Abstract
Study design:
Female Wistar rats (225 g) underwent spinal cord injury (SCI) at the T4 segment and were assigned to one of the three groups treated with: (1) saline; (2) 7.5 mg kg–1 Reparixin; or (3) 15 mg kg–1 Reparixin. Reparixin is a small molecule, allosteric noncompetitive inhibitor of CXCR1 and CXCR2 chemokine receptors involved in inflammation.
Methods:
Spinal cord homogenates at 12 and 72 h post-SCI were assayed for tumor necrosis factor α (TNF-α) and cytokine-induced neutrophil chemoattractant (CINC)-1 using enzyme-linked immunosorbant assay (ELISA). Myeloperoxidase activity and western blots for CD68, Fas and p75 content were used to assess inflammation and death receptor ligands, respectively. Histopathology and neurological outcomes were assessed by immunohistochemistry, locomotion scoring and cardiovascular measurement of autonomic dysreflexia 4 weeks post-SCI.
Results:
Both 7.5 and 15 mg kg–1 doses of Reparixin reduced levels of TNF-α and CINC-1 72 h post-SCI and decreased macrophage (CD68) content in the spinal cord lesion. Only 15 mg kg–1 Reparixin reduced both Fas and p75 levels in the spinal cord compared with untreated SCI. We observed a reduced lesion area and increased neuron number in the gray matter of Reparixin-treated rats. Hindlimb motor scores at 7 and 28 days post-SCI were improved by 15 mg kg–1 Reparixin treatment. Both 7.5 and 15 mg kg–1 Reparixin reduced development of autonomic dysreflexia 4 weeks post-SCI. The change in mean arterial pressure, induced by cutaneous or visceral stimulation, was reduced by 40–50%.
Conclusion:
Acute treatment with 15 mg kg–1 Reparixin reduces acute inflammation and is associated with minor improvements in motor function and a significant reduction in the severity of autonomic dysreflexia.
Similar content being viewed by others
Introduction
After spinal cord injury (SCI), inflammatory and oxidative processes are activated in the spinal cord by ischemia, cellular damage and hemorrhage. This inflammatory response exacerbates secondary injury mechanisms and diminishes the prospect for neurological recovery.1 Recently, treatment strategies designed to selectively reduce inflammation and cell death after SCI have demonstrated increased axonal sparing, neuroprotection and improved neurological outcomes after SCI.2, 3, 4, 5, 6 Targets have included chemokine receptors,3, 4, 7 cell adhesion integrins,2, 8 and cytokines and death receptors5, 6 that are upregulated after SCI.
The CXC chemokine, cytokine-induced neutrophil chemoattractant (CINC)-1 (rat interleukin 8), is upregulated after brain injury in rats,9 activates the G-protein-coupled receptors CXCR1 and CXCR2, and induces neutrophil recruitment and activation after ischemia.10 Reparixin (R(−)-2-(4-isobuthylphenyl)propionyl methanesulfonamide) is a novel small molecule antagonist that functions as an allosteric noncompetitive inhibitor of CXCR1 and CXCR2 and has been shown to effectively inhibit the CINC-1-induced chemotaxis of rat neutrophils in a concentration-dependent manner.10 Recently, Reparixin treatment has also been shown to attenuate the inflammatory response, reduce gliosis, promote white matter sparing and improve hindlimb locomotor recovery in rats after spinal cord contusion injury.7 Although the development of autonomic dysreflexia after SCI has been demonstrated to be sensitive to anti-inflammatory treatment2, 8 and associated with the severity of injury and tissue sparing,2, 11 the effects of Reparixin treatment on sensory or autonomic function have not been investigated.7
Autonomic dysreflexia, a condition that develops in 50–90% of patients with upper thoracic and cervical SCI, is characterized by symptoms that include episodic hypertension, debilitating headaches and profuse sweating.12, 13 The rapid increase in arterial pressure can lead to cardiac arrhythmias, seizures and hemorrhagic strokes.13, 14 We hypothesized that acute treatment of Reparixin would modulate the acute inflammatory response, promote white- and gray-matter sparing and improve blood pressure regulation after SCI by diminishing the development of autonomic dysreflexia. The attenuated expression of death receptors Fas and p75, previously linked to SCI-induced apoptosis,5, 6, 15 was explored as a potential mechanism for the beneficial Reparixin treatment effects.
