Abstract
In this study, the hands and feet of 15,384 undergraduate and postgraduate students in 3 colleges in Beijing were examined for the presence of cutaneous warts at college-entry, and those diagnosed with warts were followed up 2–3 years later. We identified totally 215 (1.4%; 95% CI, 1.2–1.6%) students with warts. The prevalence was significantly higher in male than in female students (2.0% vs. 0.9%, P < 0.0001). Of the 215 patients, 66.9% and 62.1% had only one wart and 98.3% and 93.2% had warts <1 cm in diameter, on the hands and feet, respectively. Of the 130 patients with a follow-up visit, 78 did not receive any treatment (44 recovered within 2 years). Patients aged 21–25 compared to those aged ≤20 were more likely to be free of warts (hazard ratio = 1.76; 95% CI, 1.07–2.89), while lower father’s education (hazard ratio = 0.19; 95% CI, 0.04–0.98) and poor sleep quality (hazard ratio = 0.41; 95% CI, 0.18–0.92) decreased the likelihood of resolution. The prevalence of warts is 1.4% in college students. The majority of patients have warts <1 cm and approximately 2/3 patients has one wart. Slightly over half of patients recover spontaneously within 2 years. Patients’ age, sleep quality, and paternal education may affect the resolution.
Similar content being viewed by others
Introduction
Cutaneous warts are caused by the human papilloma virus (HPV), the most prevalent types of which are HPV2/27/57 and HPV11,2,3,4,5,6,7. While most patients with cutaneous warts are asymptomatic, some may experience physical or psychological discomfort8. Many studies have documented the prevalence of cutaneous warts in children9,10,11,12,13, ranging widely from 3.3% in the USA to 33% in the Netherlands11,13. Data on the prevalence of cutaneous warts in young adults are limited compared with those in children. In an earlier UK study with a modest sample size, the prevalence was reported to be 3.5% in people aged 25 to 34 years and 0.3% in those aged 35 to 54 years14. In another earlier US study with a relatively large sample size, the prevalence of wart was 1.2% in people aged 18 to 24 years and 0.6% in those aged 25 to 3415. Neither of these reports provided data on the determinants and clinical profile of warts in adults14,15.
Cutaneous warts may resolve spontaneously. Bruggink et al. found that one-half of primary schoolchildren with warts would be free of warts within one year, and young age and non-Caucasian skin type were protective factors for wart resolution16. In comparison to children, the natural course and prognostic factors of warts in adults are scarce, although these information may be of particular importance in shared decision-making with patients.
In this study, we aimed to determine the prevalence, clinical profile, and prognosis of cutaneous warts in Chinese college students, a typical young adult population. We also aimed to identify potential factors influencing the occurrence and resolution of warts.
Results
Prevalence of Cutaneous Warts
Of the 15,384 students, 215 were diagnosed with cutaneous warts, with an overall prevalence of 1.4% (95% CI, 1.2–1.6%). The prevalence was significantly higher in male than in female students (2.0% vs. 0.9%, P < 0.0001) and in students from rural than those from urban areas (1.7% vs. 1.3%, P = 0.03). The prevalence tended to be negatively associated with maternal and paternal education levels (p for trend test = 0.070 and 0.014, respectively). No statistical difference was observed in the prevalence of cutaneous warts between groups defined by participants’ age, ethnicity, region, or parents’ occupation. In the multivariate logistic regression analysis, male gender was associated with an increased risk of warts (aOR = 2.06; 95% CI, 1.55–2.74) (Table 1). Further analyses performed separately for subtypes of cutaneous warts showed that male gender was associated with an increased risk of both common (aOR = 2.38; 95% CI, 1.60–3.55) and plantar warts (aOR = 2.04; 95% CI, 1.32–3.14).
