Abstract
Artificial vascular treatment is an emerging interdisciplinary subject of medicine. Although the use of artificial vessels has led to many successful advancements, blood clotting remains a major challenge, especially in terms of mural clots created along the vessel wall that do not completely block the vessel. The main objective of this study is to present a method for declotting artificial vessels. This research introduces a novel thrombectomy technique in artificial vessels by employing nano-magnetic particles under a rotating magnetic field to remove mural clots in artificial vessels. A mathematical model describes the relationship between process parameters. In vitro tests confirm the feasibility of nano-magnetic thrombectomy in cleaning and declotting artificial vessels. The results show that the clot fragments are nano-sized, which eliminates the risk of distal emboli as a concern of using current atherectomy techniques. Meanwhile, no damage to the artificial vessels is observed. The results show that the frequency of rotating the magnetic field has the greatest effect on clot removal. The conceptual principles stated in this study also have the potential to be used in other vascular depositions, such as the accumulation of lipids, and calcification atherosclerosis.
Similar content being viewed by others
Introduction
Since Nicholas Eck first employed vascular anastomosis in dogs in the early 1900s1, there has been a great interest in artificial blood vessels due to the escalating number of cardiovascular disease patients2. Researchers have found that synthetic grafts are a viable solution for reopening closed or narrow blood vessels to restore blood flow3 due to some merits of these grafts, including replacing the requirement to use autologous veins, shortening the length of surgery, and reducing morbidity associated with vein harvesting2. Although employing artificial vascular streamlines the procedure of restoring normal blood flow, some drawbacks have limited its practice. Higher tendency to clot formation than autologous veins is one of the greatest barriers to use the artificial grafts4. Dissimilarity of dynamic surface topography with natural arteries, lack of actively wrinkling in response to blood pressure5, the chemical composition of the vessel surface, and the absence of viable endothelial cells (EC) on the surface of artificial grafts are the main reasons for the stimulation of clot formation6. The great number of artificial veins makes this issue even more important. Arteriovenous grafts and arteriovenous fistulas face thrombosis approximately 1 and 0.3 times per year, respectively7. Moreover, thrombosis occasionally leads to multiple missed dialysis sessions, and so endovascular declotting should be performed7.
Currently, many researchers have tried to optimize the fabrication of grafts with hemocompatible materials to prevent clotting8. Methods employed for this purpose include applying a layer of gelatin and tropoelastin9 or wrinkling the synthesized grafts8 to mimic a normal and healthy artery. In addition, the most recent generation of artificial blood vessels employs a drug-containing coating on the inner surface of the vessel to reduce the risk of clotting10. Although finding new materials to synthesize vessels is considered a Holy Grail, it will take a long time to find the best materials for this purpose, and patients cannot wait for that time. Therefore, there is a strong desire to develop effective approaches to eliminating clots in artificial veins.
Various declotting approaches (including the lyse-and-wait technique, thrombo-aspiration, pulse spray aided pharmacomechanical thrombolysis, and use of mechanical thrombectomy devices7) can be categorized as either mechanical or chemical processes (or a combination of both)11. In chemical processes, a drug agent, such as tPA, is injected into the artificial vessels to dissolve the clot12. However, bleeding often occurs, which is one of the major problems associated with the administration of thrombolytic agents, especially in the mural thrombi, where the vein is not completely blocked. Mechanical thrombectomy involves running a catheter to the site of the blockage to remove the clot via one of several marketed devices13.
Mechanical devices have been developed for or adapted to perform declotting. Such devices contain a rotating expandable basket that macerates the thrombus as it spins at 3000 revolutions per minute (rpm)7. Despite the success of mechanical thrombectomy, its complexity and negative consequences in some patients have restricted its use13. Moreover, the most important concern related to mechanical thrombectomy is distal embolism by fragments during the shaving process14. Furthermore, the forces required to navigate catheters into the artificial vessels against the flow of blood circulation can lead to side effects15. All antrectomy techniques require a catheter, which limits this method’s use, especially in small vessels (typically with a diameter of less than 10 mm).
Therefore, there is a trend towards favoring miniaturization therapy16, as inserting a catheter inside a blood vessel can cause some risks, including potential damage to the vascular surface, injury at the site of puncture, and infection17. Meanwhile, a graft is a foreign material and can cause an infection. Artificial vessels can lead to terrible complications that are significantly associated with morbidity and mortality, occurring in approximately 1–2 cases out of every 10018. The infection flows through the bloodstream, causing fevers, and weight loss19. Unlike a natural vascular surgical operation, which is a clean operation, the chance of infection when an artificial graft is used is a serious issue because vascular surgery patients are often elderly, and so the infection might interact with a variety of internal underlying diseases, such as immune system weakness20 or heart disease19.
Infections in artificial veins can sometimes lead to its replacement21 or even serious organ damage20. The epidermis is the primary source of bacteria. Possibilities include administering more powerful antibiotics either parenterally or via incorporation into the surface of the arterial vessel for designing a prolonged release local delivery system18. However, antibiotics are often not sufficient to clear infections. In most cases, artificial vessels need to be removed. If infected grafts are not detached, many of them will be gradually deteriorated leading to a vessel breakdown22. Staphylococci—predominantly S. aureus—are the most commonly implicated pathogens, with S. aureus being responsible for up to 55% of all deep wounds and graft infections22. Due to the fact that some nanoparticles (NPs) have antibacterial properties such as zinc oxide, so the making of antibacterial properties in artificial grafts with the help of NPs can be useful23.
