Abstract
Cancer cachexia affects quality of life, response to chemotherapy, and survival in many advanced cancer patients. The aim of this study was to evaluate the prognostic value of pretreatment cachexia index (CXI) in patients with advanced hepatocellular carcinoma (HCC) treated with systematic chemotherapy. Patients with advanced HCC treated with lenvatinib therapy between October 2018 and October 2020 were retrospectively studied. The CXI was calculated as (L3 skeletal muscle index) × (serum albumin)/(neutrophil-to-lymphocyte ratio). The association with treatment response and early adverse events within the first two months of lenvatinib therapy was investigated. Overall survival (OS) and progression-free survival (PFS) were estimated using the Kaplan–Meier method with log-rank test. Multivariable Cox regression was used to identify the predictors of survival. A total of 116 patients (median age: 60, male: 84.5% ) with calculated CXI. They divided into two groups: high CXI (≥ 53, n = 82) and low CXI (< 53, n = 34). Patients with low CXI had a significantly lower disease control rate (61.8% vs. 89.0%, p = 0.001) and a shorter median OS (8.0 [95% CI 6.2–9.8] vs. 12.3 [95% CI 10.1–14.4] months, p = 0.002) than those with high CXI. In multivariable analysis, low CXI was independently associated with shorter OS (HR: 2.07, 95% CI: 1.17–3.65, p = 0.01) and PFS (HR: 1.84, 95% CI: 1.09–3.09, p = 0.02). Of note, during the first two months of lenvatinib therapy, anorexia (41.2% vs. 22.0%, p = 0.04) developed more frequently among patients with low CXI than those with high CXI. The CXI may be a clinically useful index for predicting poor treatment response and prognosis in patients with advanced HCC undergoing lenvatinib treatment.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) is one of the most common malignancies and third leading cause of cancer-related death worldwide1,2. In spite of dismal prognosis of advanced HCC2, recently, there has been a remarkable progress in the development of novel drugs for systemic treatment including molecular targeting agents (MTAs) such as lenvatinib3 and immune checkpoint inhibitors4. However, the response rate to systemic therapy is varied according to both tumor and patient baseline characteristics5,6.
Malnutrition 7, low skeletal muscle mass8 and inflammation9 have been suggested as poor prognostic factors in HCC patients along with tumor burden10 and hepatic reserve function11. “Cancer cachexia” describes such pathological condition in cancer patients, which is a multifactorial syndrome characterized by an ongoing loss of skeletal muscle mass attributable to negative protein and energy balance driven by a combination of reduced nutritional intake and tumor- and host-derived abnormal metabolic alterations12. Cancer cachexia not only results in decreased quality of life but is also associated with poor responses to chemotherapy and survival13,14.
According to the international consensus group, patients are considered as having cachexia when they have more than 5% loss of stable body weight in the preceding 6 months, or a body mass index (BMI) less than 20 kg/m2 and ongoing weight loss of more than 2%, or sarcopenia and ongoing weight loss of more than 2%15. However, weight loss may be confounded by reduced adipose tissue or loss of body fluid which develops commonly in patients with advanced cancer16. Furthermore, it is difficult to assess the severity of cachexia since there are no robust biomarkers to identify at-risk patients17.
The cachexia index (CXI) is a novel measure of cachexia by incorporating the clinical measures of several key features of cachexia, including reduced muscle mass, poor nutritional status, and systemic inflammation. It has demonstrated correlation with the prognosis in advanced lung cancer and non-Hodgkin’s lymphoma18,19,20. In this study, we aimed to evaluate the prognostic value of CXI in patients with advanced HCC treated with lenvatinib.