Materials and methods
Animals
Female Wistar rats (225±2 g) were obtained from Harlan Laboratories. All animal procedures were approved by the Dalhousie Committee on Laboratory Animals and performed according to the Canadian Council on Animal Care Guide to the Care and Use of Experimental Animals.
Clip-compression SCI
Rats were assigned to either uninjured (n=12) or SCI groups (n=72). Before surgery, the rats were pre-medicated with subcutaneous injections of atropine (0.05 mg kg–1, Sigma-Aldrich Canada, Oakville, ON, Canada), enrofloxacin (Baytril, 50 mg ml–1; Bayer Inc., Toronto, ON, Canada) and buprenorphine (Temgesic, 0.05 mg kg–1, Schering-Plough Ltd, Hertfordshire, UK). Atropine served to strengthen heart contractions and guard against spinal shock-induced hypotension and bradycardia.16 After laminectomy removed the dorsal half of T3, the jaws of an aneurysm clip (Toronto Western Research Institute) were released around the T4 spinal cord segment to compress the spinal cord for 60 s with 35 g of closing force.11, 17 Postoperative care of the animals included administration of subcutaneous saline (3 ml daily), Temgesic and Baytril for 3 days post-SCI and bladder compression to void urine twice daily until autonomic control of voiding returned.17
Reparixin treatment
After SCI, rats were treated with either saline or Reparixin. The Reparixin-treated animals were assigned to one of the three groups: high-dose (R2, 15 mg kg–1) 12-h acute treatment, high-dose 72-h treatment or low-dose (R1, 7.5 mg kg–1) 72-h treatment. All rats were given tail vein injections of either saline or Reparixin (11.5 mg ml–1, 300 μl) 1 h after SCI surgery to rapidly achieve effective plasma drug concentrations. According to the desired outcome measurements, rats were killed at 12 h, 72 h or 4 weeks after SCI. SCI rats in the acute 12-h end point were administered subcutaneous injections of saline or Reparixin (23 mg ml–1, 160 μl) every 2 h after the tail vein injection. SCI rats in the 72-h or 4-week end point groups were implanted with osmotic pumps (Durect Corp., Cupertino, CA, USA, Alzet model 2ML4, 10 μl h–1) that were filled with saline, Reparixin (R1, 115 mg ml–1) or Reparixin (R2, 230 mg ml–1) immediately after SCI surgery, and primed at 37 °C for 4–16 h before implantation. The injection syringes and osmotic pumps were prepared by a ‘third party’ and numbered. The investigators were kept blind to the code and only matched the treatment number to animal number.
Acute outcome measurements
Uninjured rats and rats 12 and 72 h after SCI were killed by a fatal intraperitoneal dose of urethane and transcardially perfused with ice-cold phosphate-buffered saline (pH 7.4). Thoracic (T) spinal cord segments T2–T6 (lesion) and T7–T10 (caudal to lesion) were removed and immediately frozen in liquid nitrogen.
MPO assay
Spinal cord segments were sonicated in myeloperoxidase (MPO) buffer and centrifuged at 10 000 g for 15 min at 4 °C as previously described.18 The cytosolic protein fraction and membranous protein fractions were collected and assayed for total protein concentration using the bicinchoninic acid (BCA) Protein Assay (Pierce, Rockford, IL, USA). MPO activity was measured in the cytosolic protein fraction of spinal cord homogenates by a colorimetric assay as previously described.18
Enzyme-linked immunosorbant assays
Tumor necrosis factor α (TNF-α) and CINC-1 levels were measured in the cytosolic protein fraction of spinal cord homogenates using enzyme-linked immunosorbant assay kits from R&D Systems according to the manufacturer's instructions (TNF-α, DY510; CINC-1, DY515; Minneapolis, MN, USA).
Western blot analysis
Relative protein content in the spinal cord lesion of CD68, Fas and p75 was determined by standard western blot techniques after 30 μg of membrane fraction protein was separated by SDS-polyacrylamide gel electrophoresis. Primary antibodies used were specific to CD68 (1:500; MCA 341R, Serotec, Oxford, UK), Fas (1:500; 05–351, Upstate/Millipore, Billerica, MA, USA) and p75 (1:500; sc-831, Santa Cruz Biotechnology, Santa Cruz, CA, USA). After incubation in horseradish peroxidase-conjugated secondary anitibodies, an ECL chemiluminescence kit (Amersham, Piscataway, NJ, USA) was used and the blot exposed to film. An Alpha Imager 2200 and software (Alpha Innotech, San Leandro, CA, USA) was used to capture the image and quantify relative band intensity.
