Abstract
The objective of the present study is to assess the performance of fasting blood glucose (FBG), postprandial blood glucose (PBG), and glycated hemoglobin (HbA1c) as screening for coronary heart disease (CHD) in an inpatient population undergoing coronary angiography. 1852 consecutive patients scheduled for coronary angiography were classified into Normal Glucose Tolerance (NGT), Impaired Glucose Regulation (IGR), and diabetes, based on FBG, PBG, and HbA1c. Correlations of Gensini score with glucose metabolism and insulin resistance were analyzed. The associations between glycemic variables and Gensini score or the presence of CHD were analyzed by multiple linear regression and logistic regression, respectively. CHD was diagnosed in 488, 622, and 414 patients with NGT, IGR, and diabetes, respectively. Gensini score was positively correlated with FBG (r = 0.09, p < 0.01), PBG (r = 0.20, p < 0.01), and HbA1c (r = 0.19, p < 0.01). Gensini score was not correlated with fasting insulin (r = −0.081, p = 0.36), post-prandial insulin (r = −0.02, p = 0.61), or HOMAIR (r = −0.0059, p = 0.13). When FBG, PBG and HbA1c were pooled altogether, only PBG persisted in its association with Gensini score and the prevalence of CHD. The severity of CHD was associated with glucose rather than insulin resistance in this Chinese population. PBG was optimally correlated with the presence and severity of CHD.
Similar content being viewed by others
Introduction
Diabetes has already become a major public health problem in China. According to the recent 2013 national survey, the estimated overall prevalence of diabetes and prediabetes in China was 10.9% and 35.7%, respectively1. Current diagnostic cutoff points for diabetes are based on the correlations of glycated hemoglobin (HbA1c), Fasting Blood Glucose (FBG) and Postprandial Blood Glucose (PBG) with the prevalence of diabetic retinopathy, a hallmark of microvascular disease. Nevertheless, macrovascular disease precedes microvascular disease, and cardiovascular disease (CVD) is the leading cause of mortality in patients with diabetes2. Conversely, the prevalence of IGT and diabetes in patients scheduled for coronary angiography was much higher than the general population3.The association between diabetes and coronary heart disease (CHD) has been well established by numerous studies. Heart disease was listed as the leading cause of death in people with diabetes4. The risk for myocardial infarction in diabetic patients without previous myocardial infarction was reported as high as the risk for nondiabetic patients with previous myocardial infarction5. About 1 in 6 UKPDS (United Kingdom Prospective Diabetes Study) patients with newly diagnosed type 2 diabetes mellitus had evidence of silent myocardial infarction, increasing the risks of fatal myocardial infarction and all-cause mortality6. Significantly increased cardiovascular risk/mortality was also observed even in subjects with IGT7. Hence it is important to screen for CHD in patients with glucose dysregulation.
Despite introduction of new radiological modalities like Computed Tomography Angiography (CTA), coronary angiography remains the current gold standard for diagnosing CHD8. So far, only a few studies have investigated the correlation between glycemic variables and coronary atherosclerotic status evaluated by coronary angiography. Large-scale studies investigating the correlation between glycemic variables and coronary atherosclerotic status by coronary angiography are still lacking.
The aim of the present study was to evaluate the performance of FPG, PBG, and HbA1c as screening for CHD based on a large inpatient population undergoing coronary angiography.
Research Design and Methods
Study population
Our study enrolled a total of 2045 consecutive adults who underwent coronary angiography for suspected CHD in the Cardiology Department of Zhongshan Hospital, Fudan University, a tertiary referral hospital, between March 2013 and November 2013. Patients suspected of CHD in primary and secondary hospitals, based on symptoms like chest pain and dyspnea, were referred to Zhongshan Hospital. In the outpatient department, they were first screened either by routine or dynamic electrocardiogram, coronary computed tomography angiography, exercise treadmill test, or stress myocardial perfusion imaging before coronary angiography assessment. If one of these tests was positive, they were hospitalized and underwent coronary angiography assessment. The exclusion criteria included: acute coronary syndrome, severe systemic diseases, malignancy, and patients with missing data. Finally, 1852 patients were included in the current analysis.