In addition—and most importantly—current technologies are perfect for removing clots that completely block a vessel, but have problems in removing mural thrombi on the walls of vessels. While conventional vascular therapies face major challenges in declotting artificial vessels, new therapeutic techniques, in principle, are very desirable.
Nanotechnology also has enormous potential for creating new mechanisms for treatment of patients, such as thrombosis24. Researchers have shown that nanoparticles can carry thrombolytic agents to dissolve clots inside a vessel (a promising approach to minimize the side effects of the drug)25. Magnetic nanoparticles are one of the most significant candidates between nanoparticles because of their great merits such as magnetic resonance imaging (MRI), Magnetic drug targeting, biocompatibility, magnetic hyperthermia26. Furthermore, it is possible to control the movement in a flow (as the bloodstream) of magnetic nanoparticles inside a vessel under a magnetic field for several applications27. Although most researchers have focused on drug delivery by magnetic nanoparticles to treatment of thrombosis, new strategies can also be developed based on nanotechnology.
This research describes the principles behind a novel nano-magnetic thrombectomy (NMT) method to clean artificial vessels without needing to insert a large rotating mechanical device or drug agents. The proposed method is based on employing nano-magnetic particles to abrade clots under rotating magnetic pressure. A mathematical model is used to show the relationship between parameters, and the in vitro test results are discussed.
Materials and methods
Device principles and description of components
The principle of nano-magnetic thrombectomy
This section introduces the concept of using nano-catheter-less thrombectomy via nano-magnetic particles to overcome the inherent limitations of conventional thrombectomy techniques. In this process, nano-magnetic particles are injected into the veins and float through the capillary vessels, eventually reaching the target site (by means of a magnetic field or blood flow).
The presented technique (NMT) is a debulking technique by which a magnetic field is employed to apply force to the magnetic particles against the clot surface so that the particles can penetrate the clot surface. Then, the magnetic particles follow the rotation of the magnetic field. As a result, a relative motion occurs between the nano-magnetic particles and the clot surface, causing the clot to be broken into small fragments. The schematic of this process is shown in Fig. 1. (Fig. 1A shows the schematic of injecting the nano-magnetic particles into the artificial graft in clot zone, Fig. 1B displays rotating of magnet around the artificial graft, Fig. 1C shows the forces in process and Fig. 1D displays the ablating the clot due to vertical and horizontal forces and removing the clot from the surface of the artificial graft). Finally, the fate of fragments and nano-magnetic particles (both are in nano-scales) is clearance by the liver, kidney, and lungs.
A schematic of nano-magnetic thrombectomy. (A) (step 1) Injecting the magnetic nanoparticles into the artificial graft in clot zone. (B) (step 2) Rotating of the magnet around the artificial graft. (C) (step 3) The magnetic field creates a normal force (Fn) and causes the magnetic particles to be pressed on the surface of the clot, and the driving of the magnetic field leads to moving of nanoparticles (creating a tangential force (Ft)). (D) (step 4) Ablating the clot due to vertical and horizontal forces and removing the clot from the surface of the artificial graft.
System description
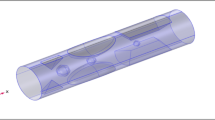
A prototype of nano-magnetic thrombectomy is designed and manufactured to ablate clots as shown in Fig. 2 (Fig. 2A shows the draft of design system, Fig. 2B displays the artificial graft is inserted into the opening of the device and magnet moves around the graft and Fig. 2C shows the image details of manufactured prototype machine). In design, two conditions must be taken into consideration in debulking a clot. The first is related to sufficient penetrating force (normal force), which is prepared by a magnet (permanent or electromagnet); the other is related to the cutting force (tangent force), which is generated by the relative motion between the nano-particles and the mural clot surface and is produced by the movement of step motors and mechanical tools. The device has three main parts, including a mechanical rotating system, a control board, and a magnetic system.
(A) The draft of the design system to operate rotate magnetic nanoparticle around the artificial graft. (B) The artificial graft is inserted into the opening of the device and the magnet moves around the graft. (C) The image of the manufactured prototype machine. 1: Head of the machine. 2: Machine mount (magnets). 3: Arterial vessel. 4: Output fluid collection. 5: Fixtures for vessel placement 6: HMI and PLC.
When a rotating system is used, there are several options for achieving the necessary motion; however, a sun gear wheel system is employed to rotate the head of the device (including magnets) around the human body or organ (vessels are located at the center). Meanwhile, the magnets can move along the radius of the head to adjust the intensity of the magnetic field. On the control board, a Programmable logic controller (PLC) is employed to control the stepping motors for rotating the sun gear with high precision. A computer program is written for different plans and guides the movement of the head using different strategies, one of which is rotating the head of the device at a special angle in harmony with the mural thrombi geometry to prevent damage to the vessels.
In this research, a permanent magnet is employed because an electromagnet in the same magnetic field density as the permanent magnet is too heavy for rotation to occur and makes the device unstable at high rotation speeds. The structure and body of the machine are made of aluminum to prevent magnetic interference. The details of the nano-magnetic ablating system are shown in Table 1.
Materials
In order to synthesis zinc ferrite nanoparticles, ZnCl2, FeCl3, and sodium hydroxide were purchased from Merck. Sterile water and normal saline serum as diluent was prepared from the Iranian Parenteral and Pharmaceutical Company (Tehran, Iran). A cubic neodymium magnet with 0.4 T was also employed. Artificial vessels made of Teflon with diameter of 6 mm is used from JOTEC GmbH.
