Abstract
Decreased albumin levels are common in congestive heart failure (CHF), but little is known about its role in mortality risk in CHF. This study developed a cohort prediction model based on 7121 individuals with heart failure to evaluate the short-term mortality and prognostic role of albumin in patients with CHF. The cohort was from intensive care unit between 2001 and 2012 in a publicly available clinical database in intensive care called MIMIC III. We used a generalized additive model to determine the nonlinear correlation between serum albumin and 14th day, 28th day and 90th day all-cause mortality in patients with heart failure. The results showed that serum albumin is an independent risk factor for 14th, 28th and 90th day all-cause mortality, and has a linear relationship with all-cause mortality in congestive heart failure. Cox regression analysis using restricted cubic spline with albumin as continuous parameter showed that the decrease of albumin level is directly related to the increase of mortality (14th day mortality: hazard ratio [HR], 0.65 [95% CI, 0.58 to 0.73]); 28th day mortality: HR, 0.56 [95% CI, 0.51 to 0.63]; 90th day mortality: HR, 0.52 [95% CI, 0.47 to 0.57]; P for trend < 0.001). The multivariate adjusted association between albumin (as a continuous variable) and all-cause mortality on the 90th days is mixed by ARDS [HR, 0.64, 95% CI (0.47–0.87), P = 0.005]. The all-cause mortality on the 90th day predicted better clinical results with the all-cause mortality on the 14th day.
Similar content being viewed by others
Introduction
Heart failure (HF), a major epidemic and public health burden, associated with considerable morbidity and mortality1. In the United States, approximately 10–51% of hospitalized patients with HF were reported to be admitted to the ICU, with a mortality rate of 10.6%2,3,4. Inadequate cardiac output may result in congestive heart failure (CHF), which is a pathological condition that impairs tissue and organ perfusion and metabolic activity. Because of the higher in-hospital mortality in ICU-treated HF patients, accurate prognosis prediction and close follow-up may be more beneficial for ICU-treated HF patients.
Hypoalbuminemia is highly prevalent in patients with systolic heart failure, which occurs in about one-third of patients5. Hypoalbuminemia in HF patients may be caused by hemodilution, malnutrition, chronic inflammation, infection, proteinuria and other mechanisms5. Meanwhile, hypoalbuminemia may leads to the decrease of colloid osmotic pressure and affect the degree of pulmonary congestion and the symptoms of heart failure6. In addition, hypoalbuminemia is known to be associated with poor prognosis for end-stage renal disease, infection and cancer, as well as in the elderly7. Therefore, Serum albumin levels may be a predictor of mortality in HF patients in the ICU. Tamara B et al.8,9 found that comparison to patients without hypoalbuminemia, the risk of death in patients suffering late systolic HF with hypoalbuminemia increased by more than 2 times. Israel G et al.10 found that the decrease of albumin was an independent predictor of mortality. The upward trend of serum albumin in patients with acute heart failure is related to a good long-term prognosis11. Albumin is a protective factor for in-hospital or long-term mortality of patients with heart failure. However, to our best knowledge, there is an unclear conclusion about the short-term mortality of systolic heart failure.
Although a variety of in-hospital mortality prediction models are currently available, none of these methods have satisfactory accuracy and have not been widely used12,13,14. In addition, there are limited data on predictive models for the association of serum albumin levels with mortality in ICU-treated HF patients. Therefore, we used data from the MIMIC III database to develop a predictive model of serum albumin levels and short-term mortality from systolic heart failure in the intensive care unit (ICU).
Methods
Data base
Our research was based on an open intensive care clinical database named Multi-parameter Intelligent Monitoring III15. The database included more than 40,000 intensive care patients admitted to Beth Israel Deaconess Medical Center (Boston, Massachusetts, USA) from 2001 to 2012. In order to apply for access to the database, we completed the online course of the National Institutes of Health in the United States and passed the test of human protection research participants (No.6182750). The project was approved by Beth Israel Deaconess Medical Center and the Institutional Review Committee of Massachusetts Institute of Technology (Cambridge, Massachusetts). In order to protect the privacy of patients, the data was de-identified. Therefore, informed consent was abandoned.