Chronic outcome measurements
Neurological outcomes
Twice weekly after SCI, open-field locomotion testing was performed and functional scoring assessed for each rat according to the 21-point BBB scale.19 This scale measures range of motion about each hindlimb joint: a score of 7 indicates there is extensive range of motion about each joint; a score of 10 reports occasional weight-supported plantar steps but without fore and hindlimb coordination.19
At 1 week after left carotid artery canulation, pulsatile arterial pressure was recorded with a Powerlab system (ADInstruments, Colorado Springs, CO, USA) from freely moving rats.17 Rats were gently restrained to connect the arterial canula to the pressure transducer (Ohmeda Medical Devices, Columbia, MD, USA, 682021), and to insert a balloon-tipped Foley balloon-tip catheter (8Fr. 3 cc balloon; CR Bard Inc., Murray Hill, NJ, USA) 4.0 cm into the colon. Autonomic dysreflexia was triggered by 1.5-ml balloon distension of the colon or by pinching of skin dorsal to the lumbar vertebrae.11, 17 The average and peak change in mean arterial pressure (MAP) and heart rate during the stimulation was measured from the baseline resting values preceding the stimulus. Colon distension- and skin pinch-induced changes were measured twice during each testing session, allowing 15–20 min of recovery time between tests. Cardiovascular testing was repeated on each animal 1 day after the initial test. Results from each test were averaged for each animal and compared between groups.
Lesion histopathology
At 4 weeks after SCI, rats were transcardially perfused with 4% paraformaldehyde in phosphate-buffered saline and the spinal cord segments containing the lesion were removed and equilibrated to 30% sucrose. Solochrome cyanine staining of compact myelin,2 and double-fluorescent immunohistochemistry for glial fibrillary acid protein (1:1000, ab5804, Chemicon, Temecula, CA, USA) and neuron-specific transcription factor, NeuN (1:5000, mab377, Chemicon) was performed on 16-μm thick serial longitudinal sections.
Lesion area
The lesion area was determined from solachrome cyanine-stained sections as described previously.20 The lesion area was determined from digital images of longitudinal sections of the spinal cord segments containing the lesion with Image Pro software (Media Cybernetics, Bethesda, MD, USA).
Neuron number
A Zeiss microscope, digital camera and LSM 510 software (Zeiss Canada Ltd., Toronto, ON, Canada) was used to capture a series of × 20 images in 500 μm increments from longitudinal spinal cord sections immunoreactive (IR) for NeuN and glial fibrillary acid proteins. The number of NeuN-IR neurons was counted manually in each 500 μm image. This was repeated in four consecutive images moving caudally from the lesion epicenter. The average number of neurons present 2000 μm from the epicenter was calculated from a minimum of four sections for each spinal cord lesion in saline- and Reparixin-treated SCI rats.
Data analysis and statistics
Data collection was performed in a blinded manner with the researcher unaware of group designation. Densitometric analysis was used to quantify results of western blots. Analysis of variance was performed on the results and significant differences among group means determined by Newman–Keuls post hoc test (P<0.05).
Results
Acute inflammation
The levels of the cytokine TNF-α were increased significantly at 12 and 72 h after SCI. Treatment with Reparixin reduced the levels of TNF-α at 12 h in the SCI lesion by 46% (Figure 1a). At 72 h post-SCI, 15 mg kg–1 Reparixin, but not 7.5 mg kg–1, was effective at reducing TNF-α levels compared with spinal cord lesions of saline-treated SCI animals. TNF-α levels at 72 h remained significantly elevated above levels in uninjured control spinal cord (Figure 1a). The levels of the chemokine CINC-1 were also increased at both 12 and 72 h after SCI (Figure 1b). Reparixin treatment had no effect on the levels of CINC-1 in the SCI lesion 12 h after injury. Compared with saline-treated SCI, both the low dose (7.5 mg kg–1) and the high dose (15 mg kg–1) of Reparixin significantly reduced CINC-1 levels in the spinal cord lesion 72 h after SCI (Figure 1b).
