Abstract
This study aimed to clarify the relationship between maternal mortality and advanced maternal age in Japan and to provide useful information for future perinatal management. Maternal death rates by age group were investigated for all maternal deaths in Japan for an 11-year period, from 2010 to 2021. Maternal deaths among those aged ≥ 40 years were examined in detail to determine the cause, and the number of deaths by cause was calculated. The causes of onset of the most common causes of death were also investigated. The maternal mortality rates were 0.8 (95% confidence interval [CI] 0.3–4.7) for < 20 years, 2.6 (95% CI 1.7–3.8) for 20–24 years, 2.9 (95% CI 2.3–3.6) for 25–29 years, 3.9 (95% CI 3.3–4.5) for 30–34 years, 6.8 (95% CI 5.9–7.9) for 35–39 years, and 11.2 (95% CI 8.8–14.3) for ≥ 40 years of age. Patients who were ≥ 40 years of age had a significantly higher mortality rate compared to that in other age groups. Hemorrhagic stroke was the most common cause of death in patients aged ≥ 40 years (15/65 [23%]), and preeclampsia (8/15 [54%]) was the most common cause of hemorrhagic stroke. Maternal mortality is significantly higher in older than in younger pregnant women in Japan, with hemorrhagic stroke being the most common cause of maternal death among women > 40 years of age. More than half of hemorrhagic strokes are associated with hypertension disorder of pregnancy. These facts should be considered by women who become pregnant at an advanced age and by healthcare providers involved in their perinatal care.
Similar content being viewed by others
Introduction
There has been an increase in the number of older women who are pregnant, and advanced maternal age (AMA) has been increasing yearly worldwide1,2,3,4,5. With increasing age of pregnancy, there is an increase in various maternal complications5,6,7. A study done in Japan reported that AMA increases the need for cesarean section and the risk for preeclampsia, placenta previa, and preterm delivery6. It has also been reported that AMA increases the risk of cervical incompetence, gestational diabetes, preterm water breaking, and preterm delivery5,7.
AMA has been reported to increase various maternal complications as well as maternal mortality3. It is predicted that the number of pregnancies at older ages will increase in the future owing to advances in assisted reproductive technologies and lifestyle changes. However, the relationship between age and maternal mortality in Japan has never been studied. This study aimed to clarify the relationship between maternal mortality and AMA in Japan and to provide useful information that will contribute to future perinatal management.
Materials and methods
Maternal mortality data
All maternal deaths in Japan during the 11-year period from 2010 to 2021 were included. Information on maternal deaths was obtained from data registered in the Japan Maternal Death Exploratory Committee (JMDEC) of the Japan Association of Obstetricians and Gynecologists (JAOG), which was launched in 2010 and covers all maternal deaths in Japan8.
The JMDEC consists of 15 obstetricians, four anesthesiologists, two emergency physicians, two pathologists, and medical specialists and forensic experts. The registration system has been described in previous reports8,9,10,11,12,13,14,15,16,17.
When a maternal death occurs, the attending physician registers the case with the Japanese Society of Obstetrics and Gynecology and sends a report to the JAOG. The report consists of 22 pages and approximately 100 questions and is intended to elicit detailed information about the clinical course, facility characteristics, and staff who participated in the patient's care, along with medical records such as anesthesia records, medical images, laboratory data, pathology reports, and autopsy reports.
All personal information contained in reports and medical records, such as maternal characteristics, clinicians, and facility geography, are anonymized in the JAOG. All of these anonymized data from across Japan are sent to the JMDEC, where they are analyzed and discussed at the JMDEC's monthly meetings regarding factors associated with maternal mortality and the circumstances of death.
Age groups
Registered maternal deaths were categorized by age: < 20, 20–24, 25–29, 30–34, 35–39, and ≥ 40 years, and the maternal mortality rate was calculated for each age group.
Maternal mortality rates were also calculated for each age group by the major cause of death in Japan. Maternal mortality rate is the number of maternal deaths per 100,000 births. No statistical adjustment was made because the population was almost exclusively Japanese, there were no racial differences, and there was no disparity in access to medical care due to the national medical insurance and free maternal health checkup systems.