Synthesis of nanoparticles of zinc ferrite (ZnFe2O4)
Co-precipitating technique was employed to synthesize zinc ferrite by mixing the aqueous solutions of ZnCl2 and FeCl3, according to a previous research28. Initially, ZnCl2 (1 M) and FeCl3 (2 M) were dissolved separately in 32 mL of distilled water and stirred well and kept at 60 °C. Thereafter, the mixture was added to the solution of NaOH (1 M) to pH reach to 10 at the temperature of 80 °C for 2 h, following by stirring until brown precipitate was obtained. The prepared nanoparticles were consequently washed several times with distilled water and then collected by magnet. Finally, the synthesized powder was dried at 75 °C for 24 h in a hot air oven.
Characterization of nanoparticles
The particle size and particle size distribution as well as the morphology of nanoparticles were evaluated by transmission electron microscopy (TEM) (JEM-2000 EX II; JEOL, Tokyo, Japan). Magnetization properties were measured by vibrating Sample Magnetometer (VSM 7400 Lake Shore) and X-ray diffraction (The D8 ADVANCE X-ray Spectrometer, a Copper X-ray tube operated at 40 kV and 40 mA, manufactured by Brucker Co.) technique to identify the crystalline phases. Moreover, size distribution of ZnFe2O4 NPs in suspension (normal saline) was performed using Dynamic Light Scattering (DLS) and Zeta potential using Zetasizer 3000HS (Malvern Instruments, Malvern, Worcestershire, UK).
Blood clot
Human blood was acquired from healthy students between 18 and 25 years old according to the Helal Ahmar Ethics Committee (students who voluntarily participate in human subject research after giving informed consent to be the subject of the research). The clots were produced by reaction of 1 mL blood with 200 µL of 0.2 mol L−1 CaCl2. To create dynamic conditions (where liquid flows), an artificial vessel with a diameter of 6 mm made of Teflon was employed while one side was connected to a reservoir in height of 1.5 m, to prepare the optional pressure and the other side was connected to the output tank to collect the liquid output including separated or dissolved clot. To prepare mural clot, the mixture of blood and CaCl2 were added into the artificial vessel while a piston was in the middle (with diameter of 2 mm), after forming the mural clot, the semi piston was detached carefully. Eventually the clot covered the inner of artificial vessel. To evaluate the rate of declotting, artificial clotted vessels was weighted before and after the NMT process as below:
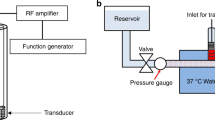
Experimental procedure
The goals of the experiments were to evaluate the possibility of NMT, examine the influence of fragment size, and study the effect of important parameters in the process. To gain a better understanding of the mechanism, a transparent tube, alongside the artificial vein, was used to observe the process in detail. In addition, the flow of normal saline in artificial clotted vessels was measured and compared to a clot-free state for a different process times. The in vitro assays were performed within 5 min and in triplicate. Meanwhile, 30 mg mL−1 of zinc ferrite (dispersed in normal saline)was used for each test. To estimate the size of fragments, the passed liquid was collected and the size of fragments were then estimated via dynamic light scattering (DLS). To study the probability of vessel surface injury, field-emission scanning electron microscope (FSEM)(Carl Zeiss Supra 55VP, Germany) images were taken from the surface of the artificial vein and transparent tube (in this case, the artificial vein and the transparent tube—both free of clots—were subjected to the NMT process for 12 h).
MTT assay
The in vitro cytotoxicity of the ZnFe2O4 NPs was estimated using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay on epithelial cells. Epithelial cells were seeded on 96-well plates at a density of 4 × 104 cells per mL and were incubated for 24 h in Dulbecco’s modified Eagle’s medium (DMEM, Gibco) supplemented with 10% fetal bovine serum (FBS, Hyclone, Logan, UT), 100 IU mL−1 penicillin, and 100 μg mL−1 streptomycin (Pen/Strep) at 37 °C. Consequently, the epithelial cells were exposed to different concentrations (6.25, 12.5, 25, 50, 100 and 200 mg mL−1) of magnetic ZnFe2O4 nanoparticles. The cells cultured without nanoparticles were used as control. After incubation for 24 and 48 h, 20 mL of MTT solution (5 mg mL−1) was added to each well and incubated for further 4 h at 37 °C, the medium was discarded and the cells were lysed in 100 μL of DMSO. The absorbance of individual wells was measured at 570 nm by an ELISA reader (Huadong, DG-5031, Nanjing). The cell viability was determined as the percentage of absorbance values at each concentration compared to the control by the mean value of three independent experiments. Statistical significance was measured by one-way analysis of variance followed by Dunnett’s multiple comparison tests. Significance was ascribed at p < 0.05.
Antibacterial activity
The antibacterial activity of ZnFe2O4 NPs was evaluated by using disc diffusion assay against bacterial cultures of Gram-negative bacteria (Escherichia coli) and Gram-positive bacteria (Staphylococcus aureus). The qualitative assessment of the antibacterial effect was done using the Disk Diffusion test using the protocol of Jorgensen and Turnidge25. The bacteria were pre-grown on Nutrient agar (NA, Sigma-Aldrich, St. Louis, MO63103, USA) for 16 h at 37.0 ± 0.1 °C. The cultures were centrifuged and the bacteria were washed and suspended in distilled water, reaching a final concentration of 1 × 105–1 × 106 CFU mL−1 (2.5 × 105 CFU mL−1) (colony-forming units (CFU) per milliliter)) for Escherichia coli and Staphylococcus aureus. A concentration of 30 mg mL−1 of ZnFe2O4 NPs was prepared in sterile water and dispensed by sonication. Sterile filter paper discs (5.0-mm) were saturated by zinc ferrite solution and placed above the culture and incubated at 37 ± 0.1 °C for 24 h after which the zone of inhibition was employed to evaluate the antibacterial results. The sterile filter paper was saturated with sterile water and used as control.