The study was approved by the Ethics Committee of Zhongshan Hospital Fudan University and informed consent was obtained from all participants. All experiments were performed in accordance with relevant guidelines and regulations.
Data collection
Before coronary angiography, all patients underwent a complete history screening, a physical examination, and biochemical evaluation. Family history of CHD in first-degree relatives, current use of medication, and smoking status were recorded. For female patients, menstrual history was also documented. The BMI was calculated as body weight in kilograms divided by body height in meters squared (kg/m2). The WHR (waist-hip ratio) was calculated as the waist circumference at the midpoint between the lower margin of the last palpable rib and the top of the iliac crest, divided by hip circumference at the widest point.
Plasma glucose, lipid profile including serum triglycerides, total cholesterol, HDL cholesterol, LDL cholesterol, ApoA1, ApoB, ApoE and LP(a), glycated albumin, creatinine and uric acid were measured using a biochemical auto analyzer (Hitachi 7600, Japan). Hemoglobin A1c (HbA1c) was determined by HPLC in a National Glycohemoglobin Standardization Program–certified laboratory. Fasting and postprandial serum insulin was measured by an electrochemiluminescence assay (Roche Diagnostics). The index of homeostasis model assessment of insulin resistance (HOMAIR) was calculated as follows: HOMAIR = fasting insulin concentration (mIU/L) × FPG (mmol/L) / 22.5. The index of HOMA β-cell function(HOMAB) was calculated as: HOMAB = 20 × fasting insulin concentration(mIU/L)/[FPG (mmol/L) – 3.5].
Diagnosis and definition
Patients were classified as Normal Glucose Tolerance (NGT), Impaired Glucose Regulation (IGR), or diabetes based on their glycemic variables. NGT was defined in patients without a previous history of diabetes as having a FPG level < 5.6 mmol/L and a PBG level < 7.8 mmol/l. IGR was defined in patients without a previous history of diabetes as meeting at least one of the following:1 FBG ≥ 5.6 mmol/L and < 7.0 mmol/L;2 PBG ≥ 7.8 mmol/L and < 11.1 mmol/L;3 HbA1c 5.7–6.4%. Diabetes was defined either by a previous history and contemporary hypoglycemic medication or according to the 1999 World Health Organization criteria.
Coronary angiography
Selective coronary angiography was performed using standard Judkins techniques or a radial approach. Angiographic findings were analyzed by two experienced cardiologists who were blinded to the study protocol. The diagnosis of CHD was defined as having a stenotic lesion of at least 50% in one or more coronary arteries. The severity of stenosis was quantified by the Gensini score9.
Statistical analysis
All statistical analyses were performed by using SPSS for Windows 13.0 (SPSS Inc, Chicago, IL, USA). Continuous variables were presented as mean ± SD and categorical variables were shown in absolute numbers or percentages. Differences between NGT, IGR, and diabetes groups were assessed by Chi-square test for categorical and ANOVA for continuous variables. Correlation between Gensini score and continuous variables was determined by Pearson correlation coefficients. Stepwise adjustments included: 1) age and gender, 2) smoking status, family history of CHD, history of atrial fibrillation, history of hypertension, BMI, WHR, SBP, and DBP, 3) lipid profile and creatinine. Multiple linear regressions were performed to evaluate the associations between Gensini score and glycemic variables. Confounders adjusted in linear regressions included age, gender, smoking status, family history of CHD, history of atrial fibrillation, history of hypertension, BMI, WHR, SBP, DBP, lipid profile, creatinine, and duration of diabetes. Logistic regressions were also performed to evaluate the associations between the presence of coronary heart disease and glycemic variables. In all analysis, P < 0.05 was considered statistically significant.