Maternal deaths among pregnant women aged 40 years and older
Maternal deaths among women aged ≥ 40 years were examined in detail to determine the causes of death, and the number of deaths by cause was calculated. The causes of onset were also investigated for diseases leading to the highest number of deaths.
Statistical analysis
Statistical analyses were performed to determine perinatal mortality using JMP 13.2.0 (SAS Institute Inc., Cary, NC, USA). Unless otherwise specified, univariate statistics and 95% confidence intervals (CI) were evaluated for the primary endpoint, perinatal mortality. Comparisons of perinatal mortality were performed using the Mann–Whitney U test. Statistical significance was set at p < 0.05. The Mann–Whitney U test was used for two-group comparisons and adjustments for multiple comparisons were made using the Bonferroni test. P-values for comparisons of maternal mortality rates between age groups were calculated using the Kruskal–Wallis test. P-values for maternal mortality rate comparisons between the 40 years and older and other age groups for each cause of death were calculated using the Mann–Whitney U test and adjusted for using the Bonferroni test.
Ethics approval and consent to participate
This study was approved by the ethics boards of the National Cerebral and Cardiovascular Center, Osaka, Japan, and JAOG. This study was conducted in accordance with the principles of the Declaration of Helsinki. Informed consent was not obtained from patients or their families because this study was based on the analysis of institutional forms, and patient records and information were anonymized prior to the analysis. Additionally, under the conditions of approval for "medical and biological research involving human subjects" in Japan informed consent was not required for this study18, and JAOG approved that informed consent was not required for this study.
Results
Overall maternal deaths and international classification of diseases maternal mortality (ICD-MM) classification system
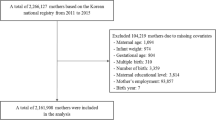
Between 2010 and 2021, 512 maternal deaths were registered in the Maternal Death Registration Project. The number of births in Japan during the same period was 11,557,975 cases. Of the 512 maternal deaths, 335 (65.4%) were direct deaths and 150 (29.3%) were indirect deaths. Twenty-seven (5.3%) were unclassifiable.
Overall, 497/512 (97.1%) cases could be classified according to the World Health Organization (WHO) ICD-MM. The breakdown of the classification is as follows: Group 1, 4 cases (0.8%); Group 2, 47 cases (9.5%); Group 3, 88 cases (17.7%); Group 4, 28 cases (5.6%); Group 5, 126 cases (27.3%); Group 6, 8 cases (1.6%); Group 7, 133 cases (26.8%); Group 8, 45 cases (9.1%); and Group 9, 8 cases (1.6%).
Number of deaths and maternal mortality rates by age group
The number of maternal deaths by age group was as follows: < 20 years, 1 case; 20–24 years, 26 cases; 25–29 years, 89 cases; 30–34 years, 161 cases; 35–39 years, 176 cases; and 40 years, 65 cases (Fig. 1A).
Maternal mortality rates by age group are shown in Fig. 1B. The maternal mortality rates were 0.8 (95% CI 0.3–4.7) for those < 20 years, 2.6 (95% CI 1.7–3.8) for those 20–24 years, 2.9 (95% CI 2.3–3.6) for those 25–29 years, 3.9 (95% CI 3.3–4.5) for those 30–34 years, 6.8 (95% CI 5.9–7.9) for those 35–39 years, and 11.2 (95% CI 8.8–14.3) for those ≥ 40 years of age. Pregnant women ≥ 40 years of age had significantly higher mortality rates compared to that in other age groups (P < 0.01). The maternal mortality rates by cause are shown in Table 1.
Maternal mortality in the 40 years and older group
Table 2 and Fig. 2 shows the background data and the number of cases of maternal mortality among those aged ≥ 40 years. The most common cause of death was hemorrhagic stroke (15/65 [23%]), followed by obstetric hemorrhage (8/65 [12%]) and suicide (8/65 [12%]). The maternal mortality rates of hemorrhagic stroke, pulmonary thromboembolism, and suicide were significantly higher among those aged ≥ 40 years than among the other age groups (P < 0.01 for hemorrhagic stroke, pulmonary thromboembolism, and suicide). Figure 3 shows a breakdown of the causes of hemorrhagic stroke, the most common cause of death. The most common causes of hemorrhagic stroke were preeclampsia (8/15 [54%]), cerebral aneurysm (2/15 [13%]), cerebral arteriovenous malformation (2/15 [13%]), moyamoya disease (1/15 [7%]), and unknown (2/15 [13%]).
