Abstract
Study design:
Retrospective chart review of cervical spinal cord injury patients, who underwent videofluoroscopic swallowing study (VFSS).
Objectives:
To evaluate the swallowing function of cervical spinal cord injury patients, analyze the features of dysphagia and investigate their association with the clinical symptoms and signs.
Setting:
Spinal Cord Injury Unit, Yonsei Rehabilitation Hospital, Seoul, Korea.
Methods:
Retrospective study (1 May 2001–31 May 2008) on inpatients with tetraplegia. All enrolled patients underwent VFSS, and their results were correlated with clinical data including symptoms and signs indicative of dysphagia.
Results:
A total of 121 cervical spinal cord injury patients (106 male and 16 female patients) were included in this study. Ten patients showed evidence of aspiration on VFSS. Statistical correlation to aspiration was found with age, presence of tracheostomy, and symptoms and signs indicating dysphagia. However, out of the 10 patients with evident aspiration, 2 patients did not show any symptoms or signs indicating aspiration.
Conclusion:
Because of the possibility of silent aspiration, we recommend that physicians treating patients with cervical spinal cord injury should always take the possibility of dysphagia and silent aspiration into consideration, especially in case of previous manifestation of pneumonia, presence of tracheostomy, or presence of signs and symptoms indicating dysphagia.
Similar content being viewed by others
Introduction
Dysphagia is a frequent problem among cervical spinal cord injury patients. In many patients, this problem is transient and tends to recover naturally throughout the rehabilitation process.1, 2 However, the fact that aspiration risk is a major risk factor of hospital-acquired pneumonia,3 and that in spinal cord injury patients respiratory problems, especially pneumonia, is the most common cause of death,4 makes precise evaluation of swallowing function in cervical spinal cord injury patients invaluable.
Frequently used measures for the assessment of swallowing function include various bedside evaluation methods, videofluoroscopic swallowing study (VFSS) and fiberoptic endoscopic examination of swallowing (FEES). Bedside swallowing evaluation has the advantage of simple implementation, but bears the disadvantage of low sensitivity and specificity in detecting dysphagia.5 VFSS and FEES both show high sensitivity and specificity, and each has its own advantages and disadvantages. The view obtained from each tool is entirely different and the portability of endoscopy is unique.6 FEES can be carried out without limitations in patient positioning, but in VFSS the patient usually has to remain in upright position.6 Neither one is significantly more effective in detecting dysphagia or in preventing aspiration pneumonia; rather, both methods are complementary in evaluating swallowing function.6 Moreover, none of the above evaluation tools have been recommended over the other for the evaluation of dysphagia in spinal cord injury patients. VFSS is primarily conducted at our hospital for the assessment of swallowing function in spinal cord injury patients, as the vast majority of our inpatients and outpatients are not in the intensive care unit or ventilator assisted, and thus do not have problems with patient positioning, and as VFSS helps determine abnormalities of swallowing comprehensively, including oral, pharyngeal and esophageal phases.
In the past, several studies investigated dysphagia in spinal cord injury patients. Kirshblum et al.7 reported that in their study, 42 of 187 traumatic cervical spinal cord injury patients who showed positive results on bedside swallow evaluation were further tested with VFSS. Dysphagia was detected in 31 patients. Significant association with dysphagia was shown for age, tracheostomy and mechanical ventilation, and anterior approach for cervical spine surgery.
Wolf et al.2 reported that 51 cervical spinal cord injury patients who were admitted to the intensive care unit because of respiratory insufficiency underwent FEES. Among the 21 patients who had shown severe dysphagia, all except 3 patients showed improvement of swallowing disorder.
Abel et al.8 reported that 73 patients with cervical spinal cord injury underwent bedside swallow evaluation and 32 patients who were suspected to have dysphagia were further tested with VFSS. Dysphagia was detected in 26 patients and incidence of pneumonia in these patients at least 2 weeks after the initial injury was found to be significantly higher than in the remaining patients. Moreover, the authors classified the type of dysphagia into oral, pharyngeal and esophageal dysphagia according to the VFSS findings.