Clinical Characteristics of Warts
Of the 215 patients diagnosed with cutaneous warts, 52.1% had common warts; 40.5%, plantar warts; 5.1%, plane warts; 1.7%, plantar as well as common warts; and 0.5%, plane as well as common warts (Table 2). Of the 212 patients with records on location of warts, 10.4% had wart(s) on the dorsum of the left hand; 19.3%, on the dorsum of the right hand; 14.2%, on the sole of the left foot; 17.0%, on the sole of the right foot; 10.4%, on any two of the aforementioned locations; 28.8%, on other non-common locations (Table 2). Of the 126 patients with warts on the hands, 66.9% had a single wart, and 98.3% had warts <1 cm in diameter; the corresponding percentages were 62.1% and 93.2%, for the 103 patients with warts on the feet, respectively (Table 2). Forty-nine patients (22.8%) had visited a doctor.
Of the 215 patients, 71 (33.0%) reported one or more suspected predisposing factors of warts, including friction (42 patients, 19.5%), trauma (23 patients, 10.7%), direct skin-to-skin contact (2 patients, 0.9%), and any two of the aforementioned factors (4 patients, 1.9%) (Table 2). Of the 215 patients, 29 (13.5%) reported to have suffered from discomfort caused by the warts, including worrying of infection (5.6%), affecting walking, sports and work (4.7%), unsightly appearance (1.9%), and any two of the aforementioned discomfort (1.4%) (Table 2). Thirty-four patients (15.8%) reported to have had clinical symptoms, including itching (3.7%), pain during activity (11.2%), spontaneous pain (0.5%), and both pain during activity and spontaneous pain (0.5%) (Table 2). The self-reported scores on pain intensity during activity, as assessed by a 0 (no pain) to 10 (worst pain imaginable) point numeric rating scale, ranged from 1 to 5 points (mean ± SD, 3.1 ± 1.5).
Follow-up Results
In total, 130 (60.5%) of the 215 patients received a follow-up survey: 95 were re-examined by a trained dermatologist on site, and 35 were interviewed via telephone. Of the 85 patients who were lost to follow-up, 60 patients could not be contacted and 25 refused to participate. All demographic and clinical characteristics, except father’s education level, did not differ between patients who participated in the follow-up survey and those who did not (Table 3).
Of the 130 patients, 78 did not receive any treatment, of whom 24 (30.8%) recovered spontaneously within 1 year, 20 (25.6%) between 1 and 2 years, and 10 (12.8%) beyond 2 years. Of the 52 who had received treatments, 26 (50.0%) were treated with cryotherapy, 7 (13.5%) with CO2 laser, 2 (3.8%) with both cryotherapy and1064-nm long-pulsed Nd: YAG laser, 5 (9.6%) with plasters containing 78% salicylic acid and 4% phenol, 3 (5.8%) with traditional Chinese medicine, 1 (1.9%) with interferon-α gel, 1 (1.9%) with retinoids cream, and 7 (13.5%) with unclear treatments.
Factors Influencing Resolution of Warts
In the multivariate analyses, the middle age group (aged 21 to 25 years vs. ≤20 years) was a protective factor for the resolution of warts, whereas lower father’s education level and poor sleep quality were risk factors for the resolution (Table 4).
Discussion
In this study, we found that 1.4% of college students were affected with warts on their hands and/or feet. The majority of patients had only one wart on the hand or foot and the majority of warts were <1 cm in diameter. Slightly over half of patients experienced spontaneous resolution of warts within two years after the initial survey. Patients’ age, sleep quality, and paternal education level were shown to be independently associated with the resolution of warts.
In comparison to the studies that had involved young adults from the UK and the USA14,15, the overall prevalence rate of cutaneous warts in our study was lower than that in the UK study, while being similar to the US study15. In our survey, the prevalence of cutaneous warts varied slightly across different age groups: 1.4%, 1.3%, and 1.6% in those aged 14 to 20, 21 to 25, and 26 to 35 years, respectively. By contrast, the prevalence of warts in children and adolescents varied considerably from 0.3% to 8.6% in individuals aged 1 to 17 years, with peak prevalence occurring at 9 to 10 years13. The reasons for the different magnitudes of variation in cutaneous wart prevalence between children and college students remain largely unknown, which may possibly be attributed to age-related differences in physical activity and sports participation, the resistance of the stratum corneum, and host immunity.