Study population
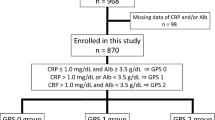
Using ICD-9 disease codes, we analyzed the database for adult CHF patients at the time of first ICU admission. Patients with CHF diagnostic criteria of the European Society of Cardiology (ESC) will be included16. This standard is also based on the typical symptoms, signs and structural or functional abnormalities of the heart during echocardiography. Exclusion criteria include patients who are younger than 18 years old, stay in ICU for less than 24 h or have no corresponding laboratory test results or data needed for research (Fig. 1). We extracted clinical variables, including demographic characteristics, ICD-9 code, physiological indicators, drugs and laboratory tests. Because the birthdate of patients over the age of in the database was accurately moved to 300 years ago to cover their age, it was modified (age −300 + 89) before the analysis. All scores were based on the lowest difference of relevant data within 24 h in ICU. Patients who had been admitted to intensive care unit for many times only include their initial admission results.
Exposure and outcomes
The main exposure was mean serum albumin, baseline albumin, maximum albumin and minimum albumin value, in which 7121 participants were measured. As the four albumin levels have basically the same trend on short-term death (data have been presented in supplementary data), the average albumin was selected to represent the correlation between albumin and short-term death in this study (Fig. S1-6,Table S1-3). The mortality on the 14th, 28th and 90th day following admission to ICU was selected as the primary endpoint, and the mortality of ICU was determined only by the first admission to ICU.
Covariates
Use PostgreSQL (version 9.6) Structured query language for extracting data from MIMIC III. Demography, vital signs, laboratory tests, complications, scoring system and other variables collected 24 h before admission to intensive care unit were taken from MIMIC III. Co-diseases include coronary artery disease, hypertension, acute respiratory distress syndrome, diabetes, cigarette, alcohol abuse, chronic obstructive pulmonary disease, BNP, LVEF, diuretic, ACEI/ARB/ARNI and cardiac glycoside.
Statistical analysis
Descriptive statistics were summarized as the average and standard deviation or median of continuous variables (quartile distance), and frequency distribution was expressed as a percentage of classified variables. Chi-square test, one-way ANOVA and Kruskar-Wallis H test were used to determine the significant differences among groups. Generalized additive model (GAM) was used to determine the non-linear relationship between serum albumin and all-cause mortality. Cox proportional risk model was used to determine the relationship between albumin level and mortality of congestive heart failure at the 14th, 28th and 90th day. These results were expressed by the risk ratio of 95% CI. Multiple imputation was used to deal with the missing data.
The timing of events was analyzed to check the outcome risk of albumin quartile (the lowest quartile in the reference group). In Cox model, the statistical interaction between serum and ARDS was tested by multiplying the interaction term. Less than 10% of the covariant data was lost, so we didn't use interpolation technology. The proportional risk hypothesis was evaluated in all models by Kolmogorov-type supremum test. The main follow-up of the analysis focused on the all-cause mortality results of the 14th, 28th and 90th day in the intensive care unit. According to ARDS subgroup analysis, Wald statistics of cross product terms of trend variables and subgroup members were used to test the heterogeneity among subgroups. All probability values were bilateral, and values less than 0.05 were considered statistically significant. R (http://www.R-project.org) was used for all statistical analysis.
Result
Baseline characteristics
A total of 7121 patients participated in this study. Table 1 lists the baseline characteristics of the study population according to average albumin level. The patients were characterized by more advanced in age, with more males than females. Heart rate, respiratory rate, platelet, creatinine, leukocyte, aspartate transaminase (AST), hypertension and acute respiratory distress syndrome (ARDS) in patients with high average serum albumin were lower than those in patients with low average albumin, while systolic blood pressure, diastolic blood pressure, mean arterial pressure, hemoglobin, diabetes and coronary heart disease (CHD) were higher than those in patients with low albumin (as shown in Table 1).
Survival analysis
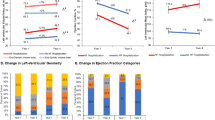
All-cause mortality was 12.5%, 16.8% and 18.4% on the 14th, 28th and 90th day after admission, respectively (Table S4). As shown in Kaplan–Meier survival curves in Fig. 2 and Table 2, unadjusted and multivariate adjusted risk ratios and 95% CI calculated according to average albumin and quartiles as continuous variables. The results showed that the average albumin as a continuous variable was related to all-cause mortality at the 14th day, 28th day and 90th day(HR 0.58, 95% CI0.53–0.64, P < 0.0001; HR0.49, 95% CI 0.45–0.54, P < 0.0001; HR0.46 ,95% CI 0.42–0.50, P < 0.0001). For every standard deviation increase of albumin, the all-cause mortality decreased by 42%, 51% and 54% on 14th, 28th and 90th days. After adjustment of heart rate, SBP, mean arterial pressure, diastolic pressure, breathe rate, temperature, SPO2, platelet, potassium, sodium, creatinine, hemoglobin, WBC, AST, BNP, LVEF, diuretic, ACEI/ARB/ARNI and cardiac glycoside, the correlation between average albumin and all-cause mortality was weakened as a continuous variable and quartile(continuous variable:HR 0.64, 95% CI 0.58–0.71, P < 0.0001; HR 0.56 95% CI 0.51–0.61, P < 0.0001;HR 0.52,95% CI 0.48–0.57, P < 0.0001). For every standard deviation increase of albumin, the all-cause mortality decreased by 36%, 44% and 48% on 14th, 28th and 90th days. ARDS significantly confuses the relationship between average albumin (as a continuous variable) and all-cause mortality. The results of P value for trend showed that all-cause mortality decreased with the increase of average albumin on the 14th, 28th and 90th day.
