example non-steroidal anti-inflammatories for pain control)
-
Discontinuation of NOACs is not necessary for uncomplicated/simple dental extractions and procedures (where the patient has normal renal function and there is only a standard bleeding risk)
-
In patients where there is a concern of increased intra-operative or postoperative bleeding, NOACs can be discontinued/dose delayed
-
Consider delay of any invasive dental procedures for patients on a time limited course of therapy, or in patients at the start of therapy (where initial doses may be higher)
-
For high risk surgical interventions, treatment should be delayed until discontinuation of the NOAC has been prepared and arranged accordingly with the patient's cardiologist, and based on their renal function (especially for general anaesthesia cases where staged extractions are not feasible)
-
Patients must be instructed on when to commence their NOAC therapy as part of the postoperative instruction
-
Severe postoperative bleeding can be managed with application of mechanical pressure, haemostatic measures, and maintenance of intravascular volume with fluid replacement (and consideration of haemodialysis in emergency situations). Where available reversal agents identified previously should be considered.
References
Neal M J . Medical Pharmacology at a Glance. 7th Edition. Wiley-Blackwell, 2012.
Pirmohamed M . Warfarin: almost 60 years old and still causing problems. Br J Clin Pharmacol 2006; 62: 509–511.
Bayer Schering Pharma AG. Xarelto: Summary of Product Characteristics. 2008.
Janssen Pharmaceutica. FDA Approves XARELTO® (rivaroxaban tablets) to Help Prevent Deep Vein Thrombosis in Patients Undergoing Knee or Hip Replacement Surgery (Press release). 2011.
U S. Food and Drug Association. FDA approves Xarelto to prevent stroke in people with common type of abnormal heart rhythm. 2011.
NICE. Rivaroxaban for the treatment of deep vein thrombosis and prevention of recurrent deep vein thrombosis and pulmonary embolism. Availlable online at http://www.nice.org.uk/guidance/TA261 (accessed March 2017).
Constandinides F, Rizzo R, Pascazio L, Maglione M . Managing patients taking novel oral anticoagulants (NOAs) in dentistry: a discussion paper on clinical implications. BMC Oral Health 2016; 16: 5.
Breik O, Cheng A, Sambrook P, Goss A . Protocol in managing oral surgical patients on dabigatran. Aust Dent J 2014; 59: 296–301.
Sabir, I, Khavandi, K, Brownrigg, J, Camm A J . Oral anticoagulants for Asian patients with atrial fibrillation. Nat Rev Cardiol 2014; 11: 290–303.
Lancashire Medicines Management Group. NHS England Guidance for prescribing of Dabigatran (Pradaxa) Rivaroxaban (Xarelto) and Apixaban (Eliquis) in Patients with Non-Valvular AF. 2015.
Curtin, C, Hayes J.M, Hayes S J . Dental Implications of New Oral Anticoagulants for Atrial Fibrillation. Dent Update 2014; 41: 526–531.
van Ryn J, Stangier J, Haertter S et al. Dabigatran etexilatea novel, reversible, oral direct thrombin inhibitor: interpretation of coagulation assays and reversal of anticoagulant activity. Thromb Haemost 2010; 103: 1116–1127.
Davis, C, Robertson, C, Shivakumar S . Implications of dabigatran, a direct thrombin inhibitor, for oral surgery practice. J Can Dent Assoc 2013; 79: 74.
Scottish Dental Clinical Effectiveness Programme. Management of Dental Patients Taking Anticoagulants or Antiplatelet Drugs. 2015. Available online at http://www.sdcep.org.uk/wp-content/uploads/2015/09/SDCEP-Anticoagulants-Quick-Reference-Guide.pdf (accessed March 2017).
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Nathwani, S., Wanis, C. Novel oral anticoagulants and exodontia: the evidence. Br Dent J 222, 623–628 (2017). https://doi.org/10.1038/sj.bdj.2017.364
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.364
This article is cited by
-
The Effect of Direct Oral Anticoagulant Therapy (DOACs) on oral surgical procedures: a systematic review
BMC Oral Health (2023)
-
Acquired bleeding disorders through antithrombotic therapy: the implications for dental practitioners
British Dental Journal (2020)
-
Characteristics, treatment and outcome of bleeding after tooth extraction in patients on DOAC and phenprocoumon compared to non-anticoagulated patients—a retrospective study of emergency department consultations
Clinical Oral Investigations (2019)