The UK study documented no significant gender differences in prevalence of warts in adults14, but the US study showed that the warts were more frequent in male than female adults15. Consistent with the US study, the prevalence of warts was significantly higher in males in our study. After adjustments for various demographical and clinical factors, gender-specific differences remained statistically significant, suggesting that male gender might be an independent risk factor of cutaneous warts in our population. This may be attributed to males being physically more active compared to females17 and therefore at a higher risk of damage to the stratum corneum that serves as an entry point of HPV18. In this study, we also found that the prevalence of warts was negatively associated with fathers’ education. This may be partially due to that students whose fathers have a lower education level were more likely to come from families with relatively lower socioeconomic status, which has been reported to be a risk factor for the warts9,14. Notably, we could not exclude the possibility that the association of male gender and father’s education with the warts was an incidental finding, because we have made multiple sets of statistical comparisons regarding the differences of prevalence of warts among subgroups of students.
To the best of our knowledge, this is the first study to document the clinical characteristics of cutaneous warts in college students. We found that the percentage of patients with multiple warts (36%) or with warts ≥1 cm in diameter (4%) was substantially lower than that in children (43% and 37%, respectively)16. We also found that pain was the most commonly reported inconvenience (12%) in our patients, while in pediatric patients the percentage of pain was much lower (8%)16. Unsightly appearance, as the most commonly reported inconvenience (14%) in pediatric patients16, was only reported by 2% of our patients. Despite the aforementioned differences in clinical characteristics, the percentage of our patients who had sought treatment prior to the survey was comparable to that of pediatric patients (23% vs. 24%10).
The spontaneous resolution rate of warts within 1 and 2 years was reported to be 50% and 67% in children, respectively16,19. By contrast, less than one-third and slightly over half of our patients recovered spontaneously within 1 and 2 years after the initial survey, respectively, suggesting a lower likelihood of spontaneous resolution of warts in young adults compared to children. It has been reported that age and ethnicity may play a role in the resolution of warts in children16. The current study shows that age, sleep quality, and father’s education level may influence the resolution of wart in young adults; speculatively, this may be attributed to individual factors (such as immunity) and family socioeconomic status. In addition, we found that the type and number of warts did not seem to influence the outcome in young adults, which is in agreement with the findings in children16.
The present study has several strengths. First, to our knowledge, this is the first study focusing on epidemiological and clinical characteristics of cutaneous warts in college students. Second, the participation rate was high given that the survey was conducted along with the college-entry health examinations. Third, all participants were examined one by one for the presence of warts by trained dermatologists according to uniform diagnostic criteria. Fourth, we identified that several factors including patients’ age, sleep quality and father’s education level were independently associated with the resolution of warts, which provides new insights into the consultation and treatment concerning cutaneous warts. This study also has limitations. First, we only examined the hands and feet. However, this was less likely to result in significant underestimation of the overall prevalence of warts, as cutaneous warts on other parts of the body accounted for <4% of all warts20. Second, the patients were only followed up once, 2–3 years after the initial survey, and some participants could only provide an estimated time of resolution. Third, we did not collect information about hygienic practice and grooming of skin, which may influence the occurrence of the warts. Finally, our survey was only conducted in 3 colleges in Beijing, which may therefore limit the generalization of the findings.
In summary, this study provides an updated estimate of the prevalence of cutaneous warts as well as new insights into the clinical and prognostic profiles of cutaneous warts in college students, likely benefiting to the medical consultation and treatment concerning cutaneous warts in young adults.