Seidl et al.9 reported that 175 cervical spinal cord injury patients underwent FEES and 28 patients were diagnosed with dysphagia. Moreover, the authors reported that besides history of tracheostomy, no other clinical factor was significantly associated with dysphagia.
In these previous studies, either only those patients suspected of dysphagia on bedside swallowing tests underwent the objective swallowing evaluation, or the objective study was conducted on all patients, but without additional investigation of the relationship between the study results and the clinical presentation of each patient. Thus, the purpose of this study is to evaluate the swallowing function of cervical spinal cord injury patients admitted to our hospital, analyze the features of dysphagia, and investigate their association with the clinical symptoms and signs.
Materials and methods
Patients
Included in this study were cervical spinal cord injury patients admitted or transferred to the Spinal Cord Injury Unit, Yonsei Rehabilitation Hospital, Seoul, Korea, between 1 May 2001 and 31 May 2008, who have signed a written consent form for VFSS. VFSS was carried out regardless of time post injury or surgery, or state of alimentation of the patient.
Each patient underwent neurological examination according to the American Spinal Injury Association Grading Scale (ASIA), and only those patients with a neurological level at or higher than T1 were included. Exclusion criteria were history of dysphagia before the spinal cord injury, combined traumatic brain injury, language or cognitive impairment that inhibits one-step verbal command obey and failure of VFSS.
This study was approved by the medical ethics committee at our hospital.
Methods
The medical record of each patient was reviewed to verify history of spine surgery, tracheostomy or pneumonia, and the patient was interviewed to identify symptoms (inability or difficulty of swallowing) and signs (post-swallow coughing, post-injury or post-swallow change of voice) that indicate dysphagia.
VFSS was carried out with the patient in upright position (Figure 1), and barium in semisolid and in liquid consistency was administered in large (50 ml) and small (10 ml) amounts. Videofluoroscopy from the lateral view was recorded on video, which was evaluated by two experienced physicians. Besides identification of possible aspiration, the following features of swallowing function were assessed: features of the oral phase, such as labial closure, rotatory lateral movement of tongue and posterior propelling of the bolus; features of the pharyngeal phase, such as swallowing reflex, closure of velopharyngeal port, pharyngeal peristalsis, elevation of larynx and cricopharyngeal dysfunction; and features of the esophageal phase, such as contraction of the cricopharyngeus muscle.
Statistical analysis
Data collected were encoded, and absolute and relative frequency distributions were analyzed. Statistical analysis was performed with Statistical Package for the Social Sciences (SPSS 17.0 for Windows, IBM Corp., Somers, NY, USA). Frequency, means and standard deviations were determined. Correlations within the data were tested in a cross-tabulation with either the χ2-test or Fisher's exact test at a significance level of P<0.05. Comparisons of means were performed with the independent t-test.
Results
Patients
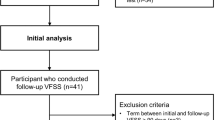
The study consisted of 121 patients, of which 105 were male (86.7%) and 16 were female (13.2%). Mean age of the patients was 44.93 years (range 9–78 years) and mean duration between spinal cord injury and VFSS was 178.35 days (range 12–1062 days).
At the time of VFSS, 38 (31.4%) patients underwent a tracheostomy, and 62 (51.2%) patients had a history of tracheostomy. A total of 103 (85.1%) patients had undergone spinal surgical procedures, of which 71 (58.7%) were anterior approach procedures and 11 (9.1%) were anterior and posterior approach procedures (Table 1).
Neurological examination showed 72 (59.5%) patients with complete spinal cord injury and 49 (40.5%) patients with an incomplete injury (Table 2).
The vast majority (118 (97.5%)) of patients suffered from paralysis as a result of trauma, of which motor vehicle accidents were most common with 81 (66.9%) patients. Only three (2.5%) patients suffered spinal cord injury due to non-traumatic causes (Table 3).
Symptoms and signs
Patients’ interviews revealed that 22 (18.2%) patients suffered from symptoms indicating dysphagia, of which 16 (13.2%) patients complained of difficulty in swallowing and 6 (5.0%) patients reported that swallowing was impossible, which included impossibility to initiate voluntary swallowing and complete absence of swallowing reflex.