Result
General characteristics of the study population
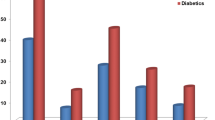
The study population was categorized into three subgroups based on glycemic status. Their characteristics were shown in Table 1. Among the three groups, significant differences were observed in age, BMI, systolic blood pressure, all glycemic variables, insulin levels, lipid profile (triglycerides, HDL-C and APOA1), HOMAIR and finally the presence and severity of CHD.
In the current study population, the prevalence of diabetes and IGR were 25.8% and 40.6%, respectively. Of note, 8.2%(113/1377) of diabetes and 47.9%(659/1377) of IGR were diagnosed for the first time.
No correlation between insulin resistance and Gensini score
In the present studied population, Gensini score was positively correlated with known risk factors such as age, SBP, non-HDL, ApoB, LP(a), and creatinine; but negatively correlated with HDL and ApoA1(r in Table 2). Gensini score was also positively correlated with PBG, postprandial insulin, glycated albumin, and HbA1c. There was no correlation with HOMA index (HOMAIR or HOMAB).
After adjusting for age and gender, FBG also became positively correlated with Gensini score, while postprandial insulin lost its correlation with Gensini score (r1 in Table 2). The positive correlation with four glycemic variables persisted after adjusting smoking status, family history of CHD, history of atrial fibrillation, history of hypertension, BMI, WHR, SBP, DBP (r2 in Table 2), and further adjustments of lipid profile and creatinine (r3 in Table 2). Gensini score was not correlated with insulin (fasting or post-prandial), HOMAIR (representing insulin resistance) or HOMAB (representing β cell function).
Association of FPG, PPG and HbA1c with CHD
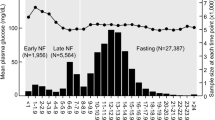
In multiple linear regression analysis, Gensini score was associated with FBG (β = 0.062, p = 0.018), PBG (β = 0.163, p < 0.001), and HbA1c (β = 0.107, p < 0.001). Nevertheless, when pooled altogether, only PBG remained significantly and independently associated with the Gensini score (Table 3). In logistic regression analysis, the presence of CHD was associated with FBG (B = 1.155, p = 0.008), PBG (β = 1.098, p < 0.001), and HbA1c (β = 1.239, p = 0.002). When pooled altogether, the association only remained significant for PBG (β = 1.096, p = 0.000) (Table 4).
Discussion
The prevalence of diabetes was 25.8% in this study, 2.37 fold higher than the 2013 nationwide survey, which estimated the prevalence of diabetes as 10.9%1. In the studied population, the severity of coronary stenosis, quantified as Gensini score, was positively correlated with FBG, PBG, glycated albumin, and HbA1c even after adjustments for all known factors. In contrast, no correlation of Gensini score with fasting insulin, postprandial insulin, HOMAIR or HOMAB remained significant after adjustments for age and gender. Two previous studies in Caucasian men, including 363 men without a diabetes history and 234 men with NGT, observed significant correlations between the number of involved vessels and postload glycemia, HbA1c, fasting insulin, and postload insulin, suggesting that the severity of atherosclerosis was positively correlated with both glucose and insulin resistance10,11. Nevertheless, this was not supported by the findings of the present study. Although hyperinsulinemia or insulin resistance has been regarded as a risk factor for developing cardiovascular disease12,13,14, most East Asian patients with diabetes have much more moderate BMI compared with Caucasians. Impaired insulin secretion was reported to contribute more to the incidence of diabetes than insulin resistance15. Therefore, the significance of insulin resistance in the development of CHD might also be different from that of Caucasians. In fact, our result was in agreement with a previous Korean study of 230 patients, which also concluded that postchallenge hyperglycemia, but not hyperinsulinemia, was associated with CHD assessed by angiography16. The UKPDS study reported that in patients with type 2 diabetes, each 1% reduction in mean HbA1c was associated with a 14% reduction in the risk of myocardial infarction17.
