Abstract
The prevalence of atopic diseases has been steadily increasing since the mid twentieth century, a rise that has been linked to modern hygienic lifestyles that limit exposure to microbes and immune system maturation. Overactive type 2 CD4+ helper T (Th2) cells are known to be closely associated with atopy and represent a key target for treatment. In this study, we present an initial characterization of ammonia oxidizing bacteria (AOB) Nitrosomonas eutropha D23, an environmental microbe that is not associated with human pathology, and show AOB effectively suppress the polarization of Th2 cells and production of Th2-associated cytokines (IL-5, IL-13, and IL-4) by human peripheral blood mononuclear cells (PBMC). We show that AOB inhibit Th2 cell polarization not through Th1-mediated suppression, but rather through mechanisms involving the anti-inflammatory cytokine IL-10 and the potential inhibition of dendritic cells, as evidenced by a reduction in Major Histocompatibility Complex Class II (MHC II) and CD86 expression following AOB treatment. This is the first report of immunomodulatory properties of AOB, and provides initial support for the development of AOB as a potential therapeutic for atopic diseases.
Similar content being viewed by others
Introduction
Since the mid twentieth century, the prevalence of atopic diseases has been steadily increasing with more than 200 million people worldwide suffering from diseases such as asthma, allergic rhinitis, or food allergies1. The rapid increase in atopy prevalence cannot be explained by changes in population genomics. Rather, the association with westernized societies suggests that environmental factors such as diet, antibiotic exposure, and other modern hygienic lifestyles play a crucial role in the etiology of these conditions2,3,4,5.
Notably, reduced exposure to non-commensal microbes, particularly early in life, as well as a loss of biodiversity within the human microbiome has been associated with atopy5,6,7,8. Exposure to microbes is essential for immune system development and training. Microbes can reinforce barrier immunity and condition innate cells to promote effector B and T cell responses against pathogens, and more specifically balance the relative numbers and specificity of different CD4+ T helper cell populations (Th1, Th2 and Th17) and regulatory T cells (Tregs)9,10,11. When underexposed to foreign antigens, the immune system is not trained to react appropriately to non-noxious antigenic stimuli, which leads to disproportionate responses to self-tissues (auto-immune diseases) or external triggers that are otherwise innocuous stimuli (atopic diseases)12,13.
Atopic diseases are marked by an exaggerated, systemic type 2 inflammatory reaction to otherwise innocuous stimuli that induce high levels of immunoglobulin E (IgE) production by B cells, eosinophilia, and various associated inflammatory immune responses14. Therapeutic approaches that interfere with Th2 cells and their cytokine mediators such as IL-5, IL-13, and IL-4 have shown promise, highlighting the potential of targeting this pathway14.
Given the role of microbes in immune system maturation, several studies have focused on identifying bacteria that have the ability to modulate the Th2 pathway and improve allergy symptoms in preclinical models6. Probiotic or commensal bacteria such as Lactobacillus, Weissela cibaria WIKIM28 or Bacteroides fragilis were found to interfere with the Th2 pathway by inducing Th1 cells or Tregs15,16,17,18. Exposure to agrarian conditions is also suggested to be protective, leading investigators to search for microbes in cowsheds and other farming environments. Cowshed bacteria, such as Acinetobacter lwoffii F78, Lactococcus lactis G121, and Staphylococcus sciuri W620, were shown to shift T cell polarization towards a Th1 response via dendritic cell conditioning6,19,20,21. These cowshed bacteria highlight the potential to identify novel immuno-modulatory bacteria from farm environments.
Farm soils frequently contain high concentrations of ammonium due to animal waste and fertilizers, and are consequently niches containing ammonia oxidizing bacteria (AOB)22,23. These soil chemolithoautotrophic Gram negative bacteria play a critical role in the global nitrogen cycle22. They can extract energy by oxidizing ammonia, a process generating the immunomodulatory molecule nitric oxide as a byproduct24,25. Interestingly, AOB have been detected in human microbiomes, and have been hypothesized to be depleted in recent decades due to modern hygienic lifestyles26,27,28. Therefore, we postulated that AOB could play a role in the human microbiome’s ability to regulate the immune response.
In this study, we present the first report that the AOB Nitrosomonas eutropha D23 inhibit Th2 immune polarization in human primary immune cells. Unlike many other Th2 suppressing bacteria, AOB do not to require the classical Th1 pathway to achieve this Th2 suppression, but rather the anti-inflammatory cytokine IL-10. We posit that this may be via the dampening of dendritic cells’ ability to activate Th2 cells.
Results
AOB inhibit Th2 immune polarization in human PBMC
To test the effect of AOB on immune responses, we developed a co-culture model with human peripheral blood mononuclear cells (PBMC) derived from healthy subjects. While AOB would not directly encounter blood and its constituents frequently, PBMC provide a well-studied model to test host-microbe interactions, and allow for investigations that are inclusive of many immune cell-types and potential signaling pathways.
First, we validated this host-microbe model by investigating AOB toxicity to PBMC and vice versa. AOB were added to PBMC at a ratio of four bacteria per PBMC for 72 h. AOB did not significantly affect PBMC cell viability as measured by the metabolic activity dye WST-1 or LIVE/DEAD staining (Figure S1a,b, p > 0.05). Furthermore, PBMC did not adversely affect AOB viability; nitrite production, a measure of AOB activity, remained unchanged in presence or absence of PBMC (Figure S1f, p > 0.05). Moreover, the ability of AOB, but not PBMC, to produce nitrite in RPMI media suggests the bacterial cells are active, metabolizing ammonia present in the media that is potentially produced by PBMC metabolism (Figure S1f). Thus, AOB and PBMC can effectively be co-cultured and their respective activities assessed.
We then tested if AOB modulate Th2 immune response pathways associated with atopic diseases29. We used PBMC from a healthy, non-atopic human donor, and treated them with exogenous factors to induce a Th2-polarized phenotype. First, we stimulated PBMC for 3 days using a proprietary Th2 differentiation kit (R&D Systems) and measured cytokine production in the culture supernatant by ELISA. Th2 stimulation led to the production of 826 ± 253 pg/mL IL-5 and 495 ± 177 pg/mL IL-13, two key markers of Th2 polarization. In contrast, unstimulated cells did not produce any detectable levels of these cytokines (Fig. 1a,b).