Results
Characterization of magnetic nanoparticles
TEM images of NPs are presented in Fig. 3. Results showed that the ZnFe2O4 NPs had an average size of 10 nm. Diffraction reflections of the XRD patterns of the prepared NPs could be assigned to the (220), (311), (400), (331), (422), (531), and (440) planes of the face-centered cubic spinel structure of ZnFe2O4 which matches incredibly well with the JCPDS card no. 22–101230 as shown in Fig. 4A. According to Scherrer equation, the crystallite size of ZnFe2O4 is estimated 9.3 nm:
Magnetization curves of ZnFe2O4 which were obtained by VSM show the saturation magnetization of ZnFe2O4 NPs is around 26 emu g−1 (Fig. 4B). The hydrodynamic sizes of ZnFe2O4 NPs were determined by DLS method. DLS measurements of particles show ZnFe2O4 NPs mean hydrodynamic number size of 19 nm. (Fig. 4C) Moreover, the surface charge of the NPs was determined by zeta potential test showing that ZnFe2O4 NPs have a zeta potential of − 22.4 mV1.
In vitro tests
To study the process in more detail, NMT was done in the transparent tube alongside the artificial vessel, as shown in Fig. 5 (Fig. 5A shows the ablating the clot in a transparent polymer tube, Fig. 5B displays the schematic of abating zone and Fig. 5C shows the MRI image of ablating clot in graft). It is clear that the clot is abraded in the area where the magnet was rotating, while in other areas where there was no magnetic field, the abrasion process did not occur. Observations showed that the nanoparticles aggregated only at the magnet site and rotated with the magnet, thereby abrading the clot.
The feasibility of NMT for cleaning the vessel can be seen clearly. The size of fragments during the NMT process (the debris that is produced during the NMT process) were collected and estimated by DLS, as shown in Fig. 6. The data showed that the size of the fragments was in the nanoscale. The test results showed that the fragments were scattered over a nano-size range.
Figure 7 shows the relationship between clot removal rate and magnet rotational frequency. The clot removal rate increased about three-fold when the magnetic frequency was increased from 15 to 45 rpm. Moreover, to evaluate the possibility of vessel injury, the NMT process was performed for 12 h (the NPs were in contact with the surface of the vessel and the polymer tube). At the end of the process, no evidence was observed of a rupture to the polymer tube or artificial vessel, although the NMT process was performed for much longer than usual. To obtain a closer look, FESEM images of the surface of the vein and the polymer tube, respectively, were taken, as shown in Fig. 8 (different scale in Fig. 8A–D).
The arterial vessel surface can be contaminated by microbes through the blood, lymphatic spread, lymph node contact, or artery wall lesions20. Infection in the arteries is difficult to treat, as the infection may manifest many years after its implantation18. The antibacterial activity of the nano-magnetic zinc ferrite was tested employing two common bacterial pathogens: Escherichia coli (Gram- negative) and Staphylococcus aureus (Gram-positive) The results are summarized in Table 2. The results indicate that nano-magnetic zinc ferrite, which was employed in NMT, had antibacterial potential. It is clear from Table 2 while the artificial vessel does not have any antibacterial effect (the diameter of the inhabitation zone is zero), the diameter of the inhabitation zone in zinc ferrite (ZnFe2O4) nanoparticles varies from 11 to 19 mm and 11 to 16 mm for Escherichia coli and Staphylococcus aureus respectively.The results showed the antibacterial activity of zinc ferrite against E.coli and S. aureus bacterial pathogens, which can clear the surface of the vein. The release of Zn- and Fe-ions upon the decomposition of the ferrite in the experimental media could be responsible for these results29. The antibacterial effect of nano-magnetic zinc ferrite had the potential to decrease the risk of infection in artificial vessels.
To assess the effects of ZnFe2O4 NPs on epithelial cell line the MTT assay was carried out. The epithelial cells were treated with various concentrations of ZnFe2O4 NPs for 24 and 48 h. According to Fig. 9, there was a low toxicity effect on cells viability in the low dose of ZnFe2O4 NPs compared to the control sample. While the of ZnFe2O4 NPs show cytotoxicity at high concentrations after 48 h exposure. This property could be useful for using these NPs as drug carriers with minor side effects.
Discussion
As there is a great desire to employ artificial blood vessels in the treatment of vascular disease, finding a solution for declotting has challenged researchers3. Although the cleaning of artificial vessels via mechanical, chemical, and pharmacomechanical approaches have gained popularity, they have some inherent limitations that cannot be avoided. In catheter-directed thrombolysis (a chemical process), in which blood clots are dissolved by injecting medicine, an increased risk of bleeding restricts the administration of thrombolytic agents for declotting, especially cases of mural thrombi30. The time window for initiating therapy (between 3 and 4.5 h for tPa31) is one of the strictest limitations32.