Kaplan–Meier chart of probability of cumulative hazard among the different average albumin levels. (A) Kaplan–Meier chart of probability of 14th day survival among the different albumin levels. (B) Kaplan–Meier chart of probability of 28th day survival among the different albumin levels. (A) Kaplan–Meier chart of probability of 90th day survival among the different albumin levels.
After adjusting the covariates of heart rate, SBP, mean arterial pressure, diastolic pressure, respiratory rate, temperature, SPO2, platelet, potassium, sodium, creatinine, hemoglobin, WBC, AST, BNP, LVEF, diuretic, ACEI/ARB/ARNI and cardiac glycoside, we observed that there was a linear relationship between average albumin level and all-cause mortality on 14th, 28th and 90th day (HR 0.63 95%CI 0.46–0.67, P < 0.0001; HR 0.59 95% CI 0.58–0.68, P < 0.0001; HR 0.52 95% CI 0.43–0.61, P < 0.0001) (Fig. 3). For every quartile standard deviation increase of average serum albumin level, all-cause mortality on the 14th, 28th and 90th day decreased by 24%, 31% and 35% compared with Q1(≤ 0.94dg/ml) (Table 2). In addition, we also found that the threshold of 3.56 mg/dl was related to different death risks, that is, the death risk of average albumin below 3.56 mg/dl was lower than that of average albumin above 3.56 mg/dl (Table S5).
Restricted cubic spline curve showing the adjusted hazard ratios for all-cause mortality as a function of average albumin concentration. Albumin as a continuous variable, model adjusted for heart rate; SBP; mean arterial pressure; diastolic pressure; respire rate; temperature; SPO2; platelet; potassium; sodium; creatinine; hemoglobin; WBC; AST, BNP, LVEF, diuretic, ACEI/ARB/ARNI, cardiac glycoside. At the figure, the frequency distribution of albumin is shown.
The multivariate adjusted association between average albumin (as a continuous variable) and all-cause mortality at the 14th and 28th day is mixed by ARDS(P value of 14th day = 0.0003, P value of 28th day = 0.0092, P value of 90th day = 0.0412) (Table S6). It was found that average albumin, as far as the participants without ARDS were concerned, had a more obvious negative correlation with all-cause mortality on the 14th and 28th day (Figure S7). However, for patients with ARDS, average albumin had no obvious correlation with all-cause mortality on the 14th and 28th day after adjusting the covariates of heart rate, SBP, mean arterial pressure, diastolic pressure, respiratory rate, temperature, SPO2, platelet, potassium, sodium, creatinine, hemoglobin, WBC, AST, BNP, LVEF, diuretic, ACEI/ARB/ARNI and cardiac glycoside (HR 1.04 95% CI 0.80–1.35, P = 0.7858; HR 0.77 95% CI 0.55–1.08, P = 1344). However, the negative correlation between average albumin and the 90th day mortality was not affected by ARDS (HR 0.64 95% CI 0.47–0.87, P = 0.0047) (Table S7).
Discussion
The three main findings of this study of serum average albumin level in 7121 intensive care unit patients with congestive heart failure were: (1) Higher average albumin level was found to be independently associated with a higher risk of 14th, 28th and 90th day all-cause mortality in CHF patients through the continuous follow-up. Especially when the average albumin level was above 3.56 mg/dl, the risk of death on 14th day was lower. (2) The negative association between albumin (as a continuous variable) and all-cause mortality at the 14th and 28th day was mixed by ARDS. (3) P value for trend was used to statistically test this trend, and Change Per Quartile was used to further quantify this trend.