AOB inhibit Th2 immune polarization in human PBMC. (a–f) IL-5 and IL-13 supernatant levels are reduced with AOB pretreatment of PBMC prior to Th2 differentiation cocktail stimulation; measured by ELISA of supernatants 72 h post-stimulation. IL-4 gene expression is also reduced with AOB pretreatment; measured by qPCR 72 h post-stimulation. AOB pre-treatment prior to Th2 differentiation cocktail stimulation of PBMCs from donor A reduced the levels of IL-5 (a) and IL-13 (b) as well as IL-4 (c) gene expression (n ≥ 12, one-way ANOVA with multiple comparisons or unpaired t-test). (d–f) IL-5 (d), IL-13 (e), and IL-4 (f) levels/expression are reduced in AOB-pretreated PBMC from 3 to 5 different donors (n ≥ 6 replicates per donor, shown on the figure is unpaired t-test p value for individual donors, unpaired t-test p value for aggregated donors: p < 0.0001 for IL-5, p < 0.01 for IL-13, p < 0.001 for IL-4). (g,h) The number of CD4+ IL-5+ cells is reduced with AOB pretreatment of PBMC following Th2 differentiation cocktail stimulation; measured by flow cytometry with anti-CD4 PerCP cy5.5 and anti-IL-5 PE antibodies applied 72 h post-stimulation. (g) Representative dot plot from donor C cells showing the reduction in CD4+ and IL-5+ cells. (h) The percentage of Th2 cells as CD4+ IL-5+ are reduced with AOB pretreatment (n = 3, donor C, unpaired t-test). IL-5 (i) and IL-13 (j) supernatant levels are reduced in the presence of AOB 7 days post-stimulation with SEB (1 µg/mL), measured by ELISA (n = 3 per donor, 3 donors, unpaired t-test, p < 0.0001 for IL-5 and IL-13 for aggregated donor data sets).
We next tested if AOB modulate the Th2 polarization phenotype. PBMC from the same healthy donor were incubated with AOB 1 h prior to Th2 stimulation, and cytokines were measured by ELISA in culture supernatants 72 h after Th2 stimulation. The addition of AOB significantly reduced IL-5 and IL-13 production as compared to the samples pre-treated with vehicle (Fig. 1a,b, p < 0.01). Similarly, AOB treatment reduced the gene expression of IL-4, another key Th2 marker (Fig. 1c, p < 0.001); see “Methods” for comment on IL-4 assessments. As PBMC from different donors can model diversity in the population, we tested the effect of AOB on Th2 cytokine production from PBMC derived from four other donors (Fig. 1d,e). AOB pretreatment significantly reduced IL-5 production in 5 of 5 donors tested (Fig. 1d, p < 0.01) and IL-13 production in 3 of 5 donors (Fig. 1e, p < 0.05). AOB also reduced IL-4 expression in 3 of 3 donors tested (Fig. 1f, p < 0.001). The IL-5 and IL-13 inhibition was also observed 120 h following stimulation, suggesting temporal stability of the inhibition (Figure S2a,b, p < 0.05). These samples are from human donors with heterogeneous mixtures of cell types with complex genomic and epigenomic makeups. As such, we observe that similar amounts of Th2 stimulating compounds, delivered to similar numbers of cells, yield substantially different levels of cytokine release from these donor cells, and resulting diverse modulation by AOB. As we saw robust modulation of IL-5 across donors, we used IL-5 as a main readout for the rest of the study.
IL-5 can be generated from multiple sources, including CD4+ T cells, eosinophils and innate lymphoid cells. We thus explored whether AOB were specifically inhibiting IL-5 production in CD4+ T cells that would induce an atopic response. We immunostained Th2 stimulated PBMC with fluorescently labeled antibodies against CD4 and IL-5, and then quantified the proportion of double-positive cells with and without AOB pretreatment using flow cytometry. AOB pretreatment significantly reduced the percentage of CD4+ IL-5+ cells following Th2 stimulation (Fig. 1g,h, p < 0.05), suggesting AOB can prevent the production of Th2 associated cytokines from CD4+ T cells. Note that CD4− IL-5+ cells were also modulated, suggesting that other cells types may also contribute to the suppression of IL-5 production.
Finally, we sought to confirm the ability of AOB to mitigate Th2 polarization using a different Th2 stimulation methodology. We used Staphylococcal enterotoxin B (SEB), a potent inducer of Th2 response, and a major contributor to the pathology of atopic dermatitis30. We confirmed that SEB was able to induce IL-5 and IL-13 production in 3 of 3 donors (Figure S3). Furthermore, AOB pretreatment of PBMC 1 h prior to SEB stimulation also significantly reduced IL-5 and IL-13 production in multiple donors (Fig. 1i,j, p < 0.05) without affecting PBMC viability (Figure S1e). Overall, these data, using multiple stimulation paradigms and multiple donors, suggest that AOB can suppress the induction of the human Th2 response.
AOB-mediated Th2 inhibition is largely independent of Th1 signaling
Having established that AOB can suppress the induction of Th2 signaling, we sought to understand what upstream mechanisms could contribute to this suppression. Th1 cells can block Th2 polarization via the effector molecule IFNγ, a mechanism used by Lactobacillus to interfere with Th2 signaling17. Therefore, we first tested if AOB induce the production of IFNγ. AOB pretreatment significantly induced IFNγ production, both in unstimulated and in Th2 stimulated PBMC (by Th2 differentiation kit) (Fig. 2a, p < 0.001). This observation was replicated in PBMC from all 5 donors tested (Fig. 2b, p < 0.01).