Concentration of cytokines TNF-α (a) and CINC-1 (b) in spinal cord homogenates of uninjured, saline-treated SCI and Reparixin-treated SCI rats. Protein levels were determined at 8 and 72 h after SCI by ELISA and are expressed as mean±s.e. +R1=7.5 mg kg–1 Reparixin-treated SCI; +R2, 15 mg kg–1 Reparixin-treated SCI; SCI, saline-treated SCI. *Denotes a significant difference from uninjured, P<0.05. φDenotes a significant difference from saline-treated SCI, P<0.05. n=8 animals in each group.
MPO was elevated at 12 and 72 h after SCI compared with uninjured spinal cord (Figure 2a). Reparixin treatment had no significant effect on MPO activity at 12 or 72 h after SCI. MPO activity 72 h after SCI was reduced by 30% following Reparixin treatment (Figure 2a), but due to variability, this difference was not significant. Inflammation was also assessed by western blot for CD68, a lysosomal protein in macrophages (Figure 2b). Densitometric analysis demonstrated a significant decrease in macrophage content in SCI lesions from Reparixin-treated compared with untreated rats at 72 h post-SCI. Both 7.5 and 15 mg kg–1 doses of Reparixin, in a dose-dependent manner, were effective at decreasing macrophage infiltration (Figure 2b).
Inflammation in spinal cord lesion after SCI. (a) MPO activity in spinal cord homogenates of uninjured, saline-treated SCI and Reparixin-treated SCI rats at 8 and 72 h after injury. Enzyme activity was quantified by a kinetic enzymatic assay and expressed as mean±s.e. +R1, 7.5 mg kg–1 Reparixin-treated SCI; +R2, 15 mg kg–1 Reparixin-treated SCI; SCI, saline-treated SCI; U, uninjured. *Denotes a significant difference from uninjured, P<0.05. φ Denotes a significant difference saline-treated SCI, P<0.05. At least n=8 animals in each group. (b) Representative western blot for CD68 protein and cumulative results from densitometry. Results from three separate blots were pooled, the average of all saline-treated SCI values set to 100 and others expressed as a relative value. Abbreviations are as listed for (a). *Denotes a significant difference from uninjured, P<0.05. φDenotes a significant difference from saline-treated SCI, P<0.05. n=8 animals in each group.
Death receptor ligand expression
The relative level of death receptor ligands, Fas and p75, were significantly increased at 72 h after SCI. The increase in Fas expression was diminished by both 7.5 and 15 mg kg–1 Reparixin treatment to levels similar to uninjured controls (Figure 3a). In contrast to Fas, levels of p75 after SCI were only diminished by the 15 mg kg–1 dose of Reparixin (Figure 3b).
Expression of death receptor ligands Fas and p75 after SCI. (a) Representative western blot for Fas protein and cumulative densitometry results. (b) Representative western blot for p75 protein and cumulative densitometry results. For both Fas and p75, results from three separate blots were pooled, the average of all saline-treated SCI values set to 100 and others expressed as a relative value. +R1, 7.5 mg kg–1 Reparixin-treated SCI; +R2, 15 mg kg–1 Reparixin-treated SCI; SCI, saline-treated SCI; U, uninjured. *Denotes a significant difference from uninjured, P<0.05. φDenotes a significant difference from saline-treated SCI, P<0.05. n=8 animals in each group.
Histopathological assessment of the spinal cord lesion
Staining of compact myelin near the lesion with solachrome cyanine indicated that the 35 g clip SCI spared very few myelinated axons (Figure 4a). Treatment with Reparixin (15 mg kg–1) appeared to ameliorate the loss of myelinated axons near the lesion (Figure 4a). Quantitative analysis of the lesion area confirmed this assessment as Reparixin treatment significantly reduced the lesion area caused by SCI (Figure 4b).
Lesion area assessment after SCI. (a) Representative micrographs of longitudinal sections from saline-treated SCI and Reparixin-treated rat spinal cord lesions stained for compact myelin with Solachrome cyanin. *Denotes approximate epicenter of each lesion. (b) Quantification of lesion area from saline-treated SCI and Reparixin-treated rat spinal cords. Average±s.e. of each group is shown in bar graph, n=6. φDenotes a significant difference from saline-treated SCI, P<0.05. +R2, 15 mg kg–1 Reparixin-treated SCI; SCI, saline-treated SCI.
In addition, the neuropil immediately caudal to the lesion epicenter was examined for surviving neurons. Using the neuron-specific transcription factor NeuN as a neuronal marker, the number of neurons was counted in 500 μm increments (Figure 5a). Within 500 μm of the lesion epicenter, no NeuN-positive neurons were observed in either saline- or Reparixin-treated SCI animals. Neuron counts increased in both groups with added distance from the lesion. At each 500 μm increment from the lesion eipicentre, the number of neurons was greater in spinal cords of the Reparixin-treated (15 mg kg–1) animals compared with the untreated SCI animals (Figure 5b).