Discussion
This study is the first to report on the relationship between age and maternal mortality in Japan. Two important new findings were extracted from the present study. First, AMA in Japan was found to be associated with a significantly higher maternal mortality rate than that noted among pregnancies at a younger age in this study. Previous studies have also reported that an increase in maternal age is associated with an increase in various obstetric complications and maternal mortality19,20,21. The results of the present study are similar to those previously reported. However, Maternal mortality was notably lower among women younger than 20 years of age, a point of difference. Second, this is a clarification of the causes of maternal mortality among women over 40 years of age.
Although the rate of chronic diseases, such as malignant, cardiovascular, and renal diseases, as comorbidities is increased among AMA cases22, the rate of their involvement as a cause of death was low. The most common cause of death in the AMA group in this study was hemorrhagic stroke. The association of hemorrhagic stroke, rather than stroke, with maternal mortality is a problem unique to Asian populations23,24, and more than half of the deaths due to hemorrhagic stroke were associated with preeclampsia. In general, the overall incidence of preeclampsia is reported to be 3–4% but increases to 5–10% in those aged 40–49 years and to 35% in those aged > 50 years25. In addition, at ≥ 40 years, the relative risk of mortality was reported to be 1.68 (95% CI 1.23–1.39) for first-time mothers26. It is clear that the incidence of preeclampsia increases in AMA cases27. Older Japanese and Asian pregnant women are more likely to develop hemorrhagic stroke28,29, and adequate attention should be paid to the development of hemorrhagic stroke due to preeclampsia. Further, in Asian populations, uterine artery Doppler, angiogenesis factors, and aspirin therapy should be used to monitor and prevent the occurrence of hypertensive nephropathy in pregnant women > 40 years old.
Among assisted reproductive therapies, frozen-thawed embryo transfer and egg donation in particular have been reported to be risk factors for preeclampsia30,31. In the present study, the proportion of maternal mortality cases at age ≥ 40 years among those who had undergone assisted reproductive therapy was low. In addition, there were no cases of maternal mortality due to hemorrhagic stroke caused by preeclampsia among assisted reproductive therapy-induced pregnancy cases. The proportion of assisted reproductive technology-induced pregnancies in Japan is expected to increase in the future, as increasing age increases the dependence on assisted reproductive technology. Therefore, it is important to be aware of the possibility of developing preeclampsia after the use of assisted reproductive technology.
In addition to hemorrhagic stroke, pulmonary thromboembolism, infectious diseases, cardiovascular diseases, and suicide significantly increased maternal mortality in older pregnant women, suggesting that we should not focus solely on hemorrhagic stroke as a cause of maternal mortality.
This study showed that the maternal mortality rate increased with AMA in Japan. This is consistent with reports from other developed countries3,32. However, other developed countries have higher rates of maternal mortality among young women as well as among AMA cases, indicating a bimodal nature of this association, while the maternal mortality rate among women aged < 20 years in Japan was low. In the United Kingdom, the maternal mortality rate among pregnant women aged 20–29 years is the lowest, and the maternal mortality rates for pregnancies among those < 20 years of age and ≥ 30 years increased compared to those among pregnant women in their 20 s3. In addition, Japan provides generous medical insurance coverage to all citizens regardless of the financial status. During pregnancy, women are given a medical checkup slip almost free of charge and can visit a hospital every four weeks in the first trimester, every two weeks in the second trimester, and every week in the last trimester of pregnancy. Further, the groups enrolled in this study were almost exclusively Japanese, which provided a sample cohort that is less prone to biases other than age.