Materials and methods
Patients
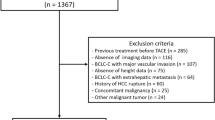
In this retrospective study, 217 patients with advanced HCC who were treated with lenvatinib as a first-line systemic therapy at Samsung Medical Center between October 2018 and October 2020 were screened as potential eligible patients. The diagnosis of HCC was made histologically or clinically in accordance with the regional HCC guidelines21,22. Patients were excluded if they met any of the following criteria (n = 101): (i) concurrent therapy with other systemic agents or radioembolization; (ii) unusual dosing regimens or frequent dose modifications due to poor drug adherence; (iii) discontinuation of lenvatinib before the 1st treatment response assessment (i.e., refusal of further treatment, follow-up loss, deterioration of performance status or liver function, infection, severe adverse events (AEs)); (iv) baseline liver function of Child–Pugh score ≥ 7; or (v) absence of valid baseline computed tomography (CT) image. Accordingly, a total of 116 consecutive patients with advanced HCC treated with lenvatinib were included in the final analysis (Fig. 1).
This study was approved by the Institutional Review Board at Samsung Medical Center, Seoul, Korea (IRB No. 2021-02-149) and was performed in accordance with the ethical guidelines of the Declaration of Helsinki. The requirement for written informed consent was waived by the IRB because the data used for analysis was anonymous and deidentified.
Data collection
Clinical characteristics including demographic information, Eastern Cooperative Oncology Group performance status (ECOG PS), comorbid condition (hypertension and diabetes mellitus), anthropometric measurements, laboratory findings (absolute neutrophil count, absolute lymphocyte count, albumin, liver function test, alpha-fetoprotein (AFP) and protein induced by vitamin K absence or antagonist-II (PIVKA-II)), and image findings (the number and size of intrahepatic lesions, macrovascular invasion and extrahepatic lesions) at the introduction time of lenvatinib or from the closest date were collected by retrospective review of medical records. In addition, information for stage of HCC according to Barcelona Clinic Liver Cancer (BCLC) stage23, previous treatment for HCC, and hepatic reserve function including Child Pugh classification or modified ALBI (mALBI) grade at baseline was obtained. ALBI score was calculated based on serum albumin and total bilirubin values using the following formula: ALBI score = (log10 bilirubin (µmol/L) × 0.66) + (albumin (g/L) x − 0.085). mALBI grade was defined by the following 4 grades: ≤ − 2.6 (grade 1), > − 2.60 to ≤ − 2.27 (grade 2a), > − 2.27 to ≤ − 1.39 (grade 2b), > − 1.39 (grade 3)24. Lastly, date of disease progression, date of death, or date of last follow-up was collected. The last date of follow-up data collection was March 21, 2021.
Assessment of treatment response and AEs
All patients received recommended starting dose for lenvatinib based on body weight: 12 mg/day in patients with body weight ≥ 60 kg or 8 mg/day in patients with body weight < 60 kg. During the study period, dose reduction or treatment interruption was made in patients who developed grade ≥ 3 AEs or uncontrolled AEs despite symptomatic management. Lenvatinib was discontinued when any unacceptable or serious AEs or clinical tumor progression was observed. Treatment response was evaluated by contrast-enhanced dynamic CT or magnetic resonance imaging (MRI) every 1–3 months according to the modified Response Evaluation Criteria in Solid Tumors (mRECIST)25. The objective response rate (ORR) was defined as the proportion of patients who achieved complete response (CR) or partial response (PR). The disease control rate (DCR) was defined as the proportion of patients who achieved CR, PR, and stable disease26. All the measurements were performed by two independent readers (MJG and WK).
For assessment of AEs, patients were evaluated at week 2 of lenvatinib therapy using laboratory results and physical findings. Thereafter, safety assessment was performed along with treatment response assessment every 1–3 months. We collected the information about development of AEs within the first 2 months of lenvatinib therapy by medical record review and graded according to the Common Terminology Criteria for Adverse Events version 5.0.
Measurement of skeletal muscle index (SMI)
Using an open-source semi-automated software (BMI measurement tools, version 1.0; https://sourceforge.net/projects/muscle-fat-area-measurement/27, cross-sectional areas of the rectus, transverse and oblique abdominal muscles, psoas muscles, and paraspinal muscles were measured at mid-L3 vertebra level by setting a threshold of − 29 to 150 Hounsfield units on the available CT scan performed before treatment initiation. Most (87.5%) of patients had performed CT scan within 1 month and the rest had within 3 months prior to initiating lenvatinib therapy as a baseline study. L3 skeletal muscle area was normalized for height in m2 and expressed as SMI.
