Abstract
Study design:
Clinical practice guidelines.
Objectives:
To develop the first Canadian clinical practice guidelines for treatment of neuropathic pain in people with spinal cord injury (SCI).
Setting:
The guidelines are relevant for inpatient and outpatient SCI rehabilitation settings in Canada.
Methods:
The CanPainSCI Working Group reviewed the evidence for different treatment options and achieved consensus. The Working Group then developed clinical considerations for each recommendation. Recommendations for research are also included.
Results:
Twelve recommendations were developed for the management of neuropathic pain after SCI. The recommendations address both pharmacologic and nonpharmacologic treatment modalities.
Conclusions:
An expert Working Group developed recommendations for the treatment of neuropathic pain after SCI that should be used to inform practice.
Similar content being viewed by others
Introduction
An international panel of experts—the CanPainSCI Working Group (WG)—was formed to develop the first Canadian clinical practice guideline (CPG) to inform the management of at- and below-level neuropathic pain (NP) in people with spinal cord injury (SCI) in an inpatient and outpatient rehabilitation setting. Using a consensus-based, modified Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach, recommendations have been made for three specific areas of management: screening and diagnosis; treatment; and model of care.1 This paper focuses on treatment of at- and below-level NP.
Treatment of neuropathic pain after spinal cord injury
SCI-related NP is a complex management challenge: frequently the long-term prognosis is poor, often worsening over time; NP can significantly impair functioning, increase disability and reduce quality of life; and it may be very difficult to achieve adequate pain control. In fact, only one-third of patients experience a 50% reduction in NP with treatment.2 As a result, the therapeutic goal for many patients with SCI-related NP is reducing pain severity sufficiently to support functional improvement.
Mechanisms operating at the spinal, peripheral and cerebral level may contribute to the development of post-SCI NP. Some experimental findings indicate that SCI-related NP may originate in the spinal cord near the site of damage and involve secondary changes in damaged nerve roots and brain structures.3 Excitotoxic and inflammatory processes that decrease inhibition and alter descending modulation may produce functional changes in surviving neurons and cortical and subcortical structures.4 Pharmacologic studies suggest that reducing membrane excitability and glutamate receptor activation (lidocaine and ketamine), increasing neuronal inhibition (baclofen and propofol) or blocking either sodium (lamotrigine) or calcium (pregabalin) channels involved in hyperexcitability may be effective for SCI-related NP.
Currently available treatment options, which target pathophysiologic changes at peripheral, spinal and cerebral levels, include both pharmacologic and nonpharmacologic approaches.3 Pharmacologic options include anticonvulsants, antidepressants and opioids. Nonpharmacologic approaches, which encompass stimulation techniques, surgery and psychological management, may differ according to the type of pain and the level of injury.
Within the emerging field of SCI-related NP, studies on pharmacologic treatment options dominate the literature.5, 6 There is guidance in the form of outcome measures,2 assessment and treatment algorithms,2, 7, 8 guidelines9, 10, 11, 12 and consensus statements.13 However, previous guidelines on this topic are either not specific to SCI-related NP or have not been conceptualized using the Appraisal of Guidelines for Research and Evaluation (AGREE) methodology.
Primary objective
The aim of the CanPainSCI WG was to develop recommendations to help rehabilitation health-care providers make decisions about the treatment of SCI-related NP.
Materials and methods
As previously described, the Steering Committee (SC) conducted a specific literature review based on treatment options for NP. If conflicting evidence for a specific treatment option was found, then the SC performed a meta-analysis in an effort to resolve the conflict (this was the case for amitriptyline) and used the GRADE process to evaluate the literature and rate the quality of the evidence (Supplementary File 1).1 Unique among most CPGs and recommendations for the management of NP, the current guideline addresses both pharmacologic and nonpharmacologic therapies within lines of treatment.
The Treatment Working Group (TWG) was formed using a previously described methodology. The panel reviewed the analysis and evidence rating for each therapy and proposed recommendations, which were refined through subsequent meetings until the panel achieved consensus. The expert panel assigned a strength of recommendation (strong or weak) in accordance with the GRADE process. The strength of a recommendation was based on numerous factors including clinical experience, side-effect profile, effectiveness in other neuropathic pain populations and any other factors that the panel considered relevant. The draft recommendations were then presented to the entire CanPainSCI WG for review and discussion. Each recommendation was accompanied by relevant clinical considerations and rationale where needed. Using the previously described methodology, the CanPainSCI WG discussed and voted on the final recommendations during a face-to-face meeting. Only those recommendations receiving at least 75% agreement were adopted and are included here.
The CanPainSCI WG assigned therapies to first-, second- third- or fourth-line use based on the assessment of evidence using the GRADE process.1 The WG made specific modifications to this process in accordance with GRADE. First, in the presence of multiple study types for a particular treatment, the WG deferred to the highest-quality study design, such as randomized controlled trials (RCTs), to rate quality. Second, the size of the study population was not used to downgrade evidence quality, as study populations in the included studies were generally small compared with study populations in more prevalent (that is, non-SCI) conditions. Third, studies were not downgraded in cases where studies were funded by pharmaceutical companies, as these studies are among the very few multicenter RCTs for any treatment modality in SCI-related NP. In addition, the WG decided that accessibility of a treatment option would not affect recommendation formation.
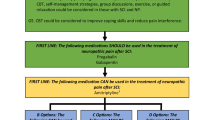
Recommendation of a treatment as first-line therapy required high-quality evidence and a strong recommendation. A second-line recommendation required high- or moderate-quality evidence and a strong recommendation. A third-line recommendation required high- or moderate-quality evidence and a weak recommendation. Assignment of a therapy to fourth-line use was based on moderate- or low-quality evidence and a weak recommendation. Criteria for the ranking of high, moderate, low and very low evidence were in accordance with the modified GRADE process described previously.1 Recommendations advising against the use of particular therapies were also developed.
For a number of treatment options, the TWG felt that further research was required before a recommendation could be made. These include certain treatments with low quality evidence, treatments with demonstrated efficacy in other populations with NP and treatments with conflicting evidence in the literature.
Results
The consensus process resulted in recommendations for 10 treatments. The CanPainSCI WG advised against the use of two therapies and recommended several treatment approaches for additional research before implementation.
Several principles guided the development of recommendations. First, the main outcome of interest is pain intensity, and all evidence supporting the recommendations includes the data on the effect of the treatment strategy on pain intensity. Second, the CanPainSCI WG recommends that combination therapy be used, when necessary, to maximize the reduction in NP intensity and that complementary or supplementary therapies be used to optimize overall patient management. One such important complementary therapy is cognitive behavioral therapy, which, although not demonstrating an effect on pain intensity, significantly affects mood, disability, patient global impression of change and health-related quality of life.14 Third, it is essential that patients with SCI-related NP receive education to increase their level of knowledge about NP and skills needed to better self-manage NP and to reduce their fear.15 Fourth, it is critical for clinicians to assess and monitor the effects of all therapies on a regular basis to maximize patient outcomes.