Moreover, when a mechanical strategy is used, clots are eliminated by rotating devices. Directional thrombectomy has some demerits, such as distal embolization14, its complexity, and the risk of damaging vessels17. The rotation of abrasive tools at high speeds leads to an increase in heat due to friction or damage to the surface of the vessel14. The most important concern in this regard is related to the size of fragments, which affects the risk of occlusion in other small vessels and requires collection systems to cope with this challenge33. In addition, the tool heads are too large to penetrate small capillary vessels34.
Furthermore, the forces required to guide catheters into the artificial vessels against the flow of blood circulation can lead to side effects15. Most current approaches are not capable of cleaning the mural thrombi or biofilms attached to the vessel wall. Therefore, due to the unavoidable inherent limitations of current approaches, focusing on new approaches is likely more worthwhile than further developing previous ones.
The possibility of NMT
The NMT process described here is based on a new principle and strategy to overcome the inherent limitations of traditional approaches. Employing nano-sized tools makes it possible to clean mural thrombi in all vessels with different diameters. Meanwhile, the principle underlying NMT and its construction is relatively simple, which makes it easier to use than other methods.
The monitoring of the whole process in the transparent tube reveals the details of the process (Fig. 5A). After injecting the nano-magnetic particles into the fluid flow and reaching the clot site, it was observed that the nano-magnetic particles follow the movement of the rotating magnet inside the artificial vein. After that, the nanoparticles ablated the clot in the position of the rotation magnet. During the process, the external magnetic field propeled the nano-magnetic particles—which served as abrading tools—to special sites that eliminated the need for catheters (the external magnet plays the role of catheter). In addition, NMT could greatly improve fluid flow in artificial vessels. The increase in fluid flow approaching that of a normal artificial vessel confirmed that the clot had been abraded by nano-magnetic particles. However, NMT never stoped the fluid flow in the vessel, while in the traditional approach, bypassing the blockage artificial vessel is required until a surgeon fixes the artificial vessels34. Researchers have shown that magnetic nanoparticles can follow a moving magnetic field27. It has been demonstrated that using a method for transporting the magnetic nanoparticles inside a microfluidic channel, where a rotating permanent magnet is employed to induces the rotation of magnetic field on magnetic nanoparticles, leads to the movement of MNP along the surface of a microfluidic channel35. Magnetic nanoparticle clusters carrying drugs can be rotated across physiologic surfaces in response to a rotating magnet to augment the drug delivery in a special site36. While, the researchers used the movement of nanoparticles to improve drug release in dissolving clots, in this study, the motion of nanoparticles under a rotating magnetic field was used to abrasive the clot.Nano-scale abrasive tools make it possible for particles to penetrate very small vessels to abrade clots. One of the main challenges of traditional thrombectomy is the size of the device head, which limits penetration into vessels37. Meanwhile, because the particle size affects the immune system, NPs should be smaller than 100 nm so that they can exit the immune system38.
Mathematical model of NMT
It is observed from the initial in vitro tests that several parameters govern the NMT process and that significant output factors depend on them. Therefore, the theoretical study of NMT is vital to understand the mechanisms and physics behind the process. In addition, mathematical modeling would be valuable for evaluating and predicting the effects of individual parameters on the outputs of the process. The below relationship state:
Due to the physics of the process, the magnetic and mechanical equations are employed to describe the process.
In the above relation, MR the clot removal rate, h is the size of fragments, \(\omega \) the frequency of magnet rotation, d the diameter of magnetic abrasive particle, N the number of magnetic abrasive particles effective in cutting operations, t time of process, \(\sigma \) the compression strength of clot, B the magnetic field density.
Magnetic model
Classical Maxwell's equations descript the electromagnetism of modeling39 as follow:
where E: electric field vector, B: magnetic flux density vector, H: magnetic flux intensity vector, J: electric current, density, D: electric flux density vector, and t: time.
Expression for force on a magnetic dipole moment in a magnetic field describes by Lorentz force equation28 as below:
From here, assuming that the moment of the magnetic particle is co-linear with the applied field. This is a reasonable assumption given the small size and high susceptibility of the magnetic particles.
Where F is the magnetic force due to magnetic field B and J is the current density.
The magnetic force Fz can be calculated from the equation39:
The magnetic pressure and magnetic tension can be written as follows28. V is the volume of the particle, M is the magnetization of the particles. The magnetic force can be calculated as below:
where: A is the area of each surface, in m2; μ0 is the permeability of space, which equals 4π × 10−7 T·m A−1; B0 is the flux density, in T.
Modeling of cutting forces
To cutting the surface of plaque by magnetic abrasive particles, two prerequisites must be given, one is the penetrating force (normal force) (\({F}_{V}\)), the other is relative to the moving velocity between abrasive particles and plaque surface that acts as a shearing force (horizontal force) (\({F}_{H}\)). It is concluded that these two force components are the primary forces governing the process fluid. However, other force components, such as the capillary viscous force due to the presence of blood, the gravitational force are assumed to be negligible compared the other ones. A schematic representation of forces acting in the abrading process is shown in Fig. 1C.