AOB induce Th1 polarization but Th1 are not necessary for Th2 inhibition. (a–d) IFNγ (a,b) and IL-12p70 (c,d) supernatant levels are increased with AOB pretreatment of PBMC prior to Th2 kit stimulation; measured by ELISA. IFNγ (a) and IL-12p70 (c) levels are increased in PBMC from donor A (n = 9, one-way ANOVA with multiple comparisons). IFNγ (b) is induced in AOB pre-treated PBMC from 5 donors and IL-12p70 (d) is induced in PBMC from 2 of 3 donors tested (n ≥ 6 per donor, unpaired t-test, p < 0.0001 for IFNγ and p < 0.0015 for IL-12 aggregated donor datasets). (e,f) The number of CD4+ IFNγ+ cells is increased with AOB pretreatment of PBMC prior to Th2 differentiation cocktail stimulation as measured by staining with anti-CD4 PerCP cy5.5 and anti-IFNγ FITC antibodies 72 h post-stimulation. (e) Representative dot plot from donor C PBMC showing an increase in the percentage of CD4+ and IFNγ+ cells. (f) Percentage of Th1 cells as CD4+ IFNγ+ are increased with AOB pretreatment (n = 6, unpaired t-test). (g,h) Addition of IFNγ or IL-12 neutralizing antibodies to PBMC prior to AOB pretreatment does not prevent AOB inhibition of Th2. IFNγ (g) production is reduced in presence of 10 µg/mL IFNγ or IL-12 neutralizing antibodies in PBMC from 3 donors (n = 3 per donor, one point per donor, one-way ANOVA with multiple comparisons). AOB-mediated reduction in IL-5 production (h) is unaffected in presence of 10 µg/mL IFNγ or IL-12 neutralizing antibodies in PBMC from 3 donors (n = 3 per donor, one point per donor, one-way ANOVA with multiple comparisons).
Th1 polarization involves the dendritic cell-mediated release of IL-12, which in turn leads to IFNγ release from CD4+ T cells31. Therefore, we tested if AOB pretreatment specifically induced a Th1 phenotype by measuring AOB impact on (i) the DC-derived Th1-inducing cytokine IL-12 and (ii) IFNγ production by CD4+ T cells specifically. As shown in Fig. 2c, AOB pretreatment increased the levels of IL-12 in culture supernatants following a Th2 stimulus (p < 0.001), an observation validated in 2 of 3 donors (Fig. 2d). To determine if IFNγ was being produced by CD4+ T cells specifically, PBMC were immunostained with fluorescently labeled antibodies against CD4 and IFNγ and analyzed using flow cytometry. We observed a 3.5-fold increase in the proportion of CD4+ IFNγ+ cells after AOB treatment (Fig. 2e,f, p < 0.001). Altogether, these data strongly suggest that AOB induce a Th1 response.
Next, we investigated whether Th1 signaling was necessary for the AOB-mediated suppression of Th2 responses. To remove the influence of Th1 signaling, we applied either IFNγ or IL-12 neutralizing antibodies to the PBMC prior to AOB treatment and Th2 stimulation. Both IFNγ or IL-12 neutralizing antibodies drastically reduced the levels of IFNγ in the supernatant as compared to isotype controls (Fig. 2g, p < 0.05) without affecting PBMC viability (Figure S1c), thus validating that Th1 pathway output and development are suppressed, respectively. However, neither neutralizing antibody treatment significantly influenced the AOB-mediated suppression of IL-5 (Fig. 2h, p > 0.05). In sum, these data demonstrate that while Th1 responses are induced by AOB treatment, the resulting Th1 responses and IFNγ production are not major contributors on AOB-mediated inhibition of Th2 polarization.
AOB-mediated Th2 inhibition requires IL-10 and is associated with a suppression of dendritic cell activity
The ability of microbes to modulate the interaction between dendritic cells and T cells has been well established32,33,34. Cowshed bacteria can interfere with the ability of dendritic cells to promote Th2 polarization by blocking the expression of the Notch ligand Jagged-135. However, AOB did not reduce the expression of Jagged-1 (data not shown), suggesting a different mechanism is involved. Dendritic cells activate CD4+ T cells through antigen presentation via MHC II and co-stimulation factors such as CD86/CD8036,37. Therefore, we tested if AOB modulate dendritic cell activation by downregulating the surface expression levels of MHC II and CD86. PBMC were pre-treated with AOB, stimulated with the Th2 stimulus (by Th2 differentiation kit) for 72 h, then immunostained with fluorescently labeled antibodies against the dendritic cell marker CD11c and either (a) MHC II or (b) CD86 followed by flow cytometry analysis. MHC II and CD86 expression were significantly reduced in CD11c+ cells after AOB treatment in 2 of 3 donors (Fig. 3a–d). These observations suggest AOB can interfere with dendritic cell activation, which may lead to reduced antigen presentation to T cells.
AOB-mediated Th2 inhibition requires IL-10 and is associated with a suppression of dendritic cell activity. (a–d) Expression of MHC II (a,b) or CD86 (c,d) in CD11c+ cells is reduced in PBMC treated with AOB prior to Th2 differentiation cocktail stimulation; measured by flow cytometry in Th2-stimulated PBMC in the presence or absence of AOB. (a,c) Representative fluorescence intensity plots of anti-MHC II FITC (a) or anti-CD86 PE (c) stained PBMC from donor C in the presence (red) or absence (grey) of AOB. (b,d) Relative MHC II (b) or CD86 (d) expression in CD11c+ positive cells is reduced with AOB treatment in 3 donors (n = 3 per donor, unpaired t-test, p < 0.0001 for MHC II and CD86 aggregated donor datasets). (e) IL-10 production is induced by AOB in PBMC from 3 donors 24 h post-stimulation; measured by ELISA of culture supernatants (n = 3 per donor, p = 0.1095 for aggregated donor data set). (f–h) Addition of IL-10 neutralizing antibodies to PBMC prior to AOB pretreatment interfered with AOB’s inhibition of Th2. IL-10 (f) production by Th2-stimulated PBMC was reduced with the addition of IL-10 neutralizing antibody but not with isotype control in 3 donors (n = 3 per donor, one point per donor, one-way ANOVA with multiple comparisons). AOB-mediated fold reduction in IL-5 (g) was obstructed by the addition of IL-10 neutralizing antibody compared to isotype control in 2 of 3 donors tested (n = 3 per donor, unpaired t test). AOB-mediated reduction in CD86 expression (h) in CD11c+ cells is hindered with the addition of IL-10 neutralizing antibody but not with isotype control (n = 3, donor D, one-way ANOVA with multiple comparisons).