Hyperglycemia itself is an independent risk factor for cardiovascular diseases. Therapies targeting postprandial glucose, including acarbose and insulin, prevent CVD in diabetic patients18,19, whose beneficial effects are independent of improving insulin resistance. It is generally accepted that hyperglycemia leads to atherosclerosis via mechanisms unified as overproduction of ROS and consequent oxidative stress20. Recently more mechanisms have been proposed. Firstly, hyperglycemia can cause epigenetic changes, especially dysregulation of microRNAs. These microRNA changes can lead to dysfunction of endothelial cells, vascular smooth muscle cells, platelets, and macrophage, as well as abnormal lipid metabolism, all of which are involved in atherosclerosis21,22,23. Secondly, the ROS overproduction caused by hyperglycemia triggers redox modifications and malfunction of ion channels in cardiomyocytes, e.g. the type 2 ryanodine receptor (RyR2) on the endoplasmic reticulum (ER). This direct effect may worsen the cardiovascular function observed in chronic hyperglycemia. Thirdly, hyperglycemia alters signaling pathways in atherosclerotic plaques. Plaques from patients with diabetes had more NF-kB expression and less SIRT6 expression, indicating a less stable plaque phenotype24,25,26,27. Collectively, these studies highlighted the contributions of hyperglycemia to the development of cardiovascular injury in diabetes.
The outstanding importance of PBG was supported by both linear and logistic regression analyses. PBG had the most significant correlation with prevalence and severity of CHD amongst the three glycemic parameters. The effects of FBG and HbA1c were completely masked by PBG when they were simultaneously included in the analysis. In logistic regression analysis, PBG stands in line with well-known risk factors like age, gender, and LP(a). Although HbA1c depicted a chronic glycemic profile, glucose fluctuations during postprandial periods triggered oxidative stress more than chronic sustained hyperglycemia. On the contrary, fasting hyperglycemia played a major role as soon as the HbA1c level rises above 8.4%28. Postprandial glucose was more sensitive than HbA1c in screening for prediabetes. 2-h Glucose level and IGT were stronger predictors of CVD than HbA1c29. Kataoka et al.30 reported that diffuse coronary artery narrowing (calculated by averaged vessel diameter and lesion length) was associated with postprandial hyperglycemia in 534 Japanese patients using quantitative coronary angiography. Later in a larger Caucasian cohort of 1040 patients, Saely et al.31 reported that PBG was associated with the number of significant coronary stenoses and the Gensini score. These results were consistent with our findings that PBG was associated with Gensini score, reiterating the importance of PBG in the natural development of coronary artery disease.
Another important finding in the present study was the correlation of PBG with the severity of atherosclerosis (quantified by Gensini score) was independent of the duration of diabetes. This finding may have important clinical implications. The duration of diabetes is known to contribute significantly to CVD risks. A 1.38-fold increased risk for CHD and a 1.86-fold higher risk for CVD death has been reported for each 10-year increase in duration of diabetes by the Framingham Heart Study32. Although the macrovascular complications of diabetes increase with duration, based on our findings, we suggest PBG should be closely monitored for early identification of CHD patients. In other words, aggressive screening of CHD is justified, provided that PBG is elevated, whether diabetes is newly diagnosed or diagnosed long ago.
The strengths of our study resided in the large study population and the use of the “gold standard” coronary angiography for assessing coronary stenosis. However, this study also had some important limitations: 1) As a cross-sectional study, we were unable to establish any causal relationships. 2) Our study focused on a highly selected group of patients, i.e. symptomatic inpatients. We didn’t have an independent population which was more general and less severe to validate the findings. 3) Also, the study involved only Asians, therefore the results may not be generalized to other racial or ethnic groups. 4)The female sample size was relatively small and thus did not allow separate analyses by gender. 5) The superiority of PBG was not validated in another independent population.