The vertical force leads to a compressive stress defined as below:
where \({\mathrm{A}}_{\mathrm{R}1}\) is the contact area of the magnetic micro/nanoparticles with the target surface, as shown in Fig. 3, the contact area is:
The height of a nano-particle penetrates on the plaque surface is defined by :
The volume is cut by one nanoparticle is equal to the amount of penetration nano particles on the plaque surface as below:
The length of the path that the particle travels over the circle depends on the size of its movement on the array-diameter of the vessel-and the size of the nanoparticle as below:
The total removal volume is equal to the volume removed by a particle in the total number of particles effective in cutting operations:
Therefore, the time required to remove the clot is calculated from the following formula:
In summary, the proposed mathematical modeling describes the relationship between significant process parameters including the magnetic field (B), the size of the nanoparticles (R) and the mechanical properties of clot (\(\sigma )\) which influence the process.The relationship between the applied force on a nanoparticle and the magnetic field strength and particle size is shown in Fig. 10A. It is clear from Fig. 10A that the magnitude of the applied force increases with increasing nanoparticle size and magnetic field strength. Meanwhile, the relationship between the removal volume of the clot by a single nanoparticle and the magnetic field strength is shown in Fig. 10B. It is also clear from Fig. 10B that there is a direct relationship between the removal volume and the intensity of the clot and magnetic field strength and the size of the nanoparticles.
(A) The relationship between the applied force on a nanoparticle and the magnetic field strength and particle size. (B) The relationship between the removal volume of the clot by a single nanoparticle and the magnetic field strength. (C) The relationship between the size of fragments and the magnetic field strength and particle size.
Fragment size
Distal embolization is one of the main side effects and great challenges of mechanical thrombectomy14,17. Rotating the abrasive tools at higher speeds produces debris, which increases the risk of occlusion in small vessels; thus, collection systems are required to cope with these challenges33. Fragments should be small enough to prevent blockages in the smallest veins (which are 6–8 μm in diameter; the cells and platelets that can move through the smallest veins are 4 microns in size38). It is clear from Fig. 6 that the average fragments are nano-sized. The fragments are small enough (less than 1 micron) to prevent blockage in the smallest veins. Therefore, the fragments produced during the NMT process will pass through the capillary system and will be taken up by the reticuloendothelial system. Furthermore, the mathematical model states that the fragment size depends on the vertical force (\(\mathrm{Fn}\)) and compression stress (\(\upsigma )\), or, in other words, on the size of the magnetic nanoparticles (\(\mathrm{R}\)) and the applied magnetic field (B) as shown in Fig. 10C. As the fragment size is one of the main criteria in thrombectomy, other NMT parameters should be selected in such a way that large fragments are avoided.
The effect of magnetic rotational frequency
Figure 7 shows that declotting in artificial vessels increases by raising the rotational frequency. The rate of clot removal depends on the relative motion between the magnetic abrasive particles and the surface layers of the mural clot. The increase in rotational frequency might cause an increase in tangential cutting force; hence, the peaks of clot layers are sheared faster, thus causing clot removal rate to increase. At the same time, the number of cutting edges per unit of time increases when the rotational frequency is increased. When particles travel at a high speed, the tangential force is great, and the chances of the abrasive particles indenting the clot surface and breaking down the micron hills of clot surface increase. But the increased rotational frequency causes the nanoparticles to fail to follow the magnetic field35, resulting in a slipping or lessening process.
Study of the probability of artificial vessel damage
Damage to vessels is one of the challenges of traditional atherectomy17. Vessel injury or burning has been reported due to the fraction between the head of the device used and the vessel wall during high-speed rotation14. An evaluation of the surface of artificial vessels by FESEM images show that if nano-magnetic particles contact the walls of vessels instead of the clot for 4 h, the rate of penetrating particles on the target surface (on the vessel wall) is at the nano-scale, as shown in Fig. 8 (different scale in Fig. 8A–D). In addition, no evidence of rupturing was observed in the artificial vessels.
The fate of nanoparticles
The fate of nanoparticles is crucial to what will eventually happen to them or how they will exit the body. Interestingly, studies confirm that nano magnetic particles undergo metabolism equally in hepatocytes and macrophages40. Researchers have shown that Fe3O4 nanoparticles are primarily cleared from the blood by the reticuloendothelial system41 or lymph nodes40. Intracellular metabolism plays a significant role in the elimination of nano-magnetic particles by the Kupffer cells in the liver, which are the primary site of iron metabolism40. However, some parameters, such as dose injected, percent initially taken up, and the cellular distribution in the liver, are affected by the rate of iron oxide metabolism in the liver40. The half-lives of different iron oxide nanoparticles in the blood for clinical use are between 1 h and 24–36 h41. However, some particle properties, such as size, morphology and surface characteristics affect the clearance process42. Interestingly, core–shell nano-magnetic particles exhibit different clearance mechanisms43. Evidence confirms that nanoparticles smaller than 100 nm can be cleared from the body. Finally, as the size of nano-magnetic particles is between the 10 to 100 nm diameter in NMT, their fate (both are nano-scales) is likely clearance by the liver, kidney, and lungs. Alternatively, it is possible to design a magnetic needle that can remove magnetic nanoparticles. In the future, animal tests will be performed to determine the fate of nanoparticles in details.
The approach presented in this paper demonstrates the possibility of cleaning the inside of an artificial vessel from outside of the body without damaging the vessel and without producing dangerous fragments. The conceptual principles explained in this study could be used in other vascular depositions, such as the accumulation of lipids, white blood cells, fibrosis, calcification, and other materials in the internal layer of arterial walls; mural thrombi in deep vein thrombosis; and atherosclerosis. The proposed technique, when compared with other atherectomy approaches, faces fewer challenges to translate this technique into in vivo. In conventional atherectomy devices, the presence of a catheter, as well as the head of the tool, creates many constraints. NMT makes it possible to eliminate the need for a catheter, thus simplifying the process and making it non-invasive. The present data suggest that NMT may have several practical and conceptual advantages over current commercially available thrombectomy systems.