First-line therapy
Recommendation 2.1
Pregabalin should be used for the reduction of neuropathic pain intensity among people with SCI.
Quality of evidence: High.
Strength of recommendation: Strong.
Clinical considerations
Pregabalin is recommended as the first choice of first-line medications, as it has the strongest evidence of any treatment modality in below-level NP: all studies demonstrate a significant reduction in pain intensity. Pregabalin studies used larger sample sizes than most treatment studies for SCI-related NP and utilized rigorous methodology. Two high-quality placebo-controlled RCTs and one moderate-quality placebo-controlled RCT, which was downgraded based on wide confidence intervals around numbers needed to treat, comprise the evidence base for pregabalin.17, 18, 19 All studies focused on NP and measured pain intensity. One trial studied a mixed population that included stroke patients (N=19), but a subgroup analysis was performed for the group with SCI.19 It is noted that a pharmaceutical company funded two of the pregabalin RCTs.17, 18
Pregabalin studies used flexible dosing between 150 and 600 mg per day. The main adverse effects were somnolence and dizziness, which were usually of mild-to-moderate intensity and transient.17, 18
Recommendation 2.2
Gabapentin should be used for the reduction of neuropathic pain intensity among people with SCI.
Quality of evidence: High.
Strength of recommendation: Strong.
Clinical considerations
Gabapentin is recommended as the next choice when pregabalin is not an option or has been proven ineffective, as the evidence supporting gabapentin in SCI-related NP is not as strong as that for pregabalin. The body of evidence for gabapentin in SCI-related NP contains three randomized trials, two of which found no significant difference between gabapentin and placebo,20, 21 although one trial21 found a trend toward pain intensity reduction with gabapentin (N=7). The third found gabapentin significantly reduced NP.22 Two observational case series included only patients with SCI-related NP. One found a reduction in NP intensity,23 and the other found a reduction in general pain intensity.24 An observational study of gabapentin in patients with SCI and different durations of symptoms, which included patients with cauda equina, found a significant reduction in the mean pain intensity score after treatment with gabapentin.25
Although the outcomes of reviewed studies were conflicting, a meta-analysis performed as part of the data review indicated benefit. In addition, other CPGs for the management of central or peripheral NP consider both pregabalin and gabapentin as first-line therapy. Although other NP CPGs consider pregabalin and gabapentin interchangeable, further study is required to establish this within the SCI-related NP population.
Maximum gabapentin doses in clinical trials ranged from 1800 to 3600 mg per day, and the major adverse events were dizziness and somnolence.20, 21, 22
Recommendation 2.3
Amitriptyline can be used for the reduction of neuropathic pain intensity among people with SCI.
Quality of evidence: High.
Strength of recommendation: Strong.
Clinical considerations
If pregabalin and gabapentin have been ineffective, then amitriptyline is recommended; less evidence exists for the efficacy of amitriptyline than for the gabapentinoids.
A meta-analysis of four antidepressant RCTs for the management of SCI-related NP found that these agents were effective in reducing neuropathic pain.5 Two RCTs that studied amitriptyline had conflicting results.20, 26 One small study of patients with NP (N=22) found amitriptyline more effective than active control (diphenhydramine) and gabapentin.20 This study also found that NP was more likely to improve in patients with depressive symptoms. The second study of patients with NP (n=51) and musculoskeletal pain (n=33) found no significant difference between amitriptyline and control (benzotropine mesylate).26
Tricyclic antidepressants are typically used to treat NP at a dose of 25 to 150 mg per day.27 Treatment is usually initiated at 10 to 25 mg daily. In the Rintala study, which demonstrated amitriptyline efficacy in the treatment of SCI-related NP, nearly all participants reached the target dose of 50 mg TID;20 these findings suggest that lower doses may be less effective. Adverse effects of tricyclic antidepressants include anticholinergic side effects, which mandate caution in the SCI population, sedation, cardiotoxicity and a reduced seizure threshold. Within other pain populations, secondary amine tricyclic antidepressants (nortriptyline and desipramine) tend to have similar efficacy but better tolerability than tertiary amines (amitriptyline and imipramine). There is a lack of evidence specific to patients with SCI-related NP for both secondary and tertiary amine tricyclic antidepressants.
Second-line therapy
Recommendation 2.4
Tramadol can be used for the reduction of neuropathic pain intensity among people with SCI.
Quality of evidence: Moderate.
Strength of recommendation: Strong.
Clinical considerations
Tramadol is recommended as second-line therapy for SCI-related NP. A single randomized, placebo-controlled trial found a significant reduction in pain intensity with tramadol compared with placebo, but the evidence quality was downgraded because of wide confidence intervals.28 The Canadian Guideline for Safe and Effective Use of Opioids for Chronic Non-Cancer Pain is a useful resource for general information on opioid management and prescription considerations.29 Although tramadol is not a scheduled drug in Canada, in the United States it is a Schedule IV drug.
The maximum daily dosage of tramadol is 400 mg, divided into up to four daily doses.27 Treatment is usually initiated at 50 mg QD or BID and titrated, based on efficacy and tolerability. Common adverse effects are sedation, nausea and constipation. Twelve out of thirteen participants in the Norrbrink and Lundeberg28 trial withdrew because of adverse medication events. A slight increase in the risk of serotonin syndrome can be seen when tramadol is combined with other monoaminergic drugs such as tricyclic antidepressants.
Recommendation 2.5
Lamotrigine may be considered in those with incomplete SCI for the reduction of neuropathic pain intensity.
Quality of evidence: Moderate.
Strength of recommendation: Strong.
Clinical considerations
Evidence for the efficacy of lamotrigine has been demonstrated only in patients with incomplete SCI. As a result, lamotrigine is recommended as second-line therapy only in this population. One randomized placebo-controlled trial showed that lamotrigine significantly reduced the intensity of NP for patients with incomplete SCI, but the evidence quality was downgraded because of wide confidence intervals.30
Lamotrigine dosage was titrated to a maximum of 400 mg per day.30 Common adverse effects were dizziness, somnolence, headache and rash. It should be noted that lamotrigine has a black box warning issued by the United States Food and Drug Administration (FDA) for serious skin rashes, including Stevens-Johnson Syndrome.
Third-line therapy
Recommendation 2.6
Transcranial direct current stimulation (tDCS) may be considered for reducing neuropathic pain intensity among people with SCI.