Neuron count caudal to SCI lesion in saline- and Reparixin-treated rats. (a) Representative × 5 micrographs of immunohistochemistry for GFAP (green) and neuron-specific transcription factor NeuN (red) in spinal cord sections containing the lesions from saline-treated and Reparixin-treated SCI rats. *Denotes approximate epicenter of each lesion. (b) × 40magnification of neurons in spinal cord sections from (a). Images were selected 1000–1500 μm from lesion epicenter. Scale bar=500 μm. (c) Summary of neuron counts. Average±s.e. of each group is shown in bar graph, n=6. φDenotes a significant difference from saline-treated SCI, P<0.05. +R2, 15 mg kg–1 Reparixin-treated SCI; SCI, saline-treated SCI.
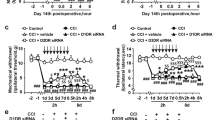
Neurological outcomes
Improvement on the 21-point BBB scale was observed in all groups as scores increased over time (Figure 6). At 1 week after SCI, both the 7.5 and the 15 mg kg–1 Reparixin-treated rats scored significantly higher than untreated SCI rats (only 15 mg kg–1 data shown). At 4 weeks after SCI, more Reparixin-treated rats were able to weight bear and step in a coordinated manner than saline-treated rats.
Motor neurological outcomes 28 days after SCI. Assessment of hindlimb motor performance according to 21-point BBB scale. Each point on graph represents the average±s.e. of saline-treated SCI rats and Reparixin-treated SCI rat's performance at each day. The average±s.e. of each group is shown at each time point. +R2=15 mg kg–1 Reparixin-treated SCI; SCI, saline-treated SCI. φDenotes a significant difference from saline-treated SCI, P<0.05. At least n=8 animals in each group.
Resting MAP and heart rate data, as well as cardiovascular response to colon distension and skin pinch, for saline- and Reparixin-treated SCI rats are reported in Table 1. Representative recording traces of cardiovascular data for saline- and Reparixin-treated rats are presented in Figure 7a. Dysfunctional regulation of blood pressure that commonly occurs after severe upper thoracic SCI was observed in saline-treated SCI rats. Both colon distension- and skin pinch-induced autonomic dysreflexia was accompanied by significant increases in MAP and bradycardia from baseline resting values (Table 1, Figures 7a and b). Reparixin treatment diminished the development of autonomic dysreflexia. The average change in MAP during colon distension or skin pinch in SCI rats was reduced by 56–92% in rats that received either low- or high-dose Reparixin treatment after SCI (Table 1, Figure 7b). Similarly, the peak change in MAP induced by colon distension or skin pinch was also reduced by 43–52% after Reparixin treatment (Table 1). Although the average and peak MAP response was diminished, Reparixin treatment had little effect on the average or peak bradycardia response observed during either colon distension or skin pinch (Table 1).
Autonomic neurological outcomes 28 days after SCI. (a) Representative cardiovascular recordings are shown for saline-treated and Reparixin-treated (+R2) SCI rats at rest and during colon distension. The duration of colon distension (60 s) is indicated by a black bar. The MAP and HR are derived from the pulsatile pressure (AP) in the top channel. (b) The change in MAP after skin pinch, or colon distension in saline-treated and Reparixin-treated SCI rats. At least two tests of skin pinch and colon distension were recorded for each animal and averaged. The average±s.e. of each group is shown in bar graph. +R1, 7.5 mg kg–1 Reparixin-treated SCI; +R2=15 mg kg–1 Reparixin-treated SCI; SCI, saline-treated SCI. *Denotes a significant difference from uninjured, P<0.05. φDenotes a significant difference from saline-treated SCI, P<0.05, n=6 animals per group.