Methods
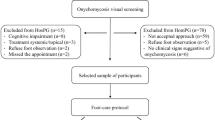
Study Design and Participants
This study was a cross-sectional survey among the first-year undergraduate and postgraduate students (September 2012, March 2013, and September 2013) of three colleges in Beijing, and those diagnosed with warts were followed up between December 2015 and March 2016. This study protocol was approved by the Institutional Review Board of 306 Hospital of PLA, and all methods were performed in accordance with relevant guidelines/regulations; oral informed consent was obtained from all the participants before the survey.
Procedure and Wart Examination
Along with the college-entry health examinations, the students were invited to complete a questionnaire containing questions about demographic information including age, sex, ethnicity, residential region, parents’ occupation, and education level. Then, the hands and feet of the students were examined one by one, following uniform diagnostic criteria, by dermatologists who were trained specifically prior to the start of the study. If a student was diagnosed with wart(s), the dermatologists collected detailed information via a face-to-face interview about the clinical characteristics of warts and potential influencing factors. The clinical characteristics included type, location, number, size, and duration of warts, duration from wart onset to seeing a doctor, suspected predisposing factors of warts, discomfort caused by warts, symptoms. The potential influencing factors of warts included smoking (yes or no), drinking (yes or no), regular exercise (yes or no), poor sleep quality (yes or no), and high psychological stress (yes or no). Smoking was defined as at least one cigarette per day. Dinking was defined as intake of at least 50 ml of Chinese liquor, 250 ml of wine, or 500 ml of beer per week. Regular exercise, sleep quality and psychological stress were self-reported by students based on their own perception. Two-three years later, a trained dermatologist revisited the patients on site to conduct a follow-up interview. In case the patients could not be reached on site, a telephone interview was conducted. During the follow-up interview, information on resolution of warts and types of topical treatment received between the initial survey and the follow-up visit was collected. Complete resolution was defined as no warts being visible and not palpated by hand. With regards to the types of treatments, the dermatologists responsible for the follow-up interview chose among the following: cryotherapy, CO2 laser, photodynamic therapy, pulsed dye laser, plasters containing 78% salicylic acid and 4% phenol, traditional Chinese medicine, interferon-α, retinoids, antitumor drugs and other treatments.
Statistical Analyses
The chi-squared test was used to examine the statistical differences in the prevalence of warts between subgroups defined by demographic characteristics. Multivariate logistic regression analyses were performed to determine which factors might be independently associated with warts, through which the adjusted odds ratio (aOR) with 95% CI was calculated. Univariate and multivariate Cox proportional hazards models were used to estimate the hazard ratios for the resolution of warts. We used a complete case strategy in the multivariate analyses given that missing data on covariates was much lower (<5%). Statistical analyses were performed with IBM SPSS version 20.0. All statistical tests were two-sided using a significance level of alpha = 0.05.
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Chen, S. L., Tsao, Y. P., Lee, J. W., Sheu, W. C. & Liu, Y. T. Characterization and analysis of human papillomaviruses of skin warts. Arch Dermatol Res 285, 460–465 (1993).
Rubben, A., Kalka, K., Spelten, B. & Grussendorf-Conen, E. I. Clinical features and age distribution of patients with HPV 2/27/57-induced common warts. Arch Dermatol Res 289, 337–340 (1997).
Iftner, A. et al. The prevalence of human papillomavirus genotypes in nonmelanoma skin cancers of nonimmunosuppressed individuals identifies high-risk genital types as possible risk factors. Cancer Res 63, 7515–7519 (2003).
Porro, A. M. et al. Detection and typing of human papillomavirus in cutaneous warts of patients infected with human immunodeficiency virus type 1. Br J Dermatol 149, 1192–1199 (2003).
Hagiwara, K. et al. A genotype distribution of human papillomaviruses detected by polymerase chain reaction and direct sequencing analysis in a large sample of common warts in Japan. J Med Virol 77, 107–112 (2005).