Quality of evidence: High
Strength of recommendation: Weak
Clinical considerations
Transcranial direct current stimulation (tDCS) is recommended as third-line therapy for patients with SCI-related NP on the basis of four RCTs focused on NP in patients with SCI. Three studies found a significant reduction in pain intensity with tDCS compared with sham control.31, 32, 33 One of these studies found a significant improvement in continuous pain on the last day of treatment, and paroxysmal pain at follow-up, but no significant reduction in overall pain intensity.33 A fourth study did not find a significant difference between tDCS and sham control.34 A prospective-controlled trial that found a significant reduction in pain intensity, compared with sham control, was upgraded because of small confidence intervals and the inclusion of an intention-to-treat analysis.35 A meta-analysis of the five studies found a positive effect for transcranial direct current stimulation on pain intensity.36 tDCS was given a weak strength of recommendation, as the panel felt that it was more appropriate to trial pharmacological therapies first, in accordance with other neuropathic pain management guidelines and extensive clinical experience with those treatments in neuropathic pain secondary to various etiologies.
Minor side effects of tDCS include skin irritation, which can be minimized by preparing electrodes with saline and the skin with electrode cream and by increasing current gradually, and phosphene, the visual perception of a brief flash of light, which is not actually present, if an electrode is placed near the eye.
Recommendation 2.7
Combined visual illusion and transcranial direct current stimulation may be considered for reducing neuropathic pain intensity among people with SCI.
Quality of evidence: High.
Strength of recommendation: Weak.
Clinical considerations
The combination of visual illusion and tDCS is recommended as third-line therapy. An RCT in SCI-related NP found a significant reduction in pain intensity after treatment compared with control illusion, visual illusion in isolation and tDCS in isolation.33 An observational study of a cohort that included individuals with neuropathic and other types of pain found a nonsignificant improvement in pain intensity after treatment.37
The main side effects of this combined therapy included mild headache and fatigue.33
Fourth-line therapy
Therapies recommended for fourth-line use can be considered in patients with pain that is refractory to earlier lines of therapy.
Recommendation 2.8
Transcutaneous electrical nerve stimulation (TENS) may be considered for the reduction of neuropathic pain intensity among people with SCI.
Quality of evidence: Low.
Strength of recommendation: Weak.
Clinical considerations
Two prospective-controlled observational studies have been performed evaluating the effect of TENS in patients with SCI-related NP.38, 39 One trial found no significant difference between high-frequency and low-frequency TENS.38 The second trial found a significant effect of low-frequency TENS on pain intensity reduction, and the quality of evidence was upgraded because the study included a control group and randomized the participants.39 An early (1975) observational case series found a pain intensity reduction with TENS for two of 11 patients.39 The evidence quality of this study was downgraded because of a lack of confidence intervals and description of methods, and a potential for bias.
It is important to consider the short duration of action for relief of pain with TENS when contemplating the use of this modality. In addition, lack of long-term follow-up precludes any discussion of the prolonged efficacy of TENS. Few side effects are associated with TENS, but patients have reported increased pain intensity and muscle spasm.38 The WG did not include TENS among the therapies without specific recommendations because of a lack of long-term follow-up, as the relatively innocuous side effects of TENS make this therapy more appropriate for a therapeutic trial in refractory cases.
An additional consideration is electrode placement. Little evidence suggests the utility of TENS when electrodes are placed in insensate areas. Recent trials have used placement of electrodes at the level of injury in an area with preserved or intact sensibility.38, 39
Recommendation 2.9
Oxycodone can be used for the reduction of neuropathic pain intensity among people with SCI.
Quality of evidence: Moderate.
Strength of recommendation: Weak.
Clinical considerations
Oxycodone is an oral opioid that has been assessed in SCI-related NP. One observational study, which showed a significant reduction in pain intensity after 3 months of treatment, had its quality of evidence upgraded because confidence intervals were provided and only patients with NP were included.40
Long-term opioid use exposes people to unique risks including possible problems with drug tolerance and dose escalation, opioid-induced hyperalgesia, endocrinopathy and potential for misuse and developing physical dependence, in addition to common side effects such as constipation, which is more problematic in people with SCI.41 Typical opioid adverse effects include sedation, nausea, vomiting and dry mouth.29 Oxycodone is ~1.5 times as potent as morphine. The potential adverse effects and issues associated with oxycodone, and opioids in general, led the panel to assign a weak strength of recommendation. The panel recommends additional research into the use of opioids as a class in patients with SCI-related NP. It is likely reasonable to use opioids other than oxycodone, and the Canadian Guideline for Safe and Effective Use of Opioids for Chronic Non-Cancer Pain should be used to guide the use of medications in this class.29
Recommendation 2.10
The dorsal root entry zone (DREZ) procedure may be considered in exceptional circumstances and as a last resort for reducing neuropathic pain intensity among people with SCI.
Quality of evidence: Low.
Strength of recommendation: Weak.
Clinical considerations
Evidence of benefit for the DREZ procedure exists, but the risk of the procedure does not justify its use beyond exceptional circumstances. The available evidence supporting the DREZ procedure is based on observational studies or case series in SCI-only populations,42, 43, 44, 45, 46 and one study included patients with cauda equina.44 A prospective-controlled observational trial found a reduction in pain intensity with the DREZ procedure and greater efficacy in below-level pain.42 An observational study found a reduction in pain intensity after the DREZ procedure.44 Three observational case series found that the DREZ procedure reduced pain intensity.44, 45, 46
Risks associated with the DREZ procedure include paresis, neuropathy or radiculopathy, ataxia and a variety of surgical complications such as persistent incisional site pain, cerebrospinal fluid leak, wound infection, subcutaneous hematoma and bacteremia.43, 46
Advise against use
The studies for these treatment options demonstrated no effect or benefit in the SCI population, and their use is therefore not advised.
Recommendation 2.11
Levetiracetam should not be used for reducing neuropathic pain intensity among people with SCI.
Quality of evidence: High.
Strength of recommendation: Strong.
Clinical considerations
A prospective RCT performed in a population with SCI-related NP comparing levetiracetam with placebo found no significant difference between the two treatments.47
Recommendation 2.12
Mexiletine should not be used for reducing neuropathic pain intensity among people with SCI.
Quality of evidence: High.
Strength of recommendation: Strong.
Clinical considerations
A prospective, placebo-controlled RCT in a population of patients with SCI-related NP found that mexiletine was not significantly more effective than placebo in reducing pain intensity.48
Therapies requiring further research
It should be strongly emphasized that the overall body of evidence for the management of at- and below-level NP is inadequate. This includes the evidence that has been used to support recommendations put forward by our group. This issue is not unique to SCI but seems to be the case in other central NP conditions as well. Often, general NP CPGs recommend that the treatment of central NP utilize the same recommendations as those for peripheral NP, with the exception of certain situations where strong evidence exists.
Multicenter RCTs in patients with SCI-related NP are recommended for all treatments in this guideline, including first-line treatments, to generate adequate sample sizes and sufficient power to determine effectiveness conclusively. Top research priorities include gabapentinoids, tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors and cannabinoids.