In conclusion, the severity of CHD was associated with glucose rather than insulin resistance in a large Chinese inpatient population scheduled for coronary angiography. Postprandial hyperglycemia was independently correlated with the presence and severity of coronary atherosclerosis in this population. These results suggest that the timing of screening should be based on postprandial glucose level, which outperformed FBG, HbA1c and insulin levels. Nevertheless, these findings still need to be validated in another independent population if we want to extend the significance of current study to a more general scenario. Follow-up studies are also needed to investigate the predictive power of postprandial glucose for future cardiovascular events.
References
Wang, L. et al. Prevalence and Ethnic Pattern of Diabetes and Prediabetes in China in 2013. Jama 317, 2515–2523 (2017).
Laakso, M. Hyperglycemia and cardiovascular disease in type 2 diabetes. Diabetes 48, 937–942 (1999).
Taubert, G. et al. Prevalence, predictors, and consequences of unrecognized diabetes mellitus in 3266 patients scheduled for coronary angiography. American heart journal 145, 285–291 (2003).
Gu, K., Cowie, C. C. & Harris, M. I. Mortality in adults with and without diabetes in a national cohort of the U.S. population, 1971-1993. Diabetes care 21, 1138–1145 (1998).
Haffner, S. M., Lehto, S., Ronnemaa, T., Pyorala, K. & Laakso, M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. The New England journal of medicine 339, 229–234 (1998).
Davis, T. M., Coleman, R. L., Holman, R. R. & Group, U. Prognostic significance of silent myocardial infarction in newly diagnosed type 2 diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS) 79. Circulation 127, 980–987 (2013).
t, E. D. E. G. Decode Study Group, Glucose tolerance and cardiovascular mortality: comparison of fasting and 2-hour diagnostic criteria. Archives of internal medicine 161, 397–405 (2001).
Fox, K. et al. Task Force on the Management of Stable Angina Pectoris of the European Society of, E. S. C. C. f. P. Guidelines, Guidelines on the management of stable angina pectoris: executive summary: The Task Force on the Management of Stable Angina Pectoris of the European Society of Cardiology. European heart journal 27, 1341–1381 (2006).
Gensini, G. G. A more meaningful scoring system for determining the severity of coronary heart disease. The American journal of cardiology 51, 606 (1983).
Kowalska, I. et al. Disturbances of glucose metabolism in men referred for coronary arteriography. Postload glycemia as predictor for coronary atherosclerosis. Diabetes care 24, 897–901 (2001).
Sasso, F. C. et al. Glucose metabolism and coronary heart disease in patients with normal glucose tolerance. Jama 291, 1857–1863 (2004).
Despres, J. P. et al. Hyperinsulinemia as an independent risk factor for ischemic heart disease. The New England journal of medicine 334, 952–957 (1996).
Fontbonne, A. et al. Hyperinsulinaemia as a predictor of coronary heart disease mortality in a healthy population: the Paris Prospective Study, 15-year follow-up. Diabetologia 34, 356–361 (1991).
Zavaroni, I. et al. Risk factors for coronary artery disease in healthy persons with hyperinsulinemia and normal glucose tolerance. The New England journal of medicine 320, 702–706 (1989).
Morimoto, A. et al. Impact of impaired insulin secretion and insulin resistance on the incidence of type 2 diabetes mellitus in a Japanese population: the Saku study. Diabetologia 56, 1671–1679 (2013).
Kim, H. K. et al. Postchallenge hyperglycemia but not hyperinsulinemia is associated with angiographically documented coronary atherosclerosis in Korean subjects. Diabetes research and clinical practice 59, 129–136 (2003).
Stratton, I. M. et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. Bmj 321, 405–412 (2000).
Raz, I. et al. Post hoc subgroup analysis of the HEART2D trial demonstrates lower cardiovascular risk in older patients targeting postprandial versus fasting/premeal glycemia. Diabetes care 34, 1511–1513 (2011).
Chiasson, J. L. et al. Acarbose treatment and the risk of cardiovascular disease and hypertension in patients with impaired glucose tolerance: the STOP-NIDDM trial. Jama 290, 486–494 (2003).