Tomson, N. et al. Human papillomavirus typing of warts and response to cryotherapy. J Eur Acad Dermatol Venereol 25, 1108–1111 (2011).
Bruggink, S. C. et al. Cutaneous wart-associated HPV types: prevalence and relation with patient characteristics. J Clin Virol 55, 250–255 (2012).
Androphy, E. J. & Lowy, D. R. Warts in Fitzpatrick’s Dermatology in General Medicine (7th ed. Wolff, K. et al.) 1914–1923 (McGraw-Hill, 2008).
Williams, H. C., Pottier, A. & Strachan, D. The descriptive epidemiology of warts in British schoolchildren. Br J Dermatol 128, 504–511 (1993).
Kilkenny, M., Merlin, K., Young, R. & Marks, R. The prevalence of common skin conditions in Australian school students: 1. Common, plane and plantar viral warts. Br J Dermatol 138, 840–845 (1998).
van Haalen, F. M., Bruggink, S. C., Gussekloo, J., Assendelft, W. J. & Eekhof, J. A. Warts in primary schoolchildren: prevalence and relation with environmental factors. Br J Dermatol 161, 148–152 (2009).
Yamamah, G. A. et al. Epidemiologic study of dermatologic disorders among children in South Sinai, Egypt. Int J Dermatol 51, 1180–1185 (2012).
Silverberg, J. I. & Silverberg, N. B. The U.S. prevalence of common warts in childhood: a population-based study. J Invest Dermatol 133, 2788–2790 (2013).
Rea, J. N., Newhouse, M. L. & Halil, T. Skin disease in Lambeth. A community study of prevalence and use of medical care. Br J Prev Soc Med 30, 107–114 (1976).
Johnson, M. T. & Roberts, J. Skin conditions and related need for medical care among persons 1–74 years. UnitedStates, 1971–1974. Vital Health Stat 11 i–v, 1–72 (1978).
Bruggink, S. C. et al. Natural course of cutaneous warts among primary schoolchildren: a prospective cohort study. Ann Fam Med 11, 437–441 (2013).
Lu, C. et al. Factors of physical activity among Chinese children and adolescents: a systematic review. Int J Behav Nutr Phys Act 14, 36 (2017).
Smotkin, D. Virology of human papillomavirus. Clin Obstet Gynecol 32, 117–126 (1989).
Massing, A. M. & Epstein, W. L. Natural history of warts. A two-year study. Arch Dermatol 87, 306–310 (1963).
Larsson, P. A. & Liden, S. Prevalence of skin diseases among adolescents 12–16 years of age. Acta Derm Venereol 60, 415–423 (1980).
Acknowledgements
This is a joint effort by many dermatologists and staff members, whose contributions are gratefully acknowledged. We especially thank the participants in this study, as well as the teachers who provided support for the organization and implementation of this study.
Author information
Authors and Affiliations
Contributions
Jianjun Liu, Hongtian Li and Shichao Lu were responsible for the conception and design of the study. Jianjun Liu, Hongtian Li, Fan Yang, Yingyun Ren, Tianbao Xia, Zigang Zhao, Xiaojia Cao, Ze-kun Wang, Mengmeng Yin and Shichao Lu were responsible for acquisition of data. Jianjun Liu, Hongtian Li and Shichao Lu performed the data analysis and drafed the manuscript. All authors participated in interpretation of the findings and all authors read and approved the final version of the manuscript. All authors confirm that the content has not been published elsewhere and does not overlap with or duplicate their published work.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, J., Li, H., Yang, F. et al. Epidemiology and Clinical Profile of Cutaneous Warts in Chinese College Students: A Cross-Sectional and Follow-Up Study. Sci Rep 8, 15450 (2018). https://doi.org/10.1038/s41598-018-33511-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-33511-x
Keywords
This article is cited by
-
Short-term effect of ambient temperature and ambient temperature changes on the risk of warts outpatient visits in Hefei, China: a retrospective time-series study
Environmental Science and Pollution Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.