The WG was unable to make specific recommendations about the management strategies discussed in the following section, because of insufficient evidence for benefit, studies with conflicting results and insufficient data to perform meta-analyses, or low-quality studies with negative results. This section also reviews treatments that have demonstrated efficacy in other NP conditions but have limited evidence within SCI populations. Additional research into the treatments within this section would be useful, as these therapies may have a benefit that is as yet unclear.
1) Treatments with low-quality evidence of positive effect
Several treatments evaluated by the SC had low-quality evidence of a positive effect in reducing SCI-related NP intensity, including exercise, spinal cord stimulation, hypnotic suggestion, massage, osteopathy and transcranial magnetic stimulation.
Exercise
One RCT of pain in patients with SCI found a reduction in the pain perception score in the treatment group compared with the control group after 3 months (F (1, 27)=4.99, P=0.03).49 However, the evidence quality of the study was downgraded because of the following : an unclear protocol; lack of specification of the type of pain, blinding, confidence intervals and power calculation; and potential bias of control participants.
Spinal cord stimulation
A case series with a mixed pain population of patients with SCI presented no statistically significant data on pain intensity reduction.50
Hypnotic suggestion
An RCT found a reduction in intensity of SCI-related NP after treatment (P<0.01), but the evidence quality was downgraded because of a lack of confidence intervals.51
Massage
A prospective-controlled trial, which included a comparison between acupuncture and massage, found that massage did not produce a significant reduction compared with acupuncture in SCI-related NP intensity.52 No evidence was found on efficacy of massage on its own.
Osteopathy
An RCT found a 16% reduction in the perception of SCI-related NP during treatment but not at later time points.53 No significance was reported for this result, and the evidence quality of this study was downgraded because of a lack of randomization process description, blinding and confidence intervals.
Transcranial magnetic stimulation
Three RCTs in SCI-related NP compared the effect of transcranial magnetic stimulation with sham therapy.54, 55, 56 Two of these trials found no significant difference in reduction in pain intensity.54, 55 The evidence quality of the third trial, which found a significant improvement in pain intensity after treatment, was downgraded because of wide confidence intervals.56
2) Treatments with evidence of positive effect in populations other than SCI
The SC evaluated several therapies with evidence of pain reduction in non-SCI populations, including cannabinoids, duloxetine and intrathecal clonidine.
Cannabinoids
With widespread media attention on cannabinoids as a treatment for refractory chronic pain and more liberalized access to these agents in Canada, patients frequently request them. Although cannabinoids appear to be beneficial in multiple sclerosis, evidence in SCI is lacking. There is insufficient evidence at this stage to recommend the use of cannabinoids for the treatment of SCI-related pain, but more information is urgently needed to guide their use in patients with SCI.
One RCT that compared dronabinol and active control (diphenhydramine) found no significant difference in seven patients with SCI-related NP, and the evidence quality of the study was downgraded because of wide confidence intervals.57
The most common adverse effects seen in the study were dry mouth, constipation, fatigue and drowsiness.57 Oral dronabinol has been studied in multiple sclerosis at a maximum dose of 10 mg daily.58 The panel strongly recommends additional research into the effects of cannabinoids in patients with SCI-related NP, especially on long-term efficacy and adverse effects, as a top research priority.
Duloxetine
One RCT showed no significant difference in reduction in intensity of NP between duloxetine and placebo in patients with SCI or stroke, although a trend was seen toward a decrease in the mean pain score with duloxetine, demonstrating the potential for benefit.59 A good evidence base exists for the effectiveness of duloxetine in treating peripheral NP in other populations.60 The CPG for the prevention and management of diabetes recommends duloxetine as an option for the treatment of NP in this population.61
Doses of 60 and 120 mg appear to be effective in reducing the intensity of peripheral NP. Typical side effects include nausea, clinically insignificant increases in blood pressure and, rarely, hepatotoxicity.27
3) Treatments lacking evidence of long-term effect or follow-up
The SC evaluated several invasive therapies that lacked evidence of long-term effect or follow-up, including intravenous lidocaine, intravenous alfentanil, intrathecal clonidine plus morphine, intravenous morphine and intravenous ketamine. As studies of these treatments in patients with SCI-related NP that are described below included no long-term follow-up, their effectiveness beyond the time during which they were administered is undefined. Although the initial proof-of-concept studies have been completed, follow-up studies are recommended before these therapies are implemented in patients with SCI-related NP. The exception to this is TENS, which also lacks long-term follow-up, but its relatively innocuous side-effect profile resulted in TENS being recommended for fourth-line use.
Intravenous lidocaine
Intravenous lidocaine has demonstrated benefit in three well-conducted RCTs of SCI-related NP.62, 63, 64 One trial also included patients with stroke.63 Two of the studies found a significant reduction in pain intensity with intravenous lidocaine compared with placebo,62, 63 whereas the third found no significant difference.64 The evidence quality of one study was downgraded because of a lack of power calculation and an unclear protocol,64 and another was downgraded because of a lack of explanation of the randomization process and large confidence intervals.62 The studies with a positive result used lidocaine 5 mg kg−1 over 30 min,62, 63 whereas the study with a negative result used lidocaine 2.5 mg kg−1 over 40 min.64 Light-headedness was a common adverse effect. As the duration of benefit for intravenous lidocaine is very short, this treatment modality should only be considered in specific circumstances where a short duration of effect is desired.
Intravenous alfentanil
A single double-blind cross-over study of nine patients with central dysesthetic pain after SCI evaluated alfentanil and ketamine compared with placebo (normal saline).66 Alfentanil significantly reduced the intensity of continuous pain compared with placebo (P=0.01), allodynia compared with placebo and wind-up-like pain compared with placebo. As the response of continuous pain to therapy was only measured before and after the infusion, the duration of response is uncertain. The intravenous mode of administration of alfentanil makes this therapy a short-term management option with a short duration of effect.
Intrathecal clonidine
One RCT that compared intrathecal clonidine with placebo (saline) found no statistically significant difference in reduction of pain intensity in patients with SCI-related pain, and the evidence quality of the study was downgraded because of a lack of description of the randomization process or patient allocation.66
Intrathecal clonidine and morphine
One double-blind cross-over study of 15 patients that compared intrathecal administration of clonidine, morphine, clonidine plus morphine and saline (placebo) found a significant reduction in pain intensity only for the combination of intrathecal morphine and clonidine compared with placebo (P=0.0084).66 Two of 4 patients with at-level pain and 5 of 14 patients with below-level pain responded to the combination, but no significant difference was found between the groups. As a significant correlation was seen between pain relief and drug concentrations in the cervical cerebrospinal fluid, consideration should be given to administering the agents above the level of injury to ensure adequate penetration of cervical cerebrospinal fluid. The duration of response is uncertain but is assumed to be <24 h, as patients were crossed over to the next therapy the following day.