Definition of cachexia index
The CXI was calculated as follows:
where SMI is the skeletal muscle index, Alb is the serum albumin in g/dL and NLR is the neutrophil-to-lymphocyte ratio, which was calculated by absolute neutrophil count / absolute lymphocyte count18.
Statistical analysis
Baseline characteristics were compared using the Mann–Whitney U tests for continuous variables or Fisher’s exact tests for categorical variables. The CXI was dichotomized at the value of 53 to evaluate the effect of CXI on treatment response, occurrence of AEs during first 2 months and survival. The cutoff point of CXI was determined by area under the receiver operating characteristics (AUROC) analysis. For other continuous variables (age, BMI, AFP, and PIVKA-II), cutoffs were chosen according to published cutoff points (BMI, AFP, and PIVKA-II)15,28, or median splits (age). Overall survival (OS) and progression-free survival (PFS) were evaluated by Kaplan–Meier method using the log-rank test to find difference between the two curves. The factors associated with OS and PFS were analyzed using the Cox proportional hazard model, and P-values of < 0.20 in the univariate analysis was used for multivariable analysis. A P-value of less than 0.05 was considered statistically significant. All statistical analyses were performed with SPSS 27.0 statistical software (IBM Corp., NY, USA).
Ethics declarations
This study was approved by the Institutional Review Board at Samsung Medical Center, Seoul, Korea (IRB No. 2021-02-149) and was performed in accordance with the ethical guidelines of the Declaration of Helsinki. The requirement for written informed consent was waived by the IRB because the data used for analysis was anonymous and deidentified.
Results
Patient characteristics
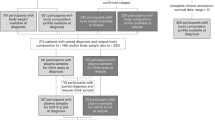
The baseline characteristics of total 116 patients are listed in Table 1. The median age for the entire group was 60 years, and 84.5% was male (n = 98). Median BMI was 23.4 kg/m2. All patients were ECOG PS score of 0 (n = 101) or 1 (n = 15). Most patients (90.5%) were diagnosed with BCLC stage C, and 88 (75.7%) patients had extrahepatic metastases. Twenty patients (17.2%) had Child–Pugh scores of 6, and 15 patients had mALBI grade ≥ 2b. The CXI values widely ranged from 17.6 to 304.2. Patients were divided into two groups: high CXI (≥ 53) and low CXI (< 53). The baseline characteristics between high and low CXI were not significantly different except that the low CXI group had a higher proportion of intrahepatic lesions and a higher PIVKA-II level compared to those in the high CXI group.
Treatment response
Among 116 patients, CR was achieved in 1 (0.9%) patient, partial response PR in 24 (20.7%) patients, and SD in 69 (59.5%) patients, resulting in ORR and DCR values of 22.4% (95% confidence interval [CI], 15.2–31.1) and 81.0% (95% CI, 72.7–87.7), respectively (Table 2). There was no significant difference in ORR between the two groups. However, low CXI group had a significantly lower DCR when compared to those in high CXI group (61.8% vs. 89.0%, p = 0.001) (Table 2).
Association between CXI and AEs development within the first 2 months of lenvatinib
During the first 2 months of lenvatinib therapy, 90 (77.6%) of 116 patients developed any grade of AEs (Table 3), and 14 (12.1%) developed grade ≥ 3 AEs. Anorexia, gastrointestinal discomfort such as nausea, vomiting, dyspepsia or epigastric soreness, abdominal pain, hypertension, and hand-foot-skin reactions (HFSR) were identified as the early AEs with the highest frequencies of any grades. Proteinuria was the most common AEs of grade ≥ 3 (5/14, 35.7%). Most AEs improved by symptomatic treatment and 20.7% of patients reduced dose of lenvatinib therapy before first tumor response assessment. There was no significant difference between the high and low CXI groups regarding development of AEs of all grade or grade ≥ 3 during first 2 months after chemotherapy. When comparing difference in frequency among individual AEs, anorexia was notably more frequent in the low CXI group (41.2% vs. 22.0%, p = 0.04). Gastrointestinal discomfort or abdominal pain occurred more frequent in the low CXI group compared to the high CXI group (35.3% vs. 20.7%, p = 0.11, 32.4% vs. 17.1%, p = 0.08, respectively) while hypertension and HFSR occurred more frequently in the high CXI group compared to the low CXI group (25.6% vs. 8.8%, p = 0.05 and 24.4% vs. 8.8%, p = 0.07, respectively); but neither showed statistical significance (Table 3).