A total of 35 (28.9%) patients showed signs indicating dysphagia, of which post-swallow coughing was the most common (19 (15.6%)).
A total of 82 (67.8%) patients showed neither symptoms nor signs indicating dysphagia (Table 4).
Results of VFSS
Descriptive analysis of VFSS results showed abnormal findings in oral phase in 5 (4.1%) patients and in pharyngeal phase in 65 (53.7%) patients. No patient showed abnormal findings in esophageal phase. The most common abnormal finding in pharyngeal phase was delayed swallowing reflex, which was observed in 51 (42.1%) patients. Aspiration was evident in 10 (8.3%) patients, of which 9 (7.4%) patients showed during-swallowing aspiration (Table 5).
Comparison of patients with and without evidence of aspiration
The mean age of patients with aspiration (54.40±13.39) was significantly higher compared with patients without aspiration (44.08±15.50) (P=0.044). Furthermore, linear by linear association with age groups of 0–19, 20–29, 30–39, 40–49, 50–59, 60–69 and 70–79 years showed significant increase of aspiration with age (P=0.039).
Mean duration between spinal cord injury and VFSS showed a slight difference (172.00±125.50 and 178.92±164.47), which was statistically not significant (P=0.897; Tables 6 and 7).
Incidence of aspiration was not significantly different in patients classified according to the etiology of injury (P=0.260). On simply comparing patients with traumatic and non-traumatic causes of injury, all patients with evidence of aspiration had traumatic causes of injury, but it failed to gain statistical significance (P=0.999).
Incidence of aspiration was also not significantly different in patients classified according to the ASIA classification (P=0.697). Comparison between patients with complete and incomplete spinal cord injury (90.3 and 93.9%, accordingly) did not show any statistical significance (P=0.738).
Moreover, classifying patients according to spinal surgical procedures did not show significant difference in incidence of aspiration (P=0.131). Comparison of patients with and without the anterior approach spinal surgical procedure (93.9 and 87.2%, accordingly) did not show any statistical significance (P=0.289).
Patients with tracheostomy by the time of VFSS showed a significantly higher incidence of aspiration (18.4%) compared with patients without tracheostomy (3.6%) (P=0.011). However, history of tracheostomy did not show significant correlation with incidence of aspiration (12.9 and 3.4%, accordingly; P=0.096).
Patients with symptoms indicating dysphagia showed significantly higher incidence of aspiration (27.3%) compared with patients without symptoms (4.0%; P=0.002), and patients with signs showed significantly higher incidence of aspiration (22.9%) than patients without signs (4.0%; P=0.001). Among the patients with aspiration on VFSS, four patients had not reported any symptoms indicating dysphagia, of which two patients had not reported any signs indicating dysphagia, which indicates the possibility of silent aspiration in this population.
Discussion
Dysphagia, being a risk factor of pneumonia, is a problem that requires close attention and immediate treatment.
In this study, 10 of 121 (8.3%) tetraplegic patients showed evidence of aspiration on VFSS. Prevalence is low compared with previous studies, which reported prevalence of dysphagia ranging between 16.0% (28 of 175 patients) and 41.2% (21 of 51 patients). Considering the fact that Abel et al. reported a recovery of dysphagia on follow-up VFSS in 9 of 22 surviving patients with initially confirmed dysphagia, and the fact that the mean duration from injury to study enrollment was shorter in these studies, the low prevalence in this study may be explained by the possible spontaneous recovery in some patients. However, the mean duration between injury and VFSS in patients with and without aspiration failed to gain statistical significance.
Age was found to be statistically related to dysphagia by Kirshblum et al.,7 but not by Wolf and Meiners,2 Abel et al.8 or Seidl et al.9 In the present study, the mean age of patients with aspiration was significantly higher compared with the patients without evidence of aspiration. Even linear by linear association after categorization in different age groups showed higher prevalence of dysphagia with increasing age. The statistical correlation between aging and dysphagia seems to be reasonable, as aging itself, independently of cervical spinal cord injury, can increase the risk of dysphagia, secondarily through increased prevalence of multiple chronic diseases or change of function of organs such as the esophagus.10 Multiple surveys in the general population also have shown higher prevalence of dysphagia in the elderly.11, 12, 13 The low prevalence of dysphagia in each of the previous studies could be accounted for by the absence of statistical significance.