Intravenous morphine
One small, double-blind, placebo-controlled, cross-over study of intravenous morphine in patients with SCI- or stroke-related NP found no significant difference in spontaneous pain between placebo and intravenous morphine but a 90-min post-injection reduction in allodynia with morphine.67 The evidence quality of the study was downgraded because of the lack of power calculation. All patients subsequently received oral sustained-release morphine, but the titration schedule was not well defined, and the study used haloperidol, an uncommon treatment for opioid-induced nausea. Overall, the results of this study were inconclusive for a benefit of intravenous morphine.
Intravenous ketamine
Two RCTs of intravenous ketamine in SCI-related NP found a significant reduction in pain intensity.64, 65 The evidence quality of one study was downgraded because of the absence of a power calculation and an unclear protocol.64 The second study, a double-blind cross-over study of nine patients with central dysesthetic pain after SCI, evaluated ketamine and alfentanil compared with placebo (normal saline).65 Ketamine significantly reduced the intensity of continuous pain and allodynia compared with placebo. As the treatment response was only measured before and after infusion, the duration of response is uncertain.
Visual illusion
One RCT in patients with SCI-related NP found a significant reduction in overall pain intensity compared with a control illusion on the last day of treatment, but this change did not persist and was not evaluated at follow-up.33 An observational study that found an insignificant reduction in pain intensity with the intervention was downgraded because of a lack of information on sequence generation, wide confidence intervals and a very small sample size (N=5).68 Another observational study found a significant increase in pain intensity after treatment in comparison with a control illusion.69
4) Treatments with conflicting evidence for reduction in neuropathic pain intensity
The SC evaluated one therapy, acupuncture, with conflicting evidence of benefit for reduction in the intensity of SCI-related NP. Meta-analysis was not possible because of the absence of comparable data between studies.
Acupuncture
One study showed no significant effect on chronic pain intensity in patients with SCI-related pain or chronic musculoskeletal pain; nonresponders were all from the central pain population.70 In another study, 8 of 15 patients with SCI-related NP responded to acupuncture.52 A retrospective observational case series of patients with traumatic or nontraumatic SCI found a significant improvement in pain for bilateral, for bilateral, symmetric, burning or constant pain compared with unilateral, asymmetric, atypical or intermittent pain.71 Studies of acupuncture suffer from a lack of standardization of process or procedure delivery and practice principles, and evidence for effectiveness is inconclusive. Additional studies are needed to clarify the benefit of using this modality.
Discussion
Whereas the majority of CPGs on treatment of NP generally focus on pharmacologic management, this guideline is the first to include both pharmacologic and nonpharmacologic treatments. The evaluation of both pharmacologic and nonpharmacologic therapies was undertaken to assess all available treatment options for this difficult-to-manage condition. When possible, we advocate the use of combination therapy, whether a combination of medications or pharmacologic and nonpharmacologic strategies.
An important benefit of this guideline is that it provides a sequential approach to the management of NP that is specific to the SCI population, with recommendations that are based solely on evidence within the SCI literature. Previous CPGs on NP management have generally evaluated management of SCI-related NP within the umbrella of central NP of any pathology, with rare exceptions for certain treatments in specific conditions, such as cannabinoids for multiple sclerosis. In general, recommendations for central NP refer to peripheral NP guidelines, an approach that assumes that the pathology of SCI-related NP is similar to other central pain conditions and that central NP conditions are similar to peripheral NP conditions. This CPG is unique in that the SCI literature was the sole reference for recommendation development. Although this inherently limited the available evidence, assessing the literature specific to the SCI population was felt to be critical, not only to evaluate the effects of different treatments on reduction in SCI-related NP but also to consider unique issues within the SCI population that may not apply to other pain populations. An example of this is the anticholinergic effect of tricyclic antidepressants on bladder and bowel function, which is vitally important to the quality of life of a patient with SCI. Despite the reliance on the SCI literature for this CPG, however, the line of treatment recommended for pharmacological agents is similar to other NP guidelines and algorithms (Table 1).
In terms of implementation, this CPG may be used to guide and provide context for future work related to NP after SCI. The ranked nature of these recommendations could be used to inform the development of clinical algorithms. In addition, the CPG can provide direction for further exploration of treatments that have an emerging evidence base but limited use in clinical practice. tDCS and visual illusion are examples of this, and further confirmation of the benefit of these modalities for management of SCI-related NP should be pursued. Clinical experience with these modalities, particularly tDCS, is generally limited and may be reflected in the strength of recommendations presented in this guideline.
It is crucially important to recognize the limited evidence on which these recommendations as a whole are based. Limitations in the evaluated evidence include the use of mixed patient populations and SCI pain types, a lack of RCTs, small sample sizes and potential lack of power. Modified GRADE criteria were therefore used when evaluating studies. This approach, although it reduced the ability of our methodology to evaluate study bias, is permissible in guideline development, particularly where a majority of studies have a similar limitation such as small study populations. This modification was made to allow interpretation of the available evidence within management of SCI-related NP. As a result, it was possible to generate recommendations for clinicians that were developed with an emphasis on maximizing potential benefit and minimizing potential harm to their patients. Clinicians and others using this guideline should be aware of its inherent limitations, however.
The lack of evidence for benefit of many therapies significantly hampers clinicians’ ability to deliver optimal care to all patients. Research is therefore urgently needed on all the therapies in this guideline to better guide appropriate clinical use. The CanPainSCI WG recommends additional research into gabapentin, amitriptyline, opioids, cannabinoids, selective serotonin and norepinephrine reuptake inhibitors, and topical agents for at-level discrete pain as top research priorities.
In addition, the lack of subgroup analysis in most studies hampers determination of benefit for specific patient types. Subgroup features that may have relevance for treatment response include pain subtype, level or severity of SCI, duration of pain or SCI and the presence of depressive symptoms. It is important for future studies to include appropriate subgroup analyses. The planning process for future research should ensure that outcomes can be compared and the data pooled to facilitate analysis of the evidence. The use of a basic set of standard outcome measures, specifically the ISCIPBDS, may help with this consideration.
Implementation of the ambitious research program recommended here requires administrative and policy changes, allocation of substantial resources and strong advocacy efforts with government and funding agencies by the SCI community. Procurement of research funding is a critically important issue for evaluation of treatments for SCI-related NP, and pharmaceutical company funding is a double-edged sword, as the funding source could potentially bias the evidence. For example, pharmaceutical funding resulted in two large RCTs for pregabalin,17, 18 which generated the evidence for use on which pregabalin has been recommended as the first choice of first-line agents. Furthermore, it is a concern that although additional research into the benefits of amitriptyline is needed, it is now available in generic form, and research funding may be difficult to obtain. Research funding concerns extend to other generic drugs and nonpharmacologic therapies, all of which require additional research to provide adequate evidence for use.