Factors associated with OS
Kaplan–Meier estimates of median OS in all patients was 10.8 (95% CI 8.9–12.8) months. The OS of the high CXI group was significantly higher than that of the low CXI group: 12.3 months (95% CI 10.1–14.4) versus 8.0 months (95% CI 6.2–9.8), Plog rank = 0.002 (Fig. 2a). In multivariable analysis, BMI < 20 kg/m2 (HR: 2.18, 95% CI: 1.13–4.18, p = 0.02) and low CXI (HR: 2.07, 95% CI: 1.17–3.65, p = 0.01) were significant independent factors associated with OS (Table 4).
Factors associated with PFS
During a median follow-up period of 5.3 months (range 3.4–8.2), disease progression or death occurred in 74 patients. Patients with high CXI demonstrated a longer PFS than those with low CXI (6.9 months, 95% CI 4.3–9.4 vs. 4.0 months, 95% CI 1.9–6.1, plog rank = 0.009) (Fig. 2b). In multivariable analysis, AFP ≥ 400 ng/mL (HR: 1.80, 95% CI: 1.10–2.95, p = 0.02), and low CXI (HR: 1.84, 95% CI: 1.09–3.09, p = 0.02) were significantly associated with PFS (Table 5).
Discussion
In this study, we demonstrated that the CXI was an independent prognostic factor for survival in advanced HCC patients treated with lenvatinib therapy. Notably, patients with low CXI showed poor treatment response in terms of DCR and PFS as well as higher rate of anorexia during the first 2 months after chemotherapy. Although the median values of CXI are different from the previous study ascribed to different characteristics of enrolled patients including demographic information, tumor type, and treatment status, similar results were obtained in this study.
The current consensus definition of cancer cachexia focused on weight loss or sarcopenia. A Japanese study of 100 patients with unresectable HCC reported that low skeletal muscle mass was an independent prognostic factor for survival29. However, in the current study, low skeletal muscle index alone was not associated with OS or PFS (Supplementary Fig. S1). This discrepancy may be attributable to the difference in the demographic profile of the study population between the two studies. The study population was younger in this study compared to the previous Japanese study (median age, 59.5 vs. 71.5) resulting in lower frequency of sarcopenic patients in this study (n = 20, 15.6%) when the cutoff values of the previous study were applied (< 42 cm2/m2 for men and < 38 cm2/m2 for women). In contrast, pretreatment CXI showed a significant association with OS after adjustment for tumor extent, hepatic reserve function, and underweight. This result suggests that CXI may be useful to identify patients at pre-cachexia condition, which is the initial phase with metabolic changes including systemic inflammation and minor body weight loss but not yet a significant depletion of skeletal muscle mass.
Cancer cachexia is a consequential process of chronic inflammation mediated by the tumor microenvironment and the inflammatory response of the host12,30. Cytokines such as tumor necrosis factor (TNF)-α, interleukins, and transforming growth factor(TGF)-β, which are produced by tumor cells and surrounding cells including cancer-associated fibroblasts stimulate a epithelial-mesenchymal transition to promote cancer progression, invasion, and metastasis31. Rodent tumor models shown evidence that increased production of systemic inflammatory cytokines such as TNF-α, IL-1, and IL-6 was associated development of cancer cachexia and weight loss32,33. A recent Korean study of 238 HCC patients reported that the serum level of several myokines including follistatin and IL-6 was higher in HCC patients with sarcopenia than in heathy controls, and that it was related to poor survival34. Hence, cancer cachexia was more frequently observed in advanced HCC 34. In this study, patients with low CXI seemed to have larger tumors, more tumor numbers, portal vein invasion, and higher serum AFP and PIVKA-II levels than in those with high CXI, which could describe their poor prognosis.