Future work
Since our approach is concept-based, it can be applied not only to artificial blood vessels, but also to any kind of atherosclerosis, mural thrombi, calcification in vein, and other situations. Therefore, more research will be done in the future to make our approach suitable for the in vivo testing of different vascular depositions. In the future, the drug-carrying nanoparticles will be examined to enhance the efficiency of declotting by combining different chemical and mechanical mechanisms.
Conclusion
The technique presented in this study provides a novel form of therapy to eliminate clots in artificial vessels by abrading the clot surface under a rotary magnetic field. The results are summarized below:
-
(1)
In vitro tests confirm the feasibility of nano-magnetic thrombectomy in artificial vessels and show that NMT is a promising approach for removing clots from artificial vessels.
-
(2)
A mathematical model is developed to demonstrate the relationships between the various process parameters. There is a direct relationship between nanoparticle size, magnetic field, and the rate of declotting in artificial vessels. Meanwhile, according to the mathematical model, increasing the magnetic field leads to an increase in the size of fragments.
-
(3)
The results show that the fragments are nano-sized, which greatly reduces the risk of distal embolization, which is a significant concern in traditional atherectomy approaches. The mathematical model also predicted the nanosize of fragments.
-
(4)
Visual observations, as well as FESEM images, showed no evidence of vein damage, even when the process times were long.
-
(5)
As the diameters of nano-magnetic particles are between 10 to 100 nm in NMT, their fate is likely clearance by the liver, kidney, and lungs. Meanwhile, the antibacterial effect of nano-magnetic zinc ferrite has the potential to decrease the risk of infection in artificial vessels.
Ethical approval
All methods were carried out in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study was approved by the Nursing Committee for Biological Ethics and Biomedical Research at the Islamic Azad University of Shirvan on November 7, 2019, No. T1179315. The author gives his consent for publishing all subjects of the paper. All participants give their consent for publishing all subjects of the paper.
Change history
17 August 2022
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1038/s41598-022-18312-7
References
Chlupáč, J., Filova, E. & Bačáková, L. Blood vessel replacement: 50 years of development and tissue engineering paradigms in vascular surgery. Physiol. Res. 58(Suppl 2), S119–S139 (2009).
Prodromos, C. The Anterior Cruciate Ligament: Reconstruction and Basic Science E-Book: Reconstruction and Basic Science (Elsevier Health Sciences, Amsterdam, 2017).
Zada, G. et al. Internal carotid artery aneurysms occurring at the origin of fetal variant posterior cerebral arteries: Surgical and endovascular experience. Oper. Neurosurg. 63(suppl1), 55–62 (2008).
Wallace, M. J. et al. Use of inferior vena caval filters and survival in patients with malignancy. Cancer 101(8), 1902–1907 (2004).
Pocivavsek, L. et al. Active wrinkles to drive self-cleaning: A strategy for anti-thrombotic surfaces for vascular grafts. Biomaterials 192, 226–234 (2019).
De Visscher, G. et al. Improved endothelialization and reduced thrombosis by coating a synthetic vascular graft with fibronectin and stem cell homing factor SDF-1α. Acta Biomater. 8(3), 1330–1338 (2012).
Quencer, K. B. & Oklu, R. Hemodialysis access thrombosis. Cardiovasc. Diagn. Ther. 7(Suppl 3), S299 (2017).
Gao, Y. Fabrication and In Vitro Testing of Synthetic Arterial Grafts (University of Pittsburgh, Pittsburgh, 2017).
Vad, S. et al. Determination of coefficient of friction for self-expanding stent-grafts. J. Biomech. Eng. 132(12), 121007 (2010).
Shulze, J.E., R.E. Betts, and D.R. Savage, Drug-delivery endovascular stent and method for treating restenosis. 2010, Google Patents.
Roberts, A. C. et al. Pulse-spray pharmacomechanical thrombolysis for treatment of thrombosed dialysis access grafts. Am. J. Surg. 166(2), 221–226 (1993).
Cynamon, J. et al. Hemodialysis graft declotting: description of the “lyse and wait” technique. J. Vasc. Interv. Radiol. 8(5), 825–829 (1997).
Powers, W. J. et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 46(10), 3020–3035 (2015).
Akkus, N. I. et al. Atherectomy devices: technology update. Med. Devices (Auckland, NZ) 8, 1 (2015).
Ribo, M. et al. Difficult catheter access to the occluded vessel during endovascular treatment of acute ischemic stroke is associated with worse clinical outcome. J. Neurointerv. Surg. 5(suppl 1), i70–i73 (2013).
Miloro, P. et al. Removing vascular obstructions: A challenge, yet an opportunity for interventional microdevices. Biomed. Microdevice 14(3), 511–532 (2012).
Saraf, H. et al. Mechanical properties of soft human tissues under dynamic loading. J. Biomech. 40(9), 1960–1967 (2007).
Vicaretti, M. 29. Pathophysiology of Vascular Graft Infections 537 (University of Adelaide Press, Adelaide, 2011).
Hasse, B. et al. Vascular graft infections. Swiss Med. Wkly. 143, w13754 (2013).
Stone, P. A. et al. Antibiotic-loaded polymethylmethacrylate beads for the treatment of extracavitary vascular surgical site infections. J. Vasc. Surg. 55(6), 1706–1711 (2012).