Conclusion
The objective of developing these guidelines was to create an evidence-based approach for treatment of SCI-related NP that could act as a resource to guide care delivery in the rehabilitation setting. These guidelines provide a sequential and a ranked approach to the management of SCI-related NP based solely on the SCI literature. The greatest limitation of these guidelines is the lack of evidence for most treatments. However, the guideline development process has identified an important opportunity to address the limitations of the evidence in the SCI population. As a result, this guideline includes numerous research recommendations. The WG will update these guidelines as additional evidence becomes available.
References
Schünemann H, Brożek J, Guyatt G, Oxman A (eds). GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Updated October 2013. The GRADE Working Group, 2013. Available at http://gdt.guidelinedevelopment.org/central_prod/_design/client/handbook/handbook.html (accessed on 13 July 2015).
Siddall PJ, Middleton JW . Pain following spinal cord injury. In: Chhabra HS (ed.). ISCoS Textbook on Comprehensive Management of Spinal Cord Injuries. Wolters Kluwer: Gurgaon, India. 2015, pp 825–848.
Siddall PJ . Management of neuropathic pain following spinal cord injury: now and in the future. Spinal Cord 2009; 47: 352–359.
Yezierski RP . Spinal cord injury pain: spinal and supraspinal mechanisms. J Rehabil Res Dev 2009; 46: 95–107.
Mehta S, Guy S, Lam T, Teasell R, Loh E . Antidepressants are effective in decreasing neuropathic pain after SCI: a meta-analysis. Top Spinal Cord Inj Rehabil 2015; 21: 166–173.
Guy S, Mehta S, Teasell R, Loh E . Anticonvulsant medication use for the management of pain following spinal cord injury: systematic review and effectiveness analysis. Spinal Cord 2014; 52: 89–96.
Siddall PJ, Middleton JW . A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord 2006; 44: 67–77.
Craven C, Verrier M, Balioussis C, Wolfe D, Hsieh J, Noonan V et al. Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian SCI Rehabilitation. Rick Hansen Institute: Toronto, ON. 2012.
Dworkin RH, O’Connor AB, Kent J, Mackey SC, Raja SN, Stacey BR et al. Interventional management of neuropathic pain: NeuPSIG recommendations. Pain 2013; 154: 2249–2261.
Attal N, Cruccu G, Baron R, Haanpää M, Hansson P, Jensen TS et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol 2010; 17: 1113-e88.
MASCIP Multidisciplinary Association of Spinal Cord Injury Professionals Guidelines for the Management of Neuropathic Pain in Adults following Spinal Cord Injury 2nd edn 2008 Available at http://www.mascip.co.uk/guidelines.aspx (accessed on 20 August 2014).
Perrouin-Verbe B, Ventura M, Albert T, Souan P, Fattal C, Revel M . Clinical practice guidelines for chronic neuropathic pain in the spinal cord injury patient: introduction and methodology. Ann Phys Rehabil Med 2009; 52: 77–82.
Moulin DE, Boulanger A, Clark AJ, Clarke H, Dao T, Finley GA et al. Pharmacological management of chronic neuropathic pain: revised consensus statement from the Canadian Pain Society. Pain Res Manag 2014; 19: 328–335.
Heutink M, Post MWM, Bongers-Janssen HMH, Dijkstra CA, Snoek GJ, Spijkerman DCM et al. The CONECSI trial: results of a randomized controlled trial of a multidisciplinary cognitive behavioral program for coping with chronic neuropathic pain after spinal cord injury. Pain 2012; 153: 120–128.
Burns AS, Delparte JJ, Ballantyne EC, Boschen KA . Evaluation of an interdisciplinary program for chronic pain after spinal cord injury. PM&R 2013; 5: 832–838.
Louw A, Diener I, Butler DS, Puentedura EJ . The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch Phys Med Rehabil 2011; 92: 2041–2056.
Cardenas DD, Nieshoff EC, Suda K, Goto S, Sanin L, Kaneko T et al. A randomized trial of pregabalin in patients with neuropathic pain due to spinal cord injury. Neurology 2013; 80: 533–539.
Siddall PJ, Cousins MJ, Otte A, Griesing T, Chambers R, Murphy TK . Pregabalin in central neuropathic pain associated with spinal cord injury: a placebo-controlled trial. Neurology 2006; 67: 1792–1800.
Vranken JH, Dijkgraaf MG, Kruis MR, van der Vegt MH, Hollmann MW, Heesen M . Pregabalin in patients with central neuropathic pain: a randomized, double-blind, placebo-controlled trial of a flexible-dose regimen. Pain 2008; 136: 150–157.
Rintala DH, Holmes SA, Courtade D, Fiess RN, Tastard LV, Loubser PG . Comparison of the effectiveness of amitriptyline and gabapentin on chronic neuropathic pain in persons with spinal cord injury. Arch Phys Med Rehabil 2007; 88: 1547–1560.
Tai Q, Kirshblum S, Chen B, Millis S, Johnston M, DeLisa JA . Gabapentin in the treatment of neuropathic pain after spinal cord injury: a prospective, randomized, double-blind, crossover trial. J Spinal Cord Med 2002; 25: 100–105.
Levendoglu F, Ogün CO, Ozerbil O, Ogün TC, Ugurlu H . Gabapentin is a first line drug for the treatment of neuropathic pain in spinal cord injury. Spine (Phila Pa 1976) 2004; 29: 743–751.
To TP, Lim TC, Hill ST, Frauman AG, Cooper N, Kirsa SW et al. Gabapentin for neuropathic pain following spinal cord injury. Spinal Cord 2002; 40: 282–285.
Putzke JD, Richards JS, Kezar L, Hicken BL, Ness TJ . Long-term use of gabapentin for treatment of pain after traumatic spinal cord injury. Clin J Pain 2002; 18: 116–121.
Ahn SH, Park HW, Lee BS, Moon HW, Jang SH, Sakong J et al. Gabapentin effect on neuropathic pain compared among patients with spinal cord injury and different durations of symptoms. Spine (Phila Pa 1976) 2003; 28: 341–346.
Cardenas DD, Warms CA, Turner JA, Marshall H, Brooke MM, Loeser JD . Efficacy of amitriptyline for relief of pain in spinal cord injury: results of a randomized controlled trial. Pain 2002; 96: 365–367.
Jefferies K . Treatment of neuropathic pain. Semin Neurol 2010; 30: 425–432.
Norrbrink C, Lundeberg T . Tramadol in neuropathic pain after spinal cord injury. A randomized, double-blind, placebo-controlled trial. Clin J Pain 2009; 25: 177–184.
Canadian Guideline for Safe and Effective Use of Opioids for Chronic Non-Cancer Pain. Canada: National Opioid Use Guideline Group (NOUGG), 2010. Available at http://nationalpaincentre.mcmaster.ca/opioid/ (accessed on 13 July 2015).