Moreover, elevated IL-6 and decreased IL-15 in pre-cachetic and cachetic patients can alter the function of immune cells, which resulted reduced anti-tumor effect35. Notably, patients with baseline sarcopenia compared to those without, had significant higher percentage of progressive HCC despite intervention in the 1st (29.2 vs. 16.1; p = 0.023), 3rd (40.7 vs. 29.5; p = 0.001), 6th (51.4 vs. 30.6; p = 0.001) and the 12th months (32.1 vs. 25.7; p = 0.001)36. One previous study reported that sorafenib responses are diminished in individuals with sarcopenic obesity with increased visceral fat, which suggests body composition could be predictive marker for primary resistance to tyrosine kinase inhibitors in patients with advanced HCC37. Hence, it is reasonable to assume that the treatment response to lenvatinib is reduced in cachexic patients resulting in poor clinical outcome. This hypothesis is supported by the findings of this study where the patients with low CXI had a significantly lower DCR (68.0% vs. 87.2%, p = 0.01) and a shorter median OS (9.5 (95% CI: 7.0–12.0) months versus 13.2 (95% CI: 10.9–15.5) months, p = 0.001). Low CXI was an independent risk factor for OS, PFS, and disease control rate at 4–12 week and progression-free survival after adjusting tumor- and hepatic function related factors (Tables 4 and 5, Supplementary Table S1). Nevertheless, underlying mechanism supporting the interaction between cachexia and TKI sensitivity in advanced HCC needs further investigation.
Regarding early AEs developed during the first 2 months after chemotherapy, patients with low CXI showed higher proportion of anorexia, which is correlated with clinical presentation of cancer cachexia. In fact, not only anorexia is considered to be an important component of cachexia but also sarcopenia potentiates chemotherapy associated anorexia38,39; hence, it is not surprising that anorexia developed more frequently in patients with low CXI consistent to previous studies29,40. Previously, several studies have reported that low SMI was associated with severe AEs29,41. However, neither SMI nor CXI was associated with severe AEs in this study. Different patterns of AE development were observed as well, where grade ≥ 3 proteinuria was observed with the highest frequency among the severe AEs compared with anorexia or diarrhea in the previous studies29,41. Interestingly, anti-angiogenesis-related adverse events including proteinuria, hypertension or HFSR, which were known to show better clinical outcomes42, developed more frequently in patients with high CXI though statistical significance was not achieved due to insufficient sample size.
There are several limitations in this study. First, because of its retrospective nature, many patients were excluded due to insufficient information such as no baseline CT, and therefore the number of subjects included in the final analysis was narrowed and the duration of observation was relatively short. Second, some of the AEs such as proteinuria or hypothyroidism may have been missed in the medical records, which may have affected the association between CXI and AEs. Furthermore, because the components of the CXI formula include albumin and neutrophil-to-lymphocyte ratio, the hepatic reserve function and the extent of tumor may affect the CXI. To overcome this potential caveat, we tried to include relatively homogenous population in terms of tumor extent [BCLC stage C (90.5%) with the presence of extrahepatic metastasis (75.7%)] and hepatic reserve function [Child–Pugh A (100%)]. Finally, although each component of CXI is well-established in terms of pathogenesis of cachexia, the weighting of each factor and optimum cut-off values need further investigation with a larger cohort. Additionally, the impact of the dynamic changes of CXI with intervention to improve nutritional state or muscle volume should be warranted.
Conclusion
The CXI was an independent prognostic factor for OS and disease progression in advanced HCC patients treated with lenvatinib therapy. The low CXI indicates a shorter OS and lower DCR. Therefore, the CXI may serve as a clinically useful index for predicting the prognosis in advanced HCC patients on chemotherapy. Moreover, nutritional support would be helpful to mitigate the early development of anorexia in patients with low pretreatment CXI.