In the case of acute HF, albumin has been proved to have an important influence on survival17,18,19. Although multiple risk grading models and HF prognostic scores have been proposed and validated, the role of SA has not been investigated12,20. In a recent meta-analysis, Peng et al.21 found that HA was associated with increased mortality in heart failure. In addition, Mahmoud et al.22 found that in-hospital mortality in HF was inversely associated with SA. SA showed a decreasing trend and was associated with worse prognosis in acute and chronic HF23,24. Jabbour et al.25 followed 212 patients with chronic systolic HF for more than 2 years and found that SA reduction from baseline was associated with higher mortality compared with retention of baseline SA. A study by Biegus et al.23 showed that a decreasing trend in SA during the first 4 days of hospitalization was associated with increased mortality at 6 months, and the risk was proportional to the degree of albumin reduction. However, few study surveyed the magnitude and direction of the association between the albumin and mortality continually. Our study revealed linear association between serum albumin and all-cause mortality on 14th, 28th, and 90th days in patients with congestive heart failure respectively. In addition, a study has found that serum albumin levels < 3 mg/dL were associated with decreased renal function during treatment in patients with acute HF26. We found the risk of all-cause mortality on day 14 was significantly reduced when albumin was increased above 3.56 mg/dl, which may provide a theoretical reference value for clinical treatment.
Low albumin in patients with heart failure is mainly manifested by reduced albumin synthesis and protein loss, which may be caused by hemodilution, chronic inflammatory states, hepatic congestion, malnutrition, cachexia due to volume overload, and proteinuria or intestinal disease. Albumin is associated with numerous detrimental biological processes which are present in HF and pertain to a worse outcome27. Low albumin in heart failure promotes and aggravates congestion due to the decrease of intravascular colloidal osmotic pressure28, the increases of oxidative stress29, inflammation30, and susceptibility to infection. The mechanism may be supposed that S-thiolation of albumin is increased in the plasma of HF patients and induced changes in the structure and antioxidant function of human serum albumin, and provide a new paradigm of the proinflammatory effect of S-thiolation HAS31. Therefore, low albumin is the sum of many harmful factors in patients with heart failure, which is expected to provide important prognostic information for patients with heart failure.
Our findings suggested that ARDS and albumin interacted in the prediction of results. Previous studies have found that hypoproteinemia (< 5.9 g/dl) and hypoproteinemia level < 2.4 g/dl were considered as signs of increased lung permeability in patients with sepsis and acute respiratory distress syndrome. The lung leakage index would decrease with the rise of serum protein32. In-depth analysis of the results showed that the decrease of colloidal osmotic pressure under normal permeability of vascular endothelium would not cause edema. On the contrary, it was the increased permeability caused by endothelial damage that leads to hypoproteinemia32. The increase of systemic permeability caused by low albumin can’t be equated with similar pulmonary vascular permeability. Besides, on the day of admission to ICU, serum albumin has nothing to do with the degree of pulmonary degassing described by LUSS in ARDS patients. Serum albumin level < 3.25 g/dL increases the chances of prolonging ICU stay (≥ 10 days), but it cannot predict the mortality rate33. This is also consistent with our conclusion, suggesting that ARDS may be the main risk of all-cause death on the 28th day. Therefore, albumin reduction in patients with initial heart failure may be largely influenced by other factors such as inflammation. In our research, we found that there is a special population in the linear relationship between albumin and all-cause mortality, and the special population refers to the patients with heart failure complicated with ARDS. In patients with heart failure complicated with ARDS, the predictive effect of albumin on all-cause mortality is greatly reduced, and the reason may be related to the close relationship among infection, low albumin and ARDS.
An interesting finding in this study is the extent to which albumin level change over time to the recent death of congestive HF. The all-cause mortality on the 90th day predicted better clinical results with the all-cause mortality on the 14th day. A significantly different finding was reported in the case of chronic HF25,34. This finding seems to be biologically unreasonable, as the decline of albumin over time is the characteristic of the degradation state of HF patients. However, the condition of patients tends to be stable after staying in ICU for 14 days, and the mortality is obviously decreasing due to the different death time ranges of our follow-up. This means that in acute cases, these changes are related to the severity, sequelae and progress of acute events. In the chronic environment, these changes may reflect the progress of chronic diseases of albumin, the harmful biological process related to low albumin and its significance to prognosis34.