Discussion
Selective anti-inflammatory treatments that reduce infiltration and activation of neutrophils and macrophages into the injured spinal cord are consistently associated with sparing of myelinated axons, neuroprotection and improved neurological outcomes.2, 3, 8 The current paper continues this theme and demonstrates that acute treatment with Reparixin, a small molecule antagonist that inhibits CXCR1 and CXCR2 chemokine receptors, improves motor and autonomic neurological outcomes after SCI. The 72-h Reparixin treatment diminished SCI-induced expression of cytokine TNF-α, chemokine CINC-1 and reduced inflammation in the spinal cord lesion. Our results expand upon a 7-day regimen of Reparixin treatment of rats that also demonstrated improved motor function and reduced inflammation after SCI.7
We report the novel finding that Reparixin treatment reduced the expression of Fas and p75 in the SCI lesion to levels comparable to uninjured spinal cord (Figures 3a and b). Both Fas and p75 receptors are implicated in apoptosis and contain intracytoplasmic death domains that activate caspases after SCI.5, 15 Previously, neutralization of the Fas receptor ligand by antibody6 or by soluble Fas receptor infusion5 has been shown to reduce apoptosis, promote regeneration and improve neurological recovery after dorsal column transection or spinal cord clip-compression, respectively. Although the mechanism Reparixin diminished the expression of Fas and p75 receptors is unknown, the inhibited oligodendrocyte apoptosis and preservation of the white matter around the SCI lesion7 could be attributed to reduced levels of Fas and p75. In this paper, we also observed that Reparixin treatment reduced the area of the spinal cord lesion, but also report a neuroprotective benefit as neurons were more abundant near the SCI lesion of Reparixin-treated rats, compared with saline-treated rats (Figure 4). Sparing of the white and gray matter could be expected as Fas is expressed by multiple cell types, including oligodendrocytes, microglia and neurons,6 whereas p75 is predominantly expressed by oligodendrocytes.15 In addition to neutrophils and macrophages, CXCR2 expression has also been reported on neurons and associated with cell survival after brain injury.9 Reparixin treatment could prevent the CINC-1-induced downregulation of neuronal CXCR29 and enhance survival after SCI.
The combined anti-inflammatory and neuroprotective benefits of Reparixin treatment were not only evident upon histopathological examination of the SCI lesion (Figures 4 and 5) but also in improved neurological outcomes of motor and autonomic function (Figures 6 and 7). These improved neurological outcomes can be attributed to sparing of white matter near the lesion and in the neuropil caudal to the lesion. Although locomotion and hindlimb range of motion were modestly improved after Reparixin treatment, the most impressive outcome was the improved regulation of blood pressure. Spinal cord-injured animals receiving the high-dose Reparixin (15 mg kg–1 h–1) treatment demonstrated minimal development of autonomic dysreflexia. This observation is similar to previous reports of modest improvements in motor function, but dramatic improvements in sensory and autonomic neurological outcomes after anti-inflammatory treatment.2, 8
In summary, inhibition of CXCR1 and CXCR2 chemokine receptors by Reparixin is an effective anti-inflammatory and neuroprotective treatment after SCI. Acute treatment of spinal cord-injured rats with Reparixin leads to dramatic improvements in autonomic neurological function and regulation of blood pressure.
References
Kwon BK, Tetzlaff W, Grauer JN, Beiner J, Vaccaro AR . Pathophysiology and pharmacologic treatment of acute spinal cord injury. Spine J 2004; 4: 451–464.
Gris D, Marsh DR, Oatway MA, Chen Y, Hamilton EF, Dekaban GA et al. Transient blockade of the CD11d/CD18 integrin reduces secondary damage after spinal cord injury, improving sensory, autonomic, and motor function. J Neurosci 2004; 24: 4043–4051.
Gonzalez R, Glaser J, Liu MT, Lane TE, Keirstead HS . Reducing inflammation decreases secondary degeneration and functional deficit after spinal cord injury. Exp Neurol 2003; 184: 456–463.
Ghirnikar RS, Lee YL, Eng LF . Chemokine antagonist infusion promotes axonal sparing after spinal cord contusion injury in rat. J Neurosci Res 2001; 64: 582–589.
Ackery A, Robins S, Fehlings MG . Inhibition of Fas-mediated apoptosis through administration of soluble Fas receptor improves functional outcome and reduces posttraumatic axonal degeneration after acute spinal cord injury. J Neurotrauma 2006; 23: 604–616.
Demjen D, Klussmann S, Kleber S, Zuliani C, Stieltjes B, Metzger C et al. Neutralization of CD95 ligand promotes regeneration and functional recovery after spinal cord injury. Nat Med 2004; 10: 389–395.