Finnerup NB, Sindrup SH, Bach FW, Johannesen IL, Jensen TS . Lamotrigine in spinal cord injury pain: a randomized controlled trial. Pain 2002; 96: 375–383.
Fregni F, Gimenes R, Valle AC, Ferreira MJ, Rocha RR, Natalle L et al. A randomized, sham-controlled, proof of principle study of transcranial direct current stimulation for the treatment of pain in fibromyalgia. Arthritis Rheum 2006; 54: 3988–3998.
Ngernyam N, Jensen MP, Arayawichanon P, Auvichayapat N, Tiamkao S, Janjarasjitt S et al. The effects of transcranial direct current stimulation in patients with neuropathic pain from spinal cord injury. Clin Neurophysiol 2015; 126: 382–390.
Soler MD, Kumru H, Pelayo R, Vidal J, Tormos JM, Fregni F et al. Effectiveness of transcranial direct current stimulation and visual illusion on neuropathic pain in spinal cord injury. Brain 2010; 133: 2565–2577.
Wrigley PJ, Gustin SM, McIndoe LN, Chakiath RJ, Henderson LA, Siddall PJ . Longstanding neuropathic pain after spinal cord injury is refractory to transcranial direct current stimulation: a randomized controlled trial. Pain 2013; 154: 2178–2184.
Yoon EJ, Kim YK, Kim HR, Kim SE, Lee Y, Shin HI . Transcranial direct current stimulation to lessen neuropathic pain after spinal cord injury: a mechanistic PET study. Neurorehabil Neural Repair 2014; 28: 250–259.
Mehta S, McIntyre A, Guy S, Teasell RW, Loh E . Effectiveness of transcranial direct current stimulation for the management of neuropathic pain after spinal cord injury: a meta-analysis. Spinal Cord 2015; 53: 780–785.
Kumru H, Soler D, Vidal J, Navarro X, Tormos JM, Pascual-Leone A et al. The effects of transcranial direct current stimulation with visual illusion in neuropathic pain due to spinal cord injury: an evoked potentials and quantitative thermal testing study. Eur J Pain 2013; 17: 55–66.
Celik EC, Erhan B, Gunduz B, Lakse E . The effect of low-frequency TENS in the treatment of neuropathic pain in patients with spinal cord injury. Spinal Cord 2013; 51: 334–337.
Davis R, Lentini R . Transcutaneous nerve stimulation for treatment of pain in patients with spinal cord injury. Surg Neurol 1975; 4: 100–101.
Barrera-Chacon JM, Mendez-Suarez JL, Jáuregui-Abrisqueta ML, Palazon R, Barbara-Bataller E, García-Obrero I . Oxycodone improves pain control and quality of life in anticonvulsant-pretreated spinal cord-injured patients with neuropathic pain. Spinal Cord 2011; 49: 36–42.
Dworkin RH, O’Connor AB, Backonja M, Farrar JT, Finnerup NB, Jensen TS et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain 2007; 132: 237–251.
Falci S, Best L, Bayles R, Lammertse D, Starnes C . Dorsal root entry zone microcoagulation for spinal cord injury-related central pain: operative intramedullary electrophysiological guidance and clinical outcome. J Neurosurg 2002; 97 (2 Suppl): 193–200.
Chun HJ, Kim YS, Yi HJ . A modified microsurgical DREZotomy procedure for refractory neuropathic pain. World Neurosurg 2011; 75: 551–557.
Spaic M, Markovic N, Tadic R . Microsurgical DREZotomy for pain of spinal cord and cauda equina injury origin: Clinical characteristics of pain and implications for surgery in a series of 26 patients. Acta Neurochir (Wien) 2002; 144: 453–462.
Chivukula S, Tempel ZJ, Chen CJ, Shin SS, Gande AV, Moossy JJ . Spinal and nucleus caudalis dorsal root entry zone lesioning for chronic pain: Efficacy and outcomes. World Neurosurg 2015; 84: 494–504.
Sindou M, Mertens P, Wael M . Microsurgical DREZotomy for pain due to spinal cord and/or cauda equina injuries: long-term results in a series of 44 patients. Pain 2001; 92: 159–171.
Finnerup NB, Grydehøj J, Bing J, Johannesen IL, Biering-Sørensen F, Sindrup SH et al. Levetiracetam in spinal cord injury pain: a randomized controlled trial. Spinal Cord 2009; 47: 861–867.
Chiou-Tan FY, Tuel SM, Johnson JC, Priebe MM, Hirsh DD, Strayer JR . Effect of mexiletine on spinal cord injury dysesthetic pain. Am J Phys Med Rehabil 1996; 75: 84–87.
Ginis KAM, Latimer AE, McKechnie K, Ditor DS, McCartney N, Hicks AL et al. Using exercise to enhance subjective well-being among people with spinal cord injury: the mediating influences of stress and pain. Rehabil Psychol 2003; 48: 157–164.
Cioni B, Meglio M, Pentimalli L, Visocchi M . Spinal cord stimulation in the treatment of paraplegic pain. J Neurosurg 1995; 82: 35–39.
Jensen MP, Barber J . Hypnotic analgesia of spinal cord injury pain. Aust J Clin Exp Hypn 2000; 28: 150–168.
Norrbrink C, Lundeberg T . Acupuncture and massage therapy for neuropathic pain following spinal cord injury: an exploratory study. Acupunct Med 2011; 29: 108–115.
Arienti C, Daccò S, Piccolo I, Redaelli T . Osteopathic manipulative treatment is effective on pain control associated to spinal cord injury. Spinal Cord 2011; 49: 515–519.
Defrin R, Grunhaus L, Zamir D, Zeilig G . The effect of a series of repetitive transcranial magnetic stimulations of the motor cortex on central pain after spinal cord injury. Arch Phys Med Rehabil 2007; 88: 1574–1580.
Kang BS, Shin HI, Bang MS . Effect of repetitive transcranial magnetic stimulation over the hand motor cortical area on central pain after spinal cord injury. Arch Phys Med Rehabil 2009; 90: 1766–1771.
Jetté F, Côté I, Meziane HB, Mercier C . Effect of single-session repetitive transcranial magnetic stimulation applied over the hand versus leg motor area on pain after spinal cord injury. Neurorehabil Neural Repair 2013; 27: 636–643.
Rintala DH, Fiess RN, Tan G, Holmes SA, Bruel BM . Effect of dronabinol on central neuropathic pain after spinal cord injury: a pilot study. Am J Phys Med Rehabil 2010; 89: 840–848.
Svendsen KB, Jensen TS, Bach FW . Does the cannabinoid dronabinol reduce central pain in multiple sclerosis? Randomised double blind placebo controlled crossover trial. BMJ 2004; 329: 253.