The limitations of this study include, first, that it was a mono-ethnic study and did not adjust the maternal mortality rates for several confounding factors, although the Japanese insurance system provides a background for the uniform provision of medical care. Second, although we had detailed data on deaths, we did not have detailed data on survivors. Third, we did not have information on hospital resources, infrastructure, and staff that contribute to maternal mortality and risk. It is not possible to determine whether high-risk women benefit from being in a particular healthcare setting. Fourth, because of the relatively low maternal mortality rates, the denominators for some of the groups were relatively small, making it impossible to make meaningful comparisons between the groups in terms of mortality rates.
In conclusion, maternal mortality increased proportionally with age in Japan. In particular, the mortality rate was 2.3 times higher for those aged ≥ 40 years than for those aged 35–39 years. In addition, hemorrhagic stroke was the most common cause of maternal mortality among those aged ≥ 40 years, and more than half of the hemorrhagic strokes were associated with preeclampsia. These facts should be considered by women who become pregnant at an advanced age and by healthcare providers involved in their perinatal care.
Conclusion
Maternal mortality rates were significantly higher among older pregnant women than among younger pregnant women in Japan, with hemorrhagic stroke being the most common cause of maternal death among women > 40 years of age. More than half of the hemorrhagic strokes were associated with preeclampsia. These facts should be considered by women who become pregnant at an advanced age and by healthcare providers involved in their perinatal care.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Ministry of Health, Labour and Welfare. Special Report on Demographic Statistics. Update 2021. Accessed 20 October 2022. https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/tokusyu/syussyo07/dl/gaikyou.pdf
Singh, G. K. Trends and social inequalities in maternal mortality in the United States, 1969–2018. Int. J. MCH. AIDS. 10, 29–42 (2021).
Mothers and Babies: Reducing Risk through Audlts and Confidential Enquiries across the UK (MBRRACE-UK). Saving Lives, Improving Mothers’ Care -Lessons learned to inform maternity care from the UK and Ireland Confidential Enquiries into Maternal Deaths and Morbidity 2017–19, accessed 20 October 2022. https://hubble-live-assets.s3.amazonaws.com/birth-companions/file_asset/file/452/MBRRACE-UK_Maternal_Report_2021_-_FINAL_-_WEB_VERSION.pdf
Lim, J. W. The changing trends in live birth statistics in Korea, 1970 to 2010. Korean J. Pediatr. 54, 429–435 (2011).
Koo, Y. J. et al. Pregnancy outcomes according to increasing maternal age. Taiwan J. Obstet. Gynecol. 51, 60–65 (2012).
Ogawa, K. et al. Association between very advanced maternal age and adverse pregnancy outcomes: a cross sectional Japanese study. BMC Pregnancy Childbirth. 17, 349 (2017).
Luke, B. & Brown, M. B. Contemporary risks of maternal morbidity and adverse outcomes with increasing maternal age and plurality. Fertil. Steril. 88, 283–293 (2007).
Hasegawa, J. et al. Decline in maternal death due to obstetric haemorrhage between 2010 and 2017 in Japan. Sci. Rep. 30(9), 11026 (2019).
Hasegawa, J. et al. Maternal deaths in Japan due to abnormally invasive placenta. Int. J. Gynaecol. Obstet. 140, 375–6 (2018).
Hasegawa, J. et al. How should maternal death due to suicide be classified? Discrepancy between ICD-10 and ICD-MM. BJOG Int. J. Obstet. Gynaecol. 127, 665–7 (2020).
Katsuragi, S. et al. Perinatal outcome in case of maternal death for cerebrovascular acute disorders: a nationwide study in Japan. J Matern Fetal Neonatal Med. 35, 2429–34 (2022).
Tanaka, H. et al. Maternal death related to sudden unexpected death in epilepsy: A nationwide survey in Japan. Brain Sci. 11, 995 (2021).
Hasegawa, J. et al. Maternal death due to stroke associated with pregnancy-induced hypertension. Circ J. 79, 1835–40 (2015).
Hasegawa, J. et al. Maternal death due to serious group a streptococcal toxic shock syndrome reduced after the coronavirus disease pandemic in Japan. J. Matern. Fetal. Neonatal. Med. 35, 10451–10454 (2022).