The anti-inflammatory cytokine IL-10 can interfere with MHC II antigen presentation and CD86 co-stimulation on dendritic cells38,39. We thus sought to test if AOB modulate Th2 polarization via an IL-10 mediated mechanism. We first measured IL-10 production following AOB treatment and Th2 stimulation. We observed a potentiation of IL-10 production following AOB treatment and Th2 stimulation in all three donors tested (Fig. 3e). Then, we tested if IL-10 was necessary for AOB-mediated inhibition of dendritic cell activity and the subsequent Th2 inhibition. IL-10 neutralizing antibody was applied prior to AOB treatment and Th2 stimulation. We verified that the anti-IL-10 antibody significantly reduced the levels of free IL-10 in the supernatant compared to the isotype control (Fig. 3f, p < 0.01). Interestingly, IL-10 neutralization significantly reduced AOB-mediated IL-5 inhibition in two out of the three donors tested (Fig. 3g, p < 0.01) without affecting PBMC viability (Figure S1d). We note that the donor D, which showed little response to the IL-10 antibody application, also showed the weakest inhibition of Th2 cytokines in response to AOB application following Th2 stimulation (Fig. 1d,e). Correspondingly, we observed that IL-10 neutralization also mitigated the AOB-induced suppression of CD86 expression in CD11c+ dendritic cells (Fig. 3h). Together, these data support the concept that IL-10 plays an important, though not exclusive, role in AOB-mediated Th2 inhibition, in a process that might involve interfering with dendritic cell ability to activate T cells.
AOB-mediated Th2 inhibition doesn’t involve secreted bacterial metabolites
Next, we aimed to identify the bacterial component(s) responsible for Th2 inhibition. To discriminate between secreted metabolites and cell wall/intracellular components, we compared live AOB to AOB that were washed to remove any residual secreted molecules then heat killed to prevent any further metabolic activity. We verified that heat killed AOB were unable to produce nitrite or nitric oxide, indicating their lack of metabolic activity (Fig. 4a,b, p < 0.001). However, heat killed AOB were equivalent to live AOB in inhibiting the Th2 markers IL-5 and IL-13 (Fig. 4c,d) or MHC II and CD86 expression (Fig. 4e,f).
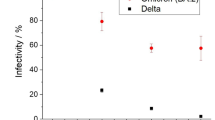
Structural components could be responsible for AOB-mediated Th2 inhibition. (a,b) AOB metabolites nitrite (a) and nitric oxide (b) are produced by live but not heat killed AOB after 1 h incubation in AOB culture media (n = 3, unpaired t-test). (c,d) Fold-reduction in IL-5 (c) and IL-13 (d) mediated by AOB (red) is not significantly different from fold-reduction mediated by heat killed AOB (blue); measured by ELISA in cell culture supernatant collected 72 h post-stimulation with the Th2 stimulation cocktail (n ≥ 6 per donor, 5 donors, one datapoint per donor, unpaired T test). (e,f) Fold reduction in MHC II (e) and CD86 (f) expression in CD11c+ cells mediated by live AOB (red) is not significantly different from fold-reduction mediated by heat killed AOB (blue); measured by flow cytometry 72 h after Th2 stimulation in donor C (n = 6, unpaired T test). (g,h) IFNγ (g) and IL-12p70 (h) production by PBMC are not as strongly induced by heat killed AOB (blue) as by live AOB (red); measured by ELISA from supernatant of PBMC culture collected 72 h post-stimulation (n ≥ 3 per donor, 3 or 5 donors, one datapoint per donor, one-way ANOVA with multiple comparisons).
Interestingly, the study of heat killed AOB further supports the differential role of Th1 polarization and dendritic cell activation. While heat killed AOB were equivalent to live AOB in regulating IL-5, MHC II, and CD86 expression (Fig. 4c,e,f), heat killed AOB induced weaker levels of expression of IFNγ and IL-12 (Fig. 4g,h).
In summary, AOB metabolic activity and associated secreted molecules, such as the immunomodulatory molecule nitric oxide, are not required for Th2 inhibition. Rather, these findings point towards a role of structural or intracellular components in mediating the effects on dendritic cells and subsequent Th2 polarization. Future studies will determine the component(s) responsible for this immune modulation, as well as its specificity compared to other bacteria.
Discussion
This study reports the immuno-modulatory properties of the ammonia oxidizing bacteria N. eutropha D23. We discovered that AOB have the ability to suppress the polarization of CD4+ T cells to a Th2 phenotype in an IL-10 dependent manner that is associated with suppression of dendritic cell activity, but is not reliant on Th1 signaling. As such, this study highlights the potential for adding AOB to human skin to treat Th2-mediated pathologies associated with atopy. To our knowledge, this is the first report describing the immuno-modulatory properties of AOB.
The results presented here point to a non-canonical mechanism by which AOB suppress Th2 polarization in a Th1 independent manner, similarly to reports of a few other bacteria35,40. While AOB can induce Th1 associated cytokines, we observed these cytokines are not a major contributor for Th2 suppression; IFNγ and IL-12 neutralizing antibodies did not prevent suppression, and suppression occurred with heat killed AOBs, which induced a weak IFNγ response.
Our data places the anti-inflammatory cytokine IL-10 at the center of AOB’s mode of action, in a process that may involve dendritic cell modulation. AOB reduced the surface levels of the proteins MHC II and CD86 involved in antigen presentation, and CD4+ T cell co-stimulation in CD11c+ dendritic cells, as shown with other immunomodulatory bacteria41. Moreover, we found the anti-inflammatory cytokine IL-10 to play a significant role in AOB-mediated Th2 suppression, as has been described for other bacteria42. We observed that IL-10 levels were increased with exposure to AOB, and more importantly, IL-10 neutralization using blocking antibodies prevented the AOB-mediated dendritic cell attenuation and the resulting Th2 suppression, an activity previously attributed to IL-1038,39. The origin of IL-10 induced by AOB, however, remains to be determined. Tolerogenic dendritic cells, Th17 cells and regulatory T cells (Tregs) are common IL-10 producers in the context of immune tolerance43. Tregs are unlikely to be involved, as AOB didn’t induce the Treg effector TGF-ß (data not shown). Moreover, the fact that AOB induce IL-10 as early as 24 h suggests production by innate immune cells. Future studies that are beyond the scope of this paper will further address this point.