Vranken JH, Hollmann MW, van der Vegt MH, Kruis MR, Heesen M, Vos K et al. Duloxetine in patients with central neuropathic pain caused by spinal cord injury or stroke: a randomized, double-blind, placebo-controlled trial. Pain 2011; 152: 267–273.
Lunn MP, Hughes RA, Wiffen PJ . Duloxetine for treating painful neuropathy, chronic pain or fibromyalgia. Cochrane Database Syst Rev 2014; 1: CD007115.
Canadian Diabetes Association Clinical Practice Guidelines Expert Committee. Canadian Diabetes Association 2013 clinical practice guidelines for the prevention and management of diabetes in Canada. Can J Diabetes 2013; 37 (Suppl 1): S1–S212.
Attal N, Gaudé V, Brasseur L, Dupuy M, Guirimand F, Parker F et al. Intravenous lidocaine in central pain: a double-blind, placebo-controlled, psychophysical study. Neurology 2000; 54: 564–574.
Finnerup NB, Biering-Sørensen F, Johannesen IL, Terkelsen AJ, Juhl GI, Kristensen AD et al. Intravenous lidocaine relieves spinal cord injury pain: a randomized controlled trial. Anesthesiology 2005; 102: 1023–1030.
Kvarnström A, Karlsten R, Quiding H, Gordh T . The analgesic effect of intravenous ketamine and lidocaine on pain after spinal cord injury. Acta Anaesthesiol Scand 2004; 48: 498–506.
Eide PK, Stubhaug A, Stenehjem AE . Central dysesthesia pain after traumatic spinal cord injury is dependent on N-methyl-D-aspartate receptor activation. Neurosurgery 1995; 37: 1080–1087.
Siddall PJ, Molloy R, Walker S, Mather LE, Rutkowski SB, Cousins MJ . The efficacy of intrathecal morphine and clonidine in the treatment of pain after spinal cord injury. Anesth Analg 2000; 91: 1493–1498.
Attal N, Guirimand F, Brasseur L, Gaude V, Chauvin M, Bouhassira D . Effects of IV morphine in central pain: a randomized placebo-controlled study. Neurology 2002; 58: 554–563.
Moseley GL . Using visual illusion to reduce at-level neuropathic pain in paraplegia. Pain 2007; 130: 294–298.
Gustin SM, Wrigley PF, Gandevia SC, Middleton JW, Henderson LA, Siddall PJ . Movement imagery increases pain in people with neuropathic pain following complete thoracic spinal cord injury. Pain 2008; 137: 237–244.
Nayak S, Shiflett SC, Schoenberger NE, Agostinelli S, Kirshblum S, Averill A et al. Is acupuncture effective in treating chronic pain after spinal cord injury? Arch Phys Med Rehabil 2001; 82: 1578–1586.
Rapson LM, Wells N, Pepper J, Majid N, Boon H . Acupuncture as a promising treatment for below-level central neuropathic pain: a retrospective study. J Spinal Cord Med 2003; 26: 21–26.
Attal N, Mazaltarine G, Perrouin-Verbe B, Albert T . Chronic neuropathic pain management in spinal cord injury patients. What is the efficacy of pharmacological treatments with a general mode of administration? (oral, transdermal, intravenous). Ann Phys Rehabil Med 2009; 52: 124–141.
Dworkin RH, O’Connor AB, Audette J, Baron R, Gourlay GK, Haanpää ML et al. Recommendations for the pharmacological management of neuropathic pain: An overview and literature update. Mayo Clin Proc 2010; 85 (3 Suppl): S3–S14.
Finnerup NB, Otto M, McQuay HJ, Jensen TS, Sindrup SH . Algorithm for neuropathic pain treatment: an evidence based proposal. Pain 2005; 118: 289–305.
Acknowledgements
Funding for the research and publication of this supplement is provided by the Ontario Neurotrauma Foundation and the Rick Hansen Institute in their mission to advance the care of people with spinal cord injury (#PM2 964). We thank Joanna Gorski for her help with manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
BL has received consulting fees from the Northern Regional Health Authority (2014 to 2016), founded the CHANGEpain Clinic, has received fees for lecturing from DePuy and has served as expert witness. CO’C has received consulting fees from Bonify (2015–current), Lilly (2014) and Allergan (2013–current), has received lecture fees from Allergan, Biogen, Purdue, Lilly, Tweed, Tilray, Quality Respiratory Care and Respironics, has received grant support from Cytokinetics (2013–current), Biogen (2010–current), Acorda (2005–2010; 2015–current), Allergan (2010–current) and Sensimat 2015 and has served as expert witness on disability, at request of third parties including CMPA, insurance companies and law firms. TNB has received grant support from the Craig Neilsen Foundation (2015) and Allergan (2015). CC has received consulting fees from Allergan (2013) and the Rick Hansen Institute (2013) and has received grant support from the Rick Hansen Institute (2014–2016), the Ontario Neurotrauma Foundation (2011–2018), the Canadian Institutes for Health Research (2008–2016) and the Rick Hansen Institute & SCI Solutions Network (2012–2015). NF has received grant support from IMI Europain (EU/EFPIA, 2009–2015). DM has received consulting fees from Johnson and Johnson (2014), fees for lecturing from Lilly (2014), Merck-Frosst (2014) and Purdue Pharma (2013), has received grant support from Pfizer (2009–2014) and has received book royalties from Cambridge University Press. PS has received grants from the Australian & New Zealand College of Anesthetists (2015) and the New South Wales state government (2013–2015) and holds a patent for a system and method for detecting pain and its components using magnetic resonance spectroscopy, US Patent 08755862, granted 17 June 2014. RT has received grant support (2013–2016) and lecture fees (2015) from Allergan. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Spinal Cord website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Guy, S., Mehta, S., Casalino, A. et al. The CanPain SCI Clinical Practice Guidelines for Rehabilitation Management of Neuropathic Pain after Spinal Cord: Recommendations for treatment. Spinal Cord 54 (Suppl 1), S14–S23 (2016). https://doi.org/10.1038/sc.2016.90
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.90
This article is cited by
-
Developing spinal cord injury physiotherapy clinical practice guidelines: a qualitative study to determine how physiotherapists and people living with spinal cord injury use evidence
Spinal Cord (2023)
-
Neuropathic Pain and Spinal Cord Injury: Management, Phenotypes, and Biomarkers
Drugs (2023)
-
Spinal cord stimulation for neuropathic pain following traumatic spinal cord injury: a case report
Spinal Cord Series and Cases (2022)
-
Is transcranial magnetic stimulation as treatment for neuropathic pain in patients with spinal cord injury efficient? A systematic review
Neurological Sciences (2022)
-
The CanPain SCI clinical practice guidelines for rehabilitation management of neuropathic pain after spinal cord injury: 2021 update
Spinal Cord (2022)