The presence of tracheostomy at the time of VFSS was significantly related to the higher incidence of aspiration in this study. This correlation was also supported in previous studies.2, 7, 8, 9 Although the cause–effect relationship between dysphagia and the need for tracheostomy is unclear, various reports of increased risk of dysphagia through tracheostomy give weight to the possibility that risk of dysphagia increases through the existence of tracheostomy in cervical spinal cord injury patients. This was also evident in the present study, as the incidence of aspiration was significantly related to the presence of tracheostomy by the time of VFSS, but not to the history of tracheostomy. Gross et al.14 also reported that the reduction of respiratory volume and subglottic pressure due to a tracheostomy tube or a thorax trauma raises the risk of aspiration. Thus, we do agree with Abel et al.8 that we should try more aggressively to close the tracheostomy earlier.
A correlation between the anterior surgical approach and occurrence of dysphagia was not observed in this study. We believe that the absence of clinical significance, despite the abundance of previous studies, which showed a significant correlation,15, 16, 17 is due to the low number of patients with evident aspiration.
Presence of both symptoms and signs indicating dysphagia was significantly related to increased incidence of aspiration. However, it is worthy to note that 2 out of 10 patients with evident aspiration did not show symptoms or signs that could indicate dysphagia. Two additional patients showed signs but no symptoms. Previous studies on dysphagia in cervical spinal cord injury patients either performed objective swallowing evaluation only in patients with suspected dysphagia on bedside swallowing tests or performed the objective swallowing evaluation on all enrolled patients, however, without evaluating their association with clinical symptoms and signs. Thus, prevalence of silent aspiration after cervical spinal cord injury was not investigated. Performing VFSS or FEES routinely on all patients would be impossible because of ethical and cost/resource issues, but physicians treating patients with cervical spinal cord injury should always take the possibility of dysphagia and silent aspiration into consideration, especially in case of previous manifestation of pneumonia, presence of tracheostomy, or presence of signs and symptoms indicating dysphagia. Patients with silent aspiration are in a higher-risk group for the development of pneumonia or other complications because of the lack of cough reflex reduces patients, family, and hospital staff to detect that aspiration is occurring.18
Although treatment of dysphagia in cervical spinal cord injury patients is beyond the scope of this article, in case of evident aspiration, conservative measures with regular follow-up evaluation of VFSS or FEES would be feasible, as favorable outcome and natural recovery have been previously reported.8 In case of liquid aspiration without evident aspiration of semisolids, adjusting food consistencies with the use of food thickener would help, and in case of aspiration in both liquids and semisolids, a temporary alimentation through a Levin tube would be a primary measure. However, for further research, a prospective longitudinal study would be ideal, to investigate the natural recovery of dysphagia, before we can decide the time frame in which further natural recovery is unlikely to occur, so that a permanent gastrostomy could be recommended.
Two limitations, which we encountered in this study, were the lack of specific time frame, in which we conducted VFSS, and the lack of follow-up data after conducting VFSS, such as the occurrence of pneumonia, management approach in patients with abnormal VFSS findings or data of follow-up VFSS evaluations of patients with evident aspiration. The lack of specific time frame led to limitations when interpreting the results of VFSS, as dysphagia in spinal cord injury patients tends to improve naturally over time, and the lack of follow-up data led to limitations when verifying the clinical impact of abnormal VFSS findings. As noted above, a prospective longitudinal study in the future would be of great help to understand the natural recovery of dysphagia in cervical spinal cord injury patients and to build a management plan for cervical spinal cord injury patients with accompanied dysphagia.
Conclusion
Dysphagia, which is a potential risk factor of aspiration pneumonia, requires close attention in cervical spinal cord injury patients. Owing to the possibility of silent aspiration, we recommend that physicians treating patients with cervical spinal cord injury should always take the possibility of dysphagia and silent aspiration into consideration, especially in case of previous manifestation of pneumonia, presence of tracheostomy or presence of signs and symptoms indicating dysphagia.