Unlike the Th1- and Treg-mediated immunomodulatory mechanisms of probiotics and gut commensals6,17,44, environmental microbes such as cowshed bacteria and AOB appear to provide an alternate, additive source of signaling that is instructive to the immune system. We suggest that this alternate, instructive signaling can have important influences on the development of atopy45.
Exposure to environmental microbe components has long been associated with decreased prevalence of atopic diseases6,7,45. Multiple types of bacterial immuno-modulatory molecules have been identified, from metabolites (e.g. SCFAs, indoles) to cell wall constituents (e.g. LPS, PSA) and nucleic acids (e.g. CpG DNA, RNA)6,46. AOB’s ability to block Th2 polarization doesn’t seem to rely on metabolites, as heat killed AOB appeared as effective as live AOB. Therefore, the immuno-modulatory molecule nitric oxide produced by AOB is unlikely to be involved in this phenotype. We suspect that TLRs are involved in the AOB mechanism of action; future studies will test the relative activity of AOB on TLRs and aim to identify the bacterial substrates that imbue AOB with their immunomodulatory activity(s).
Atopic diseases such as atopic dermatitis, allergic rhinitis, and asthma involve an uncontrolled type 2 inflammatory response mediated by the Th2 cytokines IL-5, IL-13, and IL-4. IL-13 and IL-4 lead to the production of IgE and other mediators responsible for hypersensitivity reactions, tissue damage, and inflammatory reactions. IL-13 and IL-4 also bind to specific receptors at the surface of sensory neurons and play a role in promoting itch47. IL-5 is involved in eosinophil activation, effectors of which lead to tissue damage48,49. Previous approaches suggested that the efficacy of targeting end mediators/effectors was not as widespread across atopic diseases as blocking upstream Th2 cytokines (e.g. IL-5, IL-13, IL-4)14. Based on the ability of AOB to modulate all three major Th2 cytokines, we hypothesize that AOB have the potential to influence atopic disease by blocking both IgE and eosinophil pathways, as well as interfering with itch signaling. However, future studies will be required to determine if AOB indeed have this activity.
Potential limitations to this study include the reliance on Th2 stimuli that do not fully mimic the diseased state, as well as the use of immune cells with which an environmental microbe would not frequently come into close contact. However, our observation that AOB suppress Th2 polarization mediated by Staphylococcal enterotoxin B (SEB) provides confidence that our results are not due to spurious activity of a proprietary Th2 stimulation cocktail. Furthermore, and more importantly, the SEB observations reinforce AOB’s clinical potential due to the relevance of Staphylococcus aureus and SEB in atopic dermatitis. In this disease, one might expect dermally applied AOB to encounter immune cells in a manner similar to our study, as patients often breach the skin barrier in response to the intense itch associated with SEB. Future preclinical and clinical studies will provide more insight on whether AOB-mediated Th2 inhibition can translate into disease modifying phenotypes in atopic disease.
Heat killed AOB, which retain immuno-modulatory activity, might be leveraged to prevent colonization and potential adverse events commonly associated with live bacterial products50. Moreover, their lower Th1 induction could be beneficial in the context of atopic diseases with a Th1 component (e.g. celiac disease) or atopic patients also suffering from Th1-mediated diseases (e.g. multiple sclerosis, type 1 diabetes)51.
In conclusion, the ammonia oxidizing bacteria N. eutropha D23 shows promising therapeutic potential to target atopic diseases due to its ability to block Th2 polarization and key cytokines involved in IgE production, eosinophilia, and itch. Follow up studies will provide more insights into its detailed mode of action and clinical potential.
Methods
Bacteria and PBMC
Nitrosomonas eutropha D23 is a unique strain of ammonia-oxidizing bacteria (AOB) manufactured by AOBiome Therapeutics. AOB were washed in PBS (Gibco) prior to being used for PBMC treatment. Heat killed AOB were prepared by first washing live AOB in PBS and then incubating AOB at 60 °C for 2 h.
Human PBMC were purchased from ATCC. 5 different PBMC donors were used with the following lot numbers from ATCC: 80227190 (donor A), 80424333 (donor B), 80819190 (donor C), 80424222 (donor D), and 80808190 (donor E).
PBMC stimulation and treatments
PBMC were seeded at a concentration of 7–8 × 106 cells/mL in RPMI 1640 medium without phenol red and glutamine (Gibco) supplemented with 10% heat-inactivated FBS (Gibco) and 2 mM glutamax (Gibco) and incubated at 37 °C with 5% CO2 overnight. AOB were added at a ratio of four bacteria per PBMC 1 h prior to Th2 stimulation. PBMC were then stimulated using either the CellXvivo human Th2 differentiation kit (R&D systems) following the manufacturer’s recommendations, or 1 µg/mL SEB (Sigma). Where appropriate, neutralizing antibodies were used at 10 µg/mL and refreshed daily until sample collection. The following neutralizing antibodies were used: mouse anti-human IFNγ clone K3.53 (MAB2852), mouse anti-human IL-12p70 clone 24910 (MAB219), mouse anti-human IL-10 clone 948505 (MAB9184) and the isotype controls mouse IgG2a (MAB003) and mouse IgG1 (MAB002) (all from R&D systems).
Samples were collected 3 days post-stimulation (unless otherwise indicated) by spinning down cells at 500×g for 10 min. Cell-free supernatants were frozen at – 20 °C for later cytokine quantification and cell pellets were processed for PBMC viability, RNA extraction or flow cytometry analyses as described below.
PBMC viability
PBMC viability was determined by measuring cell metabolic activity using WST-1 as described by Klinder et al.52. Briefly, 50 µl aliquots of cells were transferred into a 96 well plate, diluted twofold with PBMC culture media and supplemented with 10% WST-1 reagent (Roche) according to manufacturer’s instructions. Samples were incubated for 1 h at 37 °C with 5% CO2 and OD440nm and OD650nm were then measured using a 96-well plate spectrophotometer (Molecular Devices or BioTek). OD650nm was subtracted from OD440nm then percent viability was calculated relative to the no treatment condition.