Data availability
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- MTAs:
-
Molecular targeting agents
- BMI:
-
Body mass index
- CXI:
-
Cachexia index
- AEs:
-
Adverse events
- CT:
-
Computed tomography
- ECOG PS:
-
Eastern Cooperative Oncology Group performance status
- AFP:
-
Alpha-fetoprotein
- PIVKA-II:
-
Protein induced by vitamin K absence or antagonist-II
- BCLC:
-
Barcelona clinic liver cancer
- mALBI:
-
Modified ALBI
- MRI:
-
Magnetic resonance imaging
- mRECIST:
-
Modified Response Evaluation Criteria in Solid Tumors
- ORR:
-
Objective response rate
- CR:
-
Complete response
- PR:
-
Partial response
- DCR:
-
Disease control rate
- SD:
-
Stable disease
- SMI:
-
Skeletal Muscle Index
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- HFSR:
-
Hand-foot-skin reactions
- TNF:
-
Tumor necrosis factor
- TGF:
-
Transforming growth factor
- IL:
-
Interleukin
- VEGF:
-
Vascular endothelial growth factor
References
Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer J. Clin. 68, 394–424. https://doi.org/10.3322/caac.21492 (2018).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2016. CA A Cancer J. Clin. 66, 7–30. https://doi.org/10.3322/caac.21332 (2016).
Kudo, M. et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: A randomised phase 3 non-inferiority trial. Lancet (Lond., Engl.) 391, 1163–1173. https://doi.org/10.1016/s0140-6736(18)30207-1 (2018).
Rimassa, L., Pressiani, T. & Merle, P. Systemic treatment options in hepatocellular carcinoma. Liver Cancer 8, 427–446. https://doi.org/10.1159/000499765 (2019).
Berhane, S., Fox, R., García-Fiñana, M., Cucchetti, A. & Johnson, P. Using prognostic and predictive clinical features to make personalised survival prediction in advanced hepatocellular carcinoma patients undergoing sorafenib treatment. Br J Cancer 121, 117–124. https://doi.org/10.1038/s41416-019-0488-4 (2019).
Pfister, D. et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature 592, 450–456. https://doi.org/10.1038/s41586-021-03362-0 (2021).
Schütte, K. et al. Malnutrition is a prognostic factor in patients with hepatocellular carcinoma (HCC). Clin. Nutr. (Edinb., Scot.) 34, 1122–1127. https://doi.org/10.1016/j.clnu.2014.11.007 (2015).
Uchikawa, S. et al. Skeletal muscle loss during tyrosine kinase inhibitor treatment for advanced hepatocellular carcinoma patients. Liver Cancer 9, 148–155. https://doi.org/10.1159/000503829 (2020).
Nakano, M. et al. Immunological inflammatory biomarkers as prognostic predictors for advanced hepatocellular carcinoma. ESMO Open 6, 100020. https://doi.org/10.1016/j.esmoop.2020.100020 (2021).
Goh, M. J. et al. Efficacy and safety of lenvatinib therapy for unresectable hepatocellular carcinoma in a real-world practice in Korea. Liver Cancer 10, 52–62. https://doi.org/10.1159/000512239 (2021).
Hiraoka, A. et al. Prognostic factor of lenvatinib for unresectable hepatocellular carcinoma in real-world conditions-multicenter analysis. Cancer Med. 8, 3719–3728. https://doi.org/10.1002/cam4.2241 (2019).
Fearon, K. C., Glass, D. J. & Guttridge, D. C. Cancer cachexia: Mediators, signaling, and metabolic pathways. Cell Metab. 16, 153–166. https://doi.org/10.1016/j.cmet.2012.06.011 (2012).
Vaughan, V. C., Martin, P. & Lewandowski, P. A. Cancer cachexia: Impact, mechanisms and emerging treatments. J. Cachexia. Sarcopenia Muscle 4, 95–109. https://doi.org/10.1007/s13539-012-0087-1 (2013).
Jindal, A. & Jagdish, R. K. Sarcopenia: Ammonia metabolism and hepatic encephalopathy. Clin. Mol. Hepatol. 25, 270–279. https://doi.org/10.3350/cmh.2019.0015 (2019).
Fearon, K. et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 12, 489–495. https://doi.org/10.1016/s1470-2045(10)70218-7 (2011).