References
Steven Kirshblum DIC, DeLisa JA . Spinal Cord Medicine. Lippincott Williams & Wilkins, 2002.
Wolf C, Meiners TH . Dysphagia in patients with acute cervical spinal cord injury. Spinal Cord 2003; 41: 347–353.
Cakir Edis E, Hatipoglu ON, Yilmam I, Eker A, Tansel O, Sut N . Hospital-acquired pneumonia developed in non-intensive care units. Respiration 2009; 78: 416–422.
NSCISC. 2009 NSCISC Annual Statistical Report—Complete Public Version 2009. https://www.nscisc.uab.edu.
Bours GJ, Speyer R, Lemmens J, Limburg M, de Wit R . Bedside screening tests vs videofluoroscopy or fibreoptic endoscopic evaluation of swallowing to detect dysphagia in patients with neurological disorders: systematic review. J Adv Nurs 2009; 65: 477–493.
Langmore SE . Evaluation of oropharyngeal dysphagia: which diagnostic tool is superior? Curr Opin Otolaryngol Head Neck Surg 2003; 11: 485–489.
Kirshblum S, Johnston MV, Brown J, O’Connor KC, Jarosz P . Predictors of dysphagia after spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1101–1105.
Abel R, Ruf S, Spahn B . Cervical spinal cord injury and deglutition disorders. Dysphagia 2004; 19: 87–94.
Seidl RO, Nusser-Muller-Busch R, Kurzweil M, Niedeggen A . Dysphagia in acute tetraplegics: a retrospective study. Spinal Cord 2009, 197–201.
Achem SR, Devault KR . Dysphagia in aging. J Clin Gastroenterol 2005; 39: 357–371.
Lindgren S, Janzon L . Prevalence of swallowing complaints and clinical findings among 50–79-year-old men and women in an urban population. Dysphagia 1991; 6: 187–192.
Talley NJ, Weaver AL, Zinsmeister AR, Melton III LJ . Onset and disappearance of gastrointestinal symptoms and functional gastrointestinal disorders. Am J Epidemiol 1992; 136: 165–177.
Tibbling L, Gustafsson B . Dysphagia and its consequences in the elderly. Dysphagia 1991; 6: 200–202.
Gross RD, Steinhauer KM, Zajac DJ, Weissler MC . Direct measurement of subglottic air pressure while swallowing. Laryngoscope 2006; 116: 753–761.
Bertalanffy H, Eggert HR . Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien) 1989; 99: 41–50.
Cloward RB . The anterior approach for removal of ruptured cervical disks. J Neurosurg 15: 602–617, 1958.
Martin RE, Neary MA, Diamant NE . Dysphagia following anterior cervical spine surgery. Dysphagia 1997; 12: 2–8; discussion 9–10.
Garon BR, Sierzant T, Ormiston C . Silent aspiration: results of 2000 video fluoroscopic evaluations. J Neurosci Nurs 2009; 41: 178–185; quiz 186–177.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shin, J., Yoo, J., Lee, Y. et al. Dysphagia in cervical spinal cord injury. Spinal Cord 49, 1008–1013 (2011). https://doi.org/10.1038/sc.2011.34
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.34
Keywords
This article is cited by
-
Pulmonary function and sarcopenia as predictors of dysphagia in cervical spinal cord injury
Spinal Cord (2024)
-
Oropharyngeal Dysphagia in Acute Cervical Spinal Cord Injury: A Literature Review
Dysphagia (2023)
-
Translating Dysphagia Evidence into Practice While Avoiding Pitfalls: Assessing Bias Risk in Tracheostomy Literature
Dysphagia (2021)
-
The time course of dysphagia following traumatic cervical spinal cord injury: a prospective cohort study
Spinal Cord (2020)
-
Oropharyngeal dysphagia management in cervical spinal cord injury patients: an exploratory survey of variations to care across specialised and non-specialised units
Spinal Cord Series and Cases (2019)