Tanaka, H. et al. Increase in maternal death-related venous thromboembolism during pregnancy in Japan (2010–2013). Circ. J. 79, 1357–1362 (2015).
Tanaka, H. et al. Value of fibrinogen in cases of maternal death related to amniotic fluid embolism. J. Matern. Fetal. Neonatal. Med. 30, 2940–2943 (2017).
Tanaka, H. et al. The increase in the rate of maternal deaths related to cardiovascular disease in Japan from 1991–1992 to 2010–2012. J. Cardiol. 69, 74–78 (2017).
Eba, J. & Nakamura, K. Overview of the ethical guidelines for medical and biological research involving human subjects in Japan. Jpn. J. Clin. Oncol. 52, 539–544 (2022).
Naeye, R. L. Maternal age, obstetric complications, and the outcome of pregnancy. Obstet. Gynecol. 61, 210–216 (1983).
Frederiksen, L. E. et al. Risk of adverse pregnancy outcomes at advanced maternal age. Obstet. Gynecol. 131, 457–463 (2018).
Sheen, J. J. et al. Maternal age and risk for adverse outcomes. Am. J. Obstet. Gynecol. 219(390), e1-15 (2018).
Ervin, R. B. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl. Health Stat. Report. 13, 1–7 (2009).
Takahashi, J. C. et al. Pregnancy-associated intracranial hemorrhage: Results of a survey of neurosurgical institutes across Japan. J. Stroke Cerebrovasc. Dis. 23, e65-71 (2014).
Enomoto, N. et al. Pregnancy-associated hemorrhagic stroke: A nationwide survey in Japan. J. Obstet. Gynaecol. Res. 47, 2066–2075 (2021).
Yogev, Y. et al. Pregnancy outcome at extremely advanced maternal age. Am. J. Obstet. Gynecol. 203(558), e1-7 (2010).
Duckitt, K. & Harrington, D. Risk factors for pre-eclampsia at antenatal booking: Systematic review of controlled studies. BMJ 330, 565 (2005).
Khalil, A., Syngelaki, A., Maiz, N., Zinevich, Y. & Nicolaides, K. H. Maternal age and adverse pregnancy outcome: A cohort study. Ultrasound Obstet. Gynecol. 42, 634–643 (2013).
Tang, C. H. et al. Preeclampsia-eclampsia and the risk of stroke among peripartum in Taiwan. Stroke 40, 1162–1168 (2009).
Yoshida, K. et al. Strokes associated with pregnancy and puerperium: A nationwide study by the Japan stroke society. Stroke 48, 276–282 (2017).
Ishihara, O. et al. Impact of frozen-thawed single-blastocyst transfer on maternal and neonatal outcome: An analysis of 277,042 single-embryo transfer cycles from 2008 to 2010 in Japan. Fertil. Steril. 101, 128–133 (2014).
Malchau, S. S. et al. Perinatal outcomes in 375 children born after oocyte donation: A Danish national cohort study. Fertil. Steril. 99, 1637–1643 (2013).
Burgess, A. P. H. et al. Pregnancy-related mortality in the United States, 2003–2016: Age, race, and place of death. Am. J. Obstet. Gynecol. 222, 489.e1-489.e8 (2020).
Author information
Authors and Affiliations
Contributions
H.T. had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: H.T. Acquisition, analysis, or interpretation of data: H.T. and J.H. Drafting of the manuscript: H.T., K.T. Critical revision of the manuscript for important intellectual content: T.A., M.N., E.H., M.N., A.S., and I.I. Statistical analysis: H.T., S.K., K.T. Administrative, technical, or material support: H.T., T.A., M.N., E.H., M.N., A.S., and I.I. Supervision: S.K., T.A., M.N., E.H., M.N., T.M., A.S., I.I., and T.I. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tanaka, H., Hasegawa, J., Katsuragi, S. et al. High maternal mortality rate associated with advanced maternal age in Japan. Sci Rep 13, 12918 (2023). https://doi.org/10.1038/s41598-023-40150-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-40150-4
This article is cited by
-
Maternal preconception blood pressure and the association with preterm birth
Hypertension Research (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.