Whether high albumin can effectively reduce the all-cause mortality of congestive HF requires a sufficiently powerful placebo-controlled randomized controlled trial, but there are few studies on whether albumin supplementation can reduce the all-cause death of congestive heart failure patients in intensive care unit, most of them are only observational studies. Experiments showed that administration of albumin would not change the length of stay or mortality of patients in intensive care unit35,36. It seems unreasonable that exogenous albumin is expensive to treat hypoalbuminemia. But maybe exogenous albumin cannot stay in the body for a long time.
The most important limitation of our study is related to observation design, which makes it impossible to infer the causal relationship between the observed association between serum albumin and all-cause mortality. Even after multivariable adjustment, residual confusion remains an issue. In addition, there is a lack of the stage of heart failure and the mechanism of death not be assessed. Thirdly, low albumin levels are caused by hemodilution, chronic inflammatory states, hepatic congestion, malnutrition, cachexia due to volume overload, and proteinuria or intestinal disease, there is a deficiency in this study because of the limitation of the database. Fourthly, Because of the limitations of the database, the confounding factors, including acute decompensated heart failure, acute pulmonary edema, cardiogenic shock, acute coronary syndrome complicated by heart failure, were not enrolled in the study. Moreover, further studies are needed to take the influence of low albumin on the pharmacokinetic of the drugs into account. Nevertheless, our advantage lies in the discussion of short-term all-cause mortality, and the serum albumin level has no obvious change with time. We also believe that it is the first time that we have continuously followed up all-cause mortality for 14th, 28th and 90th days.
In conclusion, hypoproteinemia in patients with congestive heart failure in intensive care unit has a linear relationship with the 14th, 28th and 90th day mortality rate, and the recommended range exceeds 3.56g/dl. ARDS strongly confuses the association between albumin and the 14th and 28th day all-cause mortality. Meanwhile, With the passage of time, the all-cause mortality on the 90th day predicted better clinical results with the all-cause mortality on the 14th day. We emphasized the importance of albumin in short-term death of ICU patients with heart failure and provided theoretical threshold to provide a theoretical basis for the treatment goal. Sufficient and powerful randomized, placebo-controlled trials are needed in congestive heart failure of intensive care unit to test whether supplementing endogenous albumin may prove to be an effective method to reduce short-term all-cause mortality.
Data availability
Additional data are available in additional documents “Supplementary material.docx”.
References
DeMarco, C. et al. Clinical outcome of patients with heart failure and preserved left ventricular function. Am. J. Med. 121, 997–1001 (2008).
Safavi, K. C. et al. Variation exists in rates of admission to intensive care units for heart failure patients across hospitals in the United States. Circulation 127, 923–929 (2013).
VanDiepen, S. et al. Variation in critical care unit admission rates and outcomes for patients with acute coronary syndromes or heart failure among high- and low-volume cardiac hospitals. J. Am. Heart Assoc. 4, e001708 (2015).
Adams, K. F. J. et al. Characteristics and outcomes of patients hospitalized for heart failure in the United States: Rationale, design, and preliminary observations from the first 100,000 cases in the acute decompensated heart failure national registry (ADHERE). Am. Heart J. 149, 209–216 (2005).
Pasini, E. et al. Malnutrition, muscle wasting and cachexia in chronic heart failure: The nutritional approach. Italian Heart J.: Official J. Italian Fed. Cardiol. 4, 232–235 (2003).
Ballmer, P. E. Causes and mechanisms of hypoalbuminaemia. Clin. Nutr. 20, 271–273 (2001).
Quinlan, G. J. et al. Albumin: Biochemical properties and therapeutic potential. Hepatology 41, 1211–1219 (2005).
Uthamalingam, S. et al. Serum albumin and mortality in acutely decompensated heart failure. Am. Heart J. 160, 1149–1155 (2010).
Horwich, T. B. et al. Albumin levels predict survival in patients with systolic heart failure. Am. Heart J. 155, 883–889 (2008).
Gotsman, I. et al. Low serum albumin: A significant predictor of reduced survival in patients with chronic heart failure. Clin. Cardiol. 42, 365–372 (2019).
Nakayama, H. et al. Prognostic value of rising serum albumin during hospitalization in patients with acute heart failure. Am. J. Cardiol. 117, 1305–1309 (2016).
Fonarow, G. C. et al. Risk stratification for in-hospital mortality in acutely decompensated heart failure: Classification and regression tree analysis. JAMA 293, 572–580 (2005).
Abraham, W. T. et al. Predictors of in-hospital mortality in patients hospitalized for heart failure: Insights from the organized program to initiate lifesaving treatment in hospitalized patients with heart failure (OPTIMIZE-HF). J. Am. Coll. Cardiol. 52, 347–356 (2008).