Gorio A, Madaschi L, Zadra G, Marfia G, Cavalieri B, Bertini R et al. Reparixin, an inhibitor of CXCR2 function, attenuates inflammatory responses and promotes recovery of function after traumatic lesion to the spinal cord. J Pharmacol Exp Ther 2007; 322: 973–981.
Gris D, Marsh DR, Dekaban GA, Weaver LC . Comparison of effects of methylprednisolone and anti-CD11d antibody treatments on autonomic dysreflexia after spinal cord injury. Exp Neurol 2005; 194: 541–549.
Valles A, Grijpink-Ongering L, de Bree FM, Tuinstra T, Ronken E . Differential regulation of the CXCR2 chemokine network in rat brain trauma: implications for neuroimmune interactions and neuronal survival. Neurobiol Dis 2006; 22: 312–322.
Bertini R, Allegretti M, Bizzarri C, Moriconi A, Locati M, Zampella G et al. Noncompetitive allosteric inhibitors of the inflammatory chemokine receptors CXCR1 and CXCR2: prevention of reperfusion injury. Proc Natl Acad Sci USA 2004; 101: 11791–11796.
Weaver LC, Verghese P, Bruce JC, Fehlings MG, Krenz NR, Marsh DR . Autonomic dysreflexia and primary afferent sprouting after clip-compression injury of the rat spinal cord. J Neurotrauma 2001; 18: 1107–1119.
Lindan R, Joiner E, Freehafer AA, Hazel C . Incidence and clinical features of autonomic dysreflexia in patients with spinal cord injury. Parap 1980; 18: 285–292.
Karlsson A-K . Autononomic dysreflexia. Spinal Cord 1999; 37: 383–391.
Eltorai I, Kim R, Vulpe M, Kasravi H, Ho W . Fatal cerebral hemorrhage due to autonomic dysreflexia in a tetraplegic patient: case report and review. Parap 1992; 30: 355–360.
Casha S, Yu WR, Fehlings MG . Oligodendroglial apoptosis occurs along degenerating axons and is associated with FAS and P75 expression following spinal cord injury. Neurosci 2001; 103: 203–218.
Eikard B, Andersen JR . Arrhythmias during halothane anaesthesia II: the influence of atropine. Acta Anaesthesiol Scand 1977; 21: 245–251.
Marsh DR, Weaver LC . Autonomic dysreflexia, induced by noxious or innocuous stimulation, does not depend on changes in dorsal horn substance p. J Neurotrauma 2004; 21: 817–828.
Bao F, Chen Y, Dekaban GA, Weaver LC . Early anti-inflammatory treatment reduces lipid peroxidation and protein nitration after spinal cord injury in rats. J Neurochem 2004; 88: 1335–1344.
Basso DM, Beattie MS, Bresnahan JC . A sensitive and reliable locomotor rating scale for open field testing in rats. J.Neurotrauma 1995; 12: 1–21.
Ditor DS, John S, Cakiroglu J, Kittmer C, Foster PJ, Weaver LC . Magnetic resonance imaging versus histological assessment for estimation of lesion volume after experimental spinal cord injury Laboratory investigation. J Neurosurg Spine 2008; 9: 301–306.
Acknowledgements
This research was funded by the Nova Scotia Heart and Stroke Foundation in a grant to DM. In addition, JF was supported by a research fellowship from the Dalhousie Faculty of Medicine and with funding from Dompé Pharma spa., L’Aquila, Italy. We thank Ricardo Bertini at Dompé Pharma spa. for providing Reparixin for the project and valuable information regarding its appropriate in vivo administration. We also thank Ahmed Ghaly for preparing saline and drug treatments and keeping the code private until results were complete
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Marsh, D., Flemming, J. Inhibition of CXCR1 and CXCR2 chemokine receptors attenuates acute inflammation, preserves gray matter and diminishes autonomic dysreflexia after spinal cord injury. Spinal Cord 49, 337–344 (2011). https://doi.org/10.1038/sc.2010.127
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.127
Keywords
This article is cited by
-
MHC/class-II-positive cells inhibit corticosterone of adrenal gland cells in experimental arthritis: a role for IL-1β, IL-18, and the inflammasome
Scientific Reports (2020)
-
Selection and Prioritization of Candidate Drug Targets for Amyotrophic Lateral Sclerosis Through a Meta-Analysis Approach
Journal of Molecular Neuroscience (2017)
-
Multiple organ dysfunction and systemic inflammation after spinal cord injury: a complex relationship
Journal of Neuroinflammation (2016)