Brownlee, M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes 54, 1615–1625 (2005).
Arunachalam, G., Lakshmanan, A. P., Samuel, S. M., Triggle, C. R. & Ding, H. Molecular Interplay between microRNA-34a and Sirtuin1 in Hyperglycemia-Mediated Impaired Angiogenesis in Endothelial Cells: Effects of Metformin. The Journal of pharmacology and experimental therapeutics 356, 314–323 (2016).
Sardu, C. et al. Cardiac Resynchronization Therapy Outcomes in Type 2 Diabetic Patients: Role of MicroRNA Changes. Journal of diabetes research 2016, 7292564 (2016).
Ding, Y., Sun, X. & Shan, P. F. MicroRNAs and Cardiovascular Disease in Diabetes Mellitus. BioMed research international 2017, 4080364 (2017).
Balestrieri, M. L. et al. Sirtuin 6 expression and inflammatory activity in diabetic atherosclerotic plaques: effects of incretin treatment. Diabetes 64, 1395–1406 (2015).
Nakagami, H. et al. Phosphorylation of p38 mitogen-activated protein kinase downstream of bax-caspase-3 pathway leads to cell death induced by high D-glucose in human endothelial cells. Diabetes 50, 1472–1481 (2001).
Baumgartner-Parzer, S. M. et al. High-glucose–triggered apoptosis in cultured endothelial cells. Diabetes 44, 1323–1327 (1995).
Quagliaro, L. et al. Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes 52, 2795–2804 (2003).
Monnier, L., Lapinski, H. & Colette, C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care 26, 881–885 (2003).
Bonora, E. & Tuomilehto, J. The pros and cons of diagnosing diabetes with A1C. Diabetes Care 34(Suppl 2), S184–190 (2011).
Kataoka, Y. et al. Quantitative coronary angiographic studies of patients with angina pectoris and impaired glucose tolerance. Diabetes care 28, 2217–2222 (2005).
Saely, C. H. et al. Key role of postchallenge hyperglycemia for the presence and extent of coronary atherosclerosis: an angiographic study. Atherosclerosis 199, 317–322 (2008).
Fox, C. S., Sullivan, L., D’Agostino, R. B. Sr, Wilson, P. W. & Framingham, S. Heart, The significant effect of diabetes duration on coronary heart disease mortality: the Framingham Heart Study. Diabetes care 27, 704–708 (2004).
Acknowledgements
We thank Dr. Junbo Ge, Dr. Juying Qian, Dr. Daxin Zhou, Dr. Jingmin Zhou and Dr. Yangang Su from Department of Cardiology, Zhongshan hospital, Fudan University, for their cooperation and help in this study. This work was supported by the National Natural Science Foundation of China (81471016).
Author information
Authors and Affiliations
Contributions
Jingjing Jiang and Lin Zhao wrote the main manuscript text. Liu Lin, Minghui Gui and Baishen Pan prepared Tables 1 and 2. Qiqige Aleteng, Bingjie Wu and Shanshan Wang prepared Tables 3 and 4. Yan Ling and Xin Gao designed and coordinated the study. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, J., Zhao, L., Lin, L. et al. Postprandial Blood Glucose Outweighs Fasting Blood Glucose and HbA1c in screening Coronary Heart Disease. Sci Rep 7, 14212 (2017). https://doi.org/10.1038/s41598-017-14152-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-14152-y
This article is cited by
-
Intensified glycemic control by HbA1c for patients with coronary heart disease and Type 2 diabetes: a review of findings and conclusions
Cardiovascular Diabetology (2023)
-
A plant-based meal reduces postprandial oxidative and dicarbonyl stress in men with diabetes or obesity compared with an energy- and macronutrient-matched conventional meal in a randomized crossover study
Nutrition & Metabolism (2021)
-
Impact of free-living pattern of sedentary behaviour on intra-day glucose regulation in type 2 diabetes
European Journal of Applied Physiology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.