Peterson, P. N. et al. A validated risk score for in-hospital mortality in patients with heart failure from the American heart association get with the guidelines program. Circ. Cardiovasc. Qual Outcomes 3, 25–32 (2010).
Johnson, A. E. et al. MIMIC-III, a freely accessible critical care database. Sci. Data 3, 160035 (2016).
Atherton, J. J. et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Euro. J. Heart Fail. 18, 891–975 (2016).
Ancion, A. et al. Serum albumin level and hospital mortality in acute non-ischemic heart failure. ESC Heart Fail. 4, 138–145 (2017).
Bonilla-Palomas, J. L. et al. Hypoalbuminemia in acute heart failure patients: causes and its impact on hospital and long-term mortality. J. Card. Fail. 20, 350–358 (2014).
Polat, N. et al. The prognostic significance of serum albumin in patients with acute decompensated systolic heart failure. Acta Cardiol. 69, 648–654 (2014).
Peterson, P. N. et al. A validated risk score for in-hospital mortality in patients with heart failure from the American heart association get with the guidelines program. Circ. Cardiovasc. Qual. Outcomes 3, 25–32 (2010).
Peng, W. et al. Prediction of all-cause mortality with hypoalbuminemia in patients with heart failure: A meta-analysis. Biomarkers 24, 631–637 (2019).
El Iskandarani, M. et al. Prognostic role of albumin level in heart failure: A systematic review and meta-analysis. Med. (Baltimore) 100, e24785 (2021).
Biegus, J. et al. Abnormal liver function tests in acute heart failure: Relationship with clinical characteristics and outcome in the PROTECT study. Eur. J. Heart Fail. 18, 830–839 (2016).
Peter, E. J. et al. Association of admission vs. nadir serum albumin concentration with short-term treatment outcomes in patients with acute heart failure. J. Int. Med. Res. 46, 3665–3674 (2018).
Jabbour, R. et al. Serum albumin changes and multivariate dynamic risk modelling in chronic heart failure. Int. J. Cardiol. 176, 437–443 (2014).
Grodin, J. L. et al. Clinical implications of serum albumin levels in acute heart failure: Insights from DOSE-AHF and ROSE-AHF. J. Card. Fail. 22, 884–890 (2016).
Arques, S. et al. Human serum albumin in the clinical syndrome of heart failure. J. Card. Fail. 17, 451–458 (2011).
Arques, S. et al. Hypoalbuminemia in elderly patients with acute diastolic heart failure. J. Am. Coll. Cardiol. 42, 712–716 (2003).
Roche, M. et al. The antioxidant properties of serum albumin. FEBS Lett. 582, 1783–1787 (2008).
Yamamoto, M. et al. Lower albumin levels are associated with frailty measures, trace elements, and an inflammation marker in a cross-sectional study in Tanushimaru. Environ. Health Prev. Med. 26, 25 (2021).
Brioschi, M. et al. S-Thiolation targets albumin in heart failure. Antioxidants 9, 763 (2020).
Arif, S. K. et al. Hypoproteinemia as a marker of acute respiratory distress syndrome in critically ill patients with pulmonary edema. Intensive Care Med. 28, 310–317 (2002).
Chaudhuri, S. et al. Correlation of serum albumin level to lung ultrasound score and its role as predictors of outcome in acute respiratory distress syndrome patients: A prospective observational study. Crit. Care Res. Prac. 2021, 4594790 (2021).
Gotsman, I. et al. Low serum albumin: A significant predictor of reduced survival in patients with chronic heart failure. Clinical Cardiol. 42, 365–372 (2019).
Investigators, S. S. et al. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N. Engl. J. Med. 350, 2247–2256 (2004).
Caironi, P. et al. Albumin replacement in patients with severe sepsis or septic shock. N. Engl. J. Med. 370, 1412–1421 (2014).
Acknowledgements
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chao, P., Cui, X., Wang, S. et al. Serum albumin and the short-term mortality in individuals with congestive heart failure in intensive care unit: an analysis of MIMIC. Sci Rep 12, 16251 (2022). https://doi.org/10.1038/s41598-022-20600-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-20600-1
This article is cited by
-
Blood urea nitrogen to serum albumin ratio as a new prognostic indicator in type 2 diabetes mellitus patients with chronic kidney disease
Scientific Reports (2024)
-
Prognostic role of serum albumin levels in patients with chronic heart failure
Internal and Emergency Medicine (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.