PBMC viability was also confirmed using LIVE/DEAD flow cytometry staining. 1 × 106 cells were washed twice in PBS and stained with the LIVE/DEAD Fixable Green Dead Cell Stain kit for 488 nm excitation (Invitrogen) following the manufacturer’s instructions. Cells were incubated in the dark for 30 min, washed twice in PBS + 1% BSA then analyzed using a BD Accuri C6 flow cytometer. Data were quantified using FlowJo 10 software.
Cytokine quantification by ELISA
Supernatant samples were diluted in PBMC culture media prior to being assayed in order to be in the ELISAs’ dynamic range. ELISAs were then performed following manufacturer’s instructions and cytokine concentrations were calculated based on a linear regression of the standard curve. IL-5, IL-13 and IL-12 p70 ELISA kits were purchased from R&D systems, IFNγ and IL-10 from BD Biosciences).
Flow cytometry analysis of surface and intracellular markers
For intracellular quantification of IFNγ or IL-5, cells were treated with 4 µM Golgistop (BD Bioscience) to block protein secretion 14 h prior to sample collection. In the case of IL-5, cells were also treated with 81 nM PMA and 1.3 µM ionomycin (eBioscience) 5 h prior to sample collection to increase cytokine detection threshold. Cells were then washed twice in FBS buffer (BD Bioscience), fixed in BD cytofix (BD Bioscience), washed twice in FBS buffer and frozen at − 80 °C in 90% heat inactivated FBS – 10% DMSO until further analysis. Thawed cells were then washed twice in FBS buffer and permeabilized with BD perm/wash buffer (BD Bioscience). For IL-5 staining, cells were blocked with 4 µg of unlabeled rat IgG1 clone R3-34 antibody (BD bioscience). 1 × 106 cells were then stained with the following antibodies: mouse anti-human CD4 PerCP clone SK3 antibody (20 µL), mouse anti-human IFNγ FITC clone B27 (20 µL), rat anti-human IL-5 PE clone TRFK5 (5 µL) and their respective isotypes mouse IgG1 FITC clone MOPC-21 (20 µL) and rat IgG1 PE clone R3-34 (5 µL) (all from BD Bioscience). Stained cells were then washed twice in perm/wash buffer then resuspended in FBS buffer and analyzed on a BD Acuri C6 flow cytometer (BD Bioscience), and data were quantified using FlowJo 10 software.
For quantification of the surface markers MHC II and CD86, cells were washed twice with FBS buffer. 1 × 106 cells were then stained with the following antibodies: mouse anti-human MHC II FITC clone Tu39 (20 µL), mouse anti-human CD86 PE clone 2331 (FUN-1) (20 µL), mouse CD11c APC clone B-ly6 (20 µL) and their respective isotypes mouse IgG2a FITC clone G155-178 (20 µL), mouse IgG1 PE clone MOPC-21 (20 µL) and mouse IgG1 APC clone MOPC-21 (all from BD Bioscience). Stained cells were then washed twice in FBS buffer then resuspended in FBS buffer and analyzed on a BD Acuri C6 flow cytometer (BD Bioscience), data were quantified using FlowJo 10 software.
Gene expression analysis by RTqPCR
Due to the presence of high levels of IL-4 in the Th2 differentiation kit preventing a robust estimate of AOB impact on IL-4 production, IL-4 production was measured by RTqPCR to selectively quantify cellular IL-4. PBMC were washed in PBS then subjected to RNA extraction using the Qiagen RNAeasy extraction kit including the QIAshredder homogenization step following manufacturer’s recommendations. RNA was then reverse-transcribed into cDNA using the Invitrogen SuperScript III First strand synthesis system for RTqPCR following the manufacturer’s protocol with oligo dT primers. Gene expression was then measured by qPCR using the PowerUp SYBR Green Master Mix (Applied Biosystems) and QuantStudio 3 or 6 Flex (ThermoFisher Scientific) following manufacturer’s recommendations. qPCR reactions were performed in a final volume of 25 µL with an annealing temperature of 55 °C for 40 cycles. The following primer sequences were used: IL-4 (F: CCAACTGCTTCCCCCTCTG, R: TCTGTTACGGTCAACTCGGTG; sequences from PrimerBank53), EF-1a (F: CTGAACCATCCAFFCCAAAT, R: GCCGTGTGGCAATCCAAT54). Relative gene expression was calculated using the 2−ddCt method55 using EF-1a as a housekeeping gene54.
Bacterial metabolite quantification
Nitrite and nitric oxide production were measured to determine the metabolic activity of live or heat killed AOB. Nitrite was quantified using the Griess assay. Briefly, samples were mixed 1:1 with a solution of equal volumes Griess Reagent A (1.5 N Hydrochloric Acid, 58 mM Sulfanilamide) and Griess Reagent B (0.77 mM NNEQ), incubated for 20 min at room temperature protected from light then quantified by measuring OD540nm using a 96 well plate spectrophotometer. Concentrations of nitrite were then calculated based on a standard curve of sodium nitrite. Nitric oxide was quantified using the fluorescent dye DAF-2 (Abcam). Briefly, samples were mixed 1:1 with PBMC/AOB culture media containing 5 µM DAF-2 and incubated at 37 °C with 5% CO2 for 1 h. A standard curve of the fluorescent molecule DAF-2T (Abcam) was used to quantify nitric oxide production. Measurements were either taken after 1 h in AOB culture media or 72 h in PBMC culture media.
Statistical and data analysis
As bacterial interventions affect host physiology based on the variable genetic makeup of the host, we have chosen to analyze comparisons within donors, as opposed to across donors. The numbers of donors tested in this study would not offer sufficient statistical power to make proper inferences; clinical studies often require patient numbers in the 100 s, even when measuring clinical biomarker samples using ELISAs following use of drugs with a known mechanism of action. Moreover, the samples studied are from human donors with heterogeneous mixtures of cell types with complex genomic and epigenomic makeups. As such, we observe that similar amounts of Th2 stimulation to similar numbers of cells yield substantially different levels of cytokine release from these donor cells, and resulting diverse modulation by AOB (e.g. Fig. 1d,i). Thus, we sought to balance the true diversity of signaling (and indeed, AOB activity) on these populations versus clarity of presenting the experimental effects by a) presenting the absolute values in the Fig. 1 and Table S1, and b) presenting the normalized levels relative to the Th2 stimulation baseline condition in later figures.