Zhang, Y.-G. et al. Diagnosis and treatment of vascular surgery related infection. Open Biomed. Eng. J. 9, 250 (2015).
Glover, S. & Brun-Buisson, C. Infections associated with intravascular lines, grafts and devices. In Infectious Diseases 492–503 (Elsevier, 2010).
Dincă, V. et al. Biocompatible pure ZnO nanoparticles-3D bacterial cellulose biointerfaces with antibacterial properties. Arab. J. Chem. 13(1), 3521–3533 (2020).
Willis, A. J. et al. Rotating magnetic nanoparticle clusters as microdevices for drug delivery. Int. J. Nanomed. 15, 4105–4123 (2020).
Meng, Q. et al. Intranasal delivery of Huperzine A to the brain using lactoferrin-conjugated N-trimethylated chitosan surface-modified PLGA nanoparticles for treatment of Alzheimer’s disease. Int. J. Nanomed. 13, 705 (2018).
Tran, N. & Webster, T. J. Magnetic nanoparticles: Biomedical applications and challenges. J. Mater. Chem. 20(40), 8760–8767 (2010).
Karle, M. et al. Controlled counter-flow motion of magnetic bead chains rolling along microchannels. Microfluid. Nanofluid. 10(4), 935–939 (2011).
Vinosha, P. A. et al. Synthesis and properties of spinel ZnFe2O4 nanoparticles by facile co-precipitation route. Optik 134, 99–108 (2017).
Raveendra, R. et al. Synthesis, characterization and antibacterial activity of zinc ferrite nanopowder. Int. J. Sci. Res. 1(4), 543–547 (2013).
Friedrich, R. P. et al. Tissue plasminogen activator binding to superparamagnetic iron oxide nanoparticle—covalent versus adsorptive approach. Nanoscale Res. Lett. 11(1), 1–11 (2016).
Ouriel, K. et al. Comparison of streptokinase, urokinase, and recombinant tissue plasminogen activator in an in vitro model of venous thrombolysis. J. Vasc. Surg. 22(5), 593–597 (1995).
Mullen, M. T. et al. Systematic review of outcome after ischemic stroke due to anterior circulation occlusion treated with intravenous, intra-arterial, or combined intravenous+ intra-arterial thrombolysis. Stroke 43(9), 2350–2355 (2012).
Ho, P. C., Weatherby, T. M. & Dunlap, M. Burr erosion in rotational ablation of metallic coronary stent: An electron microscopic study. J. Interv. Cardiol. 23(3), 233–239 (2010).
Clarençon, F. et al. Thrombectomy for acute basilar artery occlusion by using double Merci retriever devices and bilateral temporary vertebral artery flow reversal. J. Neurosurg. 111(1), 53–56 (2009).
Engelhard, H. H. et al. A novel tissue culture tray for the study of magnetically induced rotation and translation of iron oxide nanoparticles. IEEE Magn. Lett. 8, 1–5 (2017).
Pernal, S. P. et al. An in vitro model system for evaluating remote magnetic nanoparticle movement and fibrinolysis. Int. J. Nanomed. 15, 1549 (2020).
van Leeuwen, T. G. et al. Intraluminal vapor bubble induced by excimer laser pulse causes microsecond arterial dilation and invagination leading to extensive wall damage in the rabbit. Circulation 87(4), 1258–1263 (1993).
Vinay, K., Abbas Abul, K. & Nelson, F. Mitchell Richard N. Robbins Basic Pathology 8th edn, 348–351 (Saunders Elsevier, Amsterdam, 2007).
Al-Dulaimi, T. & Khamesee, M. B. A stationary apparatus of magnetic abrasive finishing using a rotating magnetic field. Microsyst. Technol. 23(11), 5185–5191 (2017).
Jain, T. K. et al. Biodistribution, clearance, and biocompatibility of iron oxide magnetic nanoparticles in rats. Mol. Pharm. 5(2), 316–327 (2008).
Corot, C. et al. Recent advances in iron oxide nanocrystal technology for medical imaging. Adv. Drug Deliv. Rev. 58(14), 1471–1504 (2006).
Chouly, C. et al. Development of superparamagnetic nanoparticles for MRI: Effect of particle size, charge and surface nature on biodistribution. J. Microencapsul. 13(3), 245–255 (1996).
Bourrinet, P. et al. Preclinical safety and pharmacokinetic profile of ferumoxtran-10, an ultrasmall superparamagnetic iron oxide magnetic resonance contrast agent. Invest. Radiol. 41(3), 313–324 (2006).
Author information
Authors and Affiliations
Contributions
A.M. conceived the original idea and carried out the experiment. J.V. contributed to the final version of the manuscript and some tips on cytotoxicity testing. F.A. supervised the project and contributed to the final version of the manuscript. M.K. involved in planning and supervised the work and some tips on cytotoxicity testing. A.F. developed the original idea and theory. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1038/s41598-022-18312-7
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moghanizadeh, A., Ashrafizadeh, F., Varshosaz, J. et al. RETRACTED ARTICLE: Noninvasive thrombectomy of graft by nano-magnetic ablating particles. Sci Rep 11, 7004 (2021). https://doi.org/10.1038/s41598-021-86291-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-86291-2
This article is cited by
-
Retraction Note: Study the effect of static magnetic field intensity on drug delivery by magnetic nanoparticles
Scientific Reports (2022)
-
Locomotion and disaggregation control of paramagnetic nanoclusters using wireless electromagnetic fields for enhanced targeted drug delivery
Scientific Reports (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.