Amano, K. et al. Significance of fluid retention, body mass index, and weight loss in patients. JCSM Clin Rep 5, 69–78. https://doi.org/10.1002/crt2.23 (2020).
Argilés, J. M. et al. The cachexia score (CASCO): A new tool for staging cachectic cancer patients. J. Cachexia. Sarcopenia Muscle 2, 87–93. https://doi.org/10.1007/s13539-011-0027-5 (2011).
Jafri, S. H., Previgliano, C., Khandelwal, K. & Shi, R. Cachexia Index in advanced non-small-cell lung cancer patients. Clin. Med. Insights Oncol. 9, 87–93. https://doi.org/10.4137/CMO.S30891 (2015).
Go, S. I., Park, M. J. & Lee, G. W. Clinical significance of the cachexia index in patients with small cell lung cancer. BMC Cancer 21, 563. https://doi.org/10.1186/s12885-021-08300-x (2021).
Karmali, R. et al. Impact of cachexia on outcomes in aggressive lymphomas. Ann Hematol 96, 951–956. https://doi.org/10.1007/s00277-017-2958-1 (2017).
Korean Liver Cancer Association & National Cancer Center. Korean Liver Cancer Association-National Cancer Center Korea practice guidelines for the management of hepatocellular carcinoma. Gut Liver 13, 227–299. https://doi.org/10.5009/gnl19024(2019) (2018).
Korean Association for the Study of the Liver. KASL clinical practice guidelines for management of chronic hepatitis B. Clin. Mol. Hepatol. 28, 276–331. https://doi.org/10.3350/cmh.2022.0084 (2022).
Bruix, J. & Sherman, M. Management of hepatocellular carcinoma: An update. Hepatology 53, 1020–1022. https://doi.org/10.1002/hep.24199 (2011).
Hiraoka, A. et al. Validation and potential of albumin-bilirubin grade and prognostication in a Nationwide Survey of 46,681 hepatocellular carcinoma patients in Japan: The need for a more detailed evaluation of hepatic function. Liver Cancer 6, 325–336. https://doi.org/10.1159/000479984 (2017).
Lencioni, R. & Llovet, J. M. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin. Liver Dis. 30, 52–60. https://doi.org/10.1055/s-0030-1247132 (2010).
Demetris, A. J. et al. 2016 Comprehensive update of the banff working group on liver allograft pathology: Introduction of antibody-mediated rejection. Am. J. Transp. 16, 2816–2835. https://doi.org/10.1111/ajt.13909 (2016).
Kim, S. S. et al. Semiautomatic software for measurement of abdominal muscle and adipose areas using computed tomography: A STROBE-compliant article. Med. (Baltimore) 98, e15867. https://doi.org/10.1097/MD.0000000000015867 (2019).
Takada, Y. & Uemoto, S. Liver transplantation for hepatocellular carcinoma: the Kyoto experience. J. Hepatobiliary Pancreat. Sci. 17, 527–532. https://doi.org/10.1007/s00534-009-0162-y (2010).
Uojima, H. et al. Skeletal muscle mass influences tolerability and prognosis in hepatocellular carcinoma patients treated with lenvatinib. Liver Cancer 9, 193–206. https://doi.org/10.1159/000504604 (2020).
Porporato, P. E. Understanding cachexia as a cancer metabolism syndrome. Oncogenesis 5, e200. https://doi.org/10.1038/oncsis.2016.3 (2016).
Inácio Pinto, N. et al. Cancer as a proinflammatory environment: Metastasis and cachexia. Mediators Inflamm. 2015, 791060. https://doi.org/10.1155/2015/791060 (2015).
Gelin, J. et al. Role of endogenous tumor necrosis factor alpha and interleukin 1 for experimental tumor growth and the development of cancer cachexia. Cancer Res. 51, 415–421 (1991).
Strassmann, G., Fong, M., Kenney, J. S. & Jacob, C. O. Evidence for the involvement of interleukin 6 in experimental cancer cachexia. J. Clin. Invest. 89, 1681–1684. https://doi.org/10.1172/JCI115767 (1992).