One-way analysis of variance (ANOVA) with Tukey multiple comparison correction or unpaired t-test were performed when appropriate, as indicated in the figure legends, using Graphpad Prism 8 software (Graphpad Software Inc).
References
Pawankar, R. Allergic diseases and asthma: A global public health concern and a call to action. World Allergy Organ. J. 7, 12 (2014).
Rook, G. A. W. Hygiene hypothesis and autoimmune diseases. Clin. Rev. Allergy Immunol. 42, 5–15 (2012).
Yazdanbakhsh, M., Kremsner, P. G. & Van Ree, R. Immunology: Allergy, parasites, and the hygiene hypothesis. Science 296, 490–494 (2002).
Strachan, D. P. Hay fever, hygiene, and household size. Br. Med. J. 299, 1259–1260 (1989).
Braun-Fahrländer, C. et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N. Engl. J. Med. 347, 869–877 (2002).
Jatzlauk, G., Bartel, S., Heine, H., Schloter, M. & Krauss-Etschmann, S. Influences of environmental bacteria and their metabolites on allergies, asthma, and host microbiota. Allergy Eur. J. Allergy Clin. Immunol. 72, 1859–1867 (2017).
Sbihi, H. et al. Thinking bigger: How early-life environmental exposures shape the gut microbiome and influence the development of asthma and allergic disease. Allergy Eur. J. Allergy Clin. Immunol. 74, 2103–2115 (2019).
Scudellari, M. Cleaning up the hygiene hypothesis. Proc. Natl. Acad. Sci. USA. 114, 1433–1436 (2017).
Biedermann, T., Skabytska, Y., Kaesler, S. & Volz, T. Regulation of T cell immunity in atopic dermatitis by microbes: The Yin and Yang of cutaneous inflammation. Front. Immunol. 6, 1–9 (2015).
Rook, G. A. W. & Brunet, L. R. Microbes, immunoregulation, and the gut. Gut 54, 317–320 (2005).
Belkaid, Y. & Hand, T. W. Role of the microbiota in immunity and inflammation. Cell 157, 121–141 (2014).
Donkor, O. N., Shah, N. P., Apostolopoulos, V. & Vasiljevic, T. Development of allergic responses related to microorganisms exposure in early life. Int. Dairy J. 20, 373–385 (2010).
Ristori, G., Buttinelli, C., Pozzilli, C., Fieschi, C. & Salvetti, M. Microbe exposure, innate immunity and autoimmunity. Cell 20, 54 (1999).
Gandhi, N. A. et al. Targeting key proximal drivers of type 2 inflammation in disease. Nat. Rev. Drug Discov. 15, 35–50 (2016).
Lim, S. K. et al. Weissella cibaria WIKIM28 ameliorates atopic dermatitis-like skin lesions by inducing tolerogenic dendritic cells and regulatory T cells in BALB/c mice. Sci. Rep. 7, 1–9 (2017).
Smelt, M. J. et al. Probiotics can generate FoxP3 T-cell responses in the small intestine and simultaneously inducing CD4 and CD8 T cell activation in the large intestine. PLoS ONE 8, e68952 (2013).
Pochard, P. et al. Lactic acid bacteria inhibit TH2 cytokine production by mononuclear cells from allergic patients. J. Allergy Clin. Immunol. 110, 617–623 (2002).
Mazmanian, S. K., Cui, H. L., Tzianabos, A. O. & Kasper, D. L. An immunomodulatory molecule of symbiotic bacteria directs maturation of the host immune system. Cell 122, 107–118 (2005).
Kauth, M. & Heine, H. Allergy protection by cowshed bacteria—Recent findings and future prospects. Pediatr. Allergy Immunol. 27, 340–347 (2016).
Vuitton, D. A. & Dalphin, J. C. From farming to engineering: The microbiota and allergic diseases. Engineering 3, 98–109 (2017).
Debarry, J. et al. Acinetobacter lwoffii and Lactococcus lactis strains isolated from farm cowsheds possess strong allergy-protective properties. J. Allergy Clin. Immunol. 119, 1514–1521 (2007).
Cavagnaro, T. R., Jackson, L. E., Hristova, K. & Scow, K. M. Short-term population dynamics of ammonia oxidizing bacteria in an agricultural soil. Appl. Soil Ecol. 40, 13–18 (2008).
Wessén, E. et al. Spatial distribution of ammonia-oxidizing bacteria and archaea across a 44-hectare farm related to ecosystem functioning. ISME J. 5, 1213–1225 (2011).
Bogdan, C. Nitric oxide and the immune response NO production in the immune system. Nat. Immunol. 2, 907–916 (2001).
Arp, D. J., Sayavedra-Soto, L. A. & Hommes, N. G. Molecular biology and biochemistry of ammonia oxidation by Nitrosomonas europaea. Arch. Microbiol. 178, 250–255 (2002).
Whitlock, D. R. & Feelisch, M. Soil bacteria, nitrite and the skin. In The Hygiene Hypothesis and Darwinian Medicine 103–115 (Birkhäuser Basel, 2009). https://doi.org/10.1007/978-3-7643-8903-1_6.
Oh, J. et al. Biogeography and individuality shape function in the human skin metagenome. Nature 514, 59–64 (2014).
Ma, Y. et al. Human papillomavirus community in healthy persons, defined by metagenomics analysis of human microbiome project shotgun sequencing data sets. J. Virol. 88, 4786–4797 (2014).
Prete, G. D. Human Th1 and Th2 lymphocytes: Their role in the pathophysiology of atopy. Allergy 47, 450–455 (1992).
Strange, P. Staphylococcal enterotoxin B applied on intact normal and intact atopic skin induces dermatitis. Arch. Dermatol. 132, 27 (1996).
Heufler, C. et al. Interleukin-12 is produced by dendritic cells and mediates T helper 1 development as well as interferon-γ production by T helper 1 cells. Eur. J. Immunol. 26, 659–668 (1996).
Kapsenberg, M. L. et al. Microbial compounds selectively induce Th1 cell-promoting or Th2 cell-promoting dendritic cells in vitro with diverse Th cell-polarizing signals. J. Immunol. Ref. 168, 1704–1709 (2002).
Drakes, M., Blanchard, T. & Czinn, S. Bacterial probiotic modulation of dendritic cells. Infect. Immun. 72, 3299–3309 (2004).
Pulendran, B. Modulating Th1/Th2 responses with microbes, dendritic cells, and pathogen recognition receptors. Immunol. Res. 29, 187–196 (2004).
Sun, J., Krawczyk, C. J. & Pearce, E. J. Suppression of Th2 cell development by Notch ligands Delta1 and Delta4. J. Immunol. 180, 1655–1661 (2008).
Steinman, R. M. The dendritic cell system and its role in immunogenicity. Annu. Rev. Immunol. 9, 271–296 (1991).
Ingulli, E., Mondino, A., Khoruts, A. & Jenkins, M. K. In vivo detection of dendritic cell antigen presentation to CD4+ T cells. J. Exp. Med. 185, 2133–2141 (1997).
Buelens, C. et al. Interleukin-10 differentially regulates B7–1 (CD80) and B7–2 (CD86) expression on human peripheral blood dendritic cells. Eur. J. Immunol. 25, 2668–2672 (1995).
Mittal, S. K., Cho, K.-J., Ishido, S. & Roche, P. A. Interleukin 10 (IL-10)-mediated Immunosuppression: March-1 induction regulates antigen presentation by macrophages but not dendritic cells. J. Biol. Chem. 290(45), 27158–27167. https://doi.org/10.1074/jbc.M115.682708 (2015).
Iwabuchi, N., Takahashi, N., Xiao, J., Miyaji, K. & Iwatsuki, K. In vitro Th1 cytokine-independent Th2 suppressive effects of bifidobacteria. Microbiol. Immunol. 51, 649–660 (2007).
McAdam, A. J., Schweitzer, A. N. & Sharpe, A. H. The role of B7 co-stimulation in activation and differentiation ofCD4+and CD8+ T cells. Immunol. Rev. 165, 231–247 (1998).
Schülke, S. Induction of interleukin-10 producing dendritic cells as a tool to suppress allergen-specific T helper 2 responses. Front. Immunol. 9, 455 (2018).
Couper, K. N., Blount, D. G. & Riley, E. M. IL-10: The master regulator of immunity to infection. J. Immunol. 180, 5771–5777 (2008).
Rooks, M. G. & Garrett, W. S. Gut microbiota, metabolites and host immunity. Nat. Rev. Immunol. 16, 341–352 (2016).
Stein, M. M. et al. Innate immunity and asthma risk in Amish and Hutterite farm children. N. Engl. J. Med. 375, 411–421 (2016).
Postler, T. S. & Ghosh, S. Understanding the holobiont: How microbial metabolites affect human health and shape the immune system. Cell Metab. 26, 110–130 (2017).
Mack, M. R. & Kim, B. S. The itch-scratch cycle: A neuroimmune perspective. Trends Immunol. 39, 980–991 (2018).
Desreumaux, P. & Capron, M. Eosinophils in allergic reactions. Curr. Opin. Immunol. 8, 790–795 (1996).
Abu-Ghazaleh, R. I., Kita, H. & Gleich, G. J. Eosinophil activation and function in health and disease. Immunol. Ser. 57, 137–167 (1992).
Sanders, M. E. et al. Safety assessment of probiotics for human use. Gut Microbes 1, 1–22 (2010).
Walker, L. S. K. & Von Herrath, M. CD4 T cell differentiation in type 1 diabetes. Clin. Exp. Immunol. 183, 16–29 (2015).
Klinder, A., Seyfarth, A., Hansmann, D., Bader, R. & Jonitz-Heincke, A. Inflammatory response of human peripheral blood mononuclear cells and osteoblasts incubated with metallic and ceramic submicron particles. Front. Immunol. https://doi.org/10.3389/fimmu.2018.00831 (2018).
Spandidos, A., Wang, X., Wang, H. & Seed, B. PrimerBank: A resource of human and mouse PCR primer pairs for gene expression detection and quantification. Nucleic Acids Res. https://doi.org/10.1093/nar/gkp1005 (2009).
Stott, B. et al. Human IL-31 is induced by IL-4 and promotes TH2-driven inflammation. J. Allergy Clin. Immunol. 132, 446–54.e5 (2013).
Livak, K. J. & Schmittgen, T. D. Analysis of relative gene expression data using real-time quantitative PCR and the 22DDCT method. Methods 25(4), 402–408 (2001).
Acknowledgements
We would like to thank AOBiome Therapeutics for providing the funding and resources for this study as well as all AOBiome’s team members, particularly Daniel Brownell, Judith Ng-Cashin, Ioannis Gryllos, Chris Johnson, and Neeraja Vajrala. Additionally, we would like to acknowledge Robrecht Thoonen and Anita Hartog for their advice and review of the manuscript.
Author information
Authors and Affiliations
Contributions
A.G. and D.M. contributed to the design and concept; D.M. and N.E. conducted the experiments; all authors contributed to results analysis, interpretation, and final manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors were employed by AOBiome Therapeutics at the time of this study; AOBiome Therapeutics is currently investigating the clinical use of AOB for treatment of atopic dermatitis.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Maura, D., Elmekki, N. & Goddard, C.A. The ammonia oxidizing bacterium Nitrosomonas eutropha blocks T helper 2 cell polarization via the anti-inflammatory cytokine IL-10. Sci Rep 11, 14162 (2021). https://doi.org/10.1038/s41598-021-93299-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-93299-1
This article is cited by
-
Delivery of a sebum modulator by an engineered skin microbe in mice
Nature Biotechnology (2024)
-
The gut virome is associated with stress-induced changes in behaviour and immune responses in mice
Nature Microbiology (2024)
-
Disease modification in inflammatory skin disorders: opportunities and challenges
Nature Reviews Drug Discovery (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.