Choi, K. et al. The association of the serum levels of myostatin, follistatin, and interleukin-6 with sarcopenia, and their impacts on survival in patients with hepatocellular carcinoma. Clin. Mol. Hepatol. 26, 492–505. https://doi.org/10.3350/cmh.2020.0005 (2020).
Khaddour, K., Gomez-Perez, S. L., Jain, N., Patel, J. D. & Boumber, Y. Obesity, sarcopenia, and outcomes in non-small cell lung cancer patients treated with immune checkpoint inhibitors and tyrosine kinase inhibitors. Front. Oncol. 10, 576314. https://doi.org/10.3389/fonc.2020.576314 (2020).
Badran, H. et al. Baseline Sarcopenia is Associated with lack of response to therapy, liver decompensation and high mortality in hepatocellular carcinoma patients. Asian Pac. J. Cancer Prev. 21, 3285–3290. https://doi.org/10.31557/apjcp.2020.21.11.3285 (2020).
Nault, J. C. et al. Visceral fat area predicts survival in patients with advanced hepatocellular carcinoma treated with tyrosine kinase inhibitors. Digestive Liver Dis. 47, 869–876. https://doi.org/10.1016/j.dld.2015.07.001 (2015).
da Silva, S. P., Santos, J. M. O., Costa, E. S. M. P., da Costa, R. M. G. & Medeiros, R. Cancer cachexia and its pathophysiology: Links with sarcopenia, anorexia and asthenia. J Cachexia Sarcopenia Muscle 11, 619–635. https://doi.org/10.1002/jcsm.12528 (2020).
Vega, M. C., Laviano, A. & Pimentel, G. D. Sarcopenia and chemotherapy-mediated toxicity. Einstein (Sao Paulo) 14, 580–584. https://doi.org/10.1590/S1679-45082016MD3740 (2016).
Hiraoka, A. et al. Clinical importance of muscle volume in lenvatinib treatment for hepatocellular carcinoma: Analysis adjusted with inverse probability weighting. J. Gastroenterol. Hepatol. 36, 1812–1819. https://doi.org/10.1111/jgh.15336 (2021).
Bozzetti, F. Forcing the vicious circle: Sarcopenia increases toxicity, decreases response to chemotherapy and worsens with chemotherapy. Ann. Oncol. 28, 2107–2118. https://doi.org/10.1093/annonc/mdx271 (2017).
Liu, X. et al. Early presence of anti-angiogenesis-related adverse events as a potential biomarker of antitumor efficacy in metastatic gastric cancer patients treated with apatinib: A cohort study. J. Hematol. Oncol. 10, 153. https://doi.org/10.1186/s13045-017-0521-0 (2017).
Funding
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (NRF-2016R1C1B2015463 and NRF-2019R1C1C1007729). This research was also supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HR20C0025).
Author information
Authors and Affiliations
Contributions
M.J.G. and W.K.: study design and drafting of the manuscript. W.K.J.: software, statistical analysis, and interpreted the data. D.H.S.: study design, interpretated data, and manuscript review & editing. G.Y.G.: resources, data curation and critical revision of the manuscript. Y.H.P.: statistical analysis, visualization, and manuscript review & editing. M.S.C.: study design, methodology, formal analysis, and study supervision. J.H.L.: study supervision, visualization, and interpreted data. K.C.K.: project administration, study supervision and interpreted data. S.W.P.: project administration, study supervision, and critical revision of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goh, M.J., Kang, W., Jeong, W.K. et al. Prognostic significance of cachexia index in patients with advanced hepatocellular carcinoma treated with systemic chemotherapy. Sci Rep 12, 7647 (2022). https://doi.org/10.1038/s41598-022-11736-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-11736-1
This article is cited by
-
Cachexia Index in Patients with Gastrointestinal Cancer: A Systematic Review and Meta-Analysis
Journal of Gastrointestinal Cancer (2024)
-
Evaluation of the cachexia index using a bioelectrical impedance analysis in elderly patients with non-Hodgkin’s lymphoma: A single-center prospective study
Annals of Hematology (2024)
-
Prognostic significance of the cachexia index in patients with unresectable advanced gastric cancer receiving palliative chemotherapy: a retrospective single-center study
Surgery Today (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.