Abstract
To quantify the effects of ageing and non-ageing factors, a characterization of the effects of ageing, genetic, and exogenous variables on 12 major non-communicable diseases was evaluated using a model assessing cumulative frequency of death and survival by age group from dead and surviving populations based on mortality statistics. Indices (0–1) of the roles of ageing (ARD), genetics (GRD) and exogenous (ERD) variables in deaths due to disease were established, and the sum of ARD, GRD and ERD was 1 (value of each indices was <1). Results showed that ageing plays an important role in death from chronic disease; exogenous factors may contribute more to the pattern of chronic disease than genetic factors (ARD, GRC and ERD were 0.818, 0.058 and 0.124 respectively for all non-communicable diseases). In descending order, ERD for non-communicable diseases were breast cancer, leukaemia, cancer of the cervix uteri and uterus, liver cancer, nephritis and nephropathy, stomach cancer, lung cancer, diabetes, cerebrovascular disease, coronary heart disease, COPD, and Alzheimer’s disease, while a smaller ERD indicated a tendency of natural death. An understanding of the aforementioned complex relationships of specific non-communicable diseases will be beneficial in designing primary prevention measures for non-communicable diseases in China.
Similar content being viewed by others
Introduction
Modern non-communicable diseases or chronic diseases, such as cardiovascular disease, cancer, and obstructive pulmonary disease, have become the leading causes of death worldwide1,2,3. It is generally accepted that both genetic and environmental factors are related to mechanisms of chronic diseases; here, “genetic factors” are intrinsically hereditary, excluding epigenetic variables; “environmental factors” are all environmental factors including aspects of the social and the natural environment such as stress, lack of physical activity and environmental pollutants. Certain extrinsic risk factors, such as smoking, being overweight, and hyperlipidaemia, may lead to chronic diseases, though they are not necessarily associated with any particular disease4,5,6. Hence, the assessment and control of such risk factors is complicated. Moreover, the incidence of non-communicable diseases tends to increase with age; therefore, a discussion of the aforementioned risk factors shall highlight the association of non-communicable diseases with ageing. Here, “ageing” results in changes in individual capacity to withstand exogenous physical, social and psychological (psychosocial) stressors with increased age. Although the ageing effect could be controlled through manipulation of the exogenous variables that are the causative agents and genetic factors, the role of ageing, genetic and exogenous variables could still be assessed in a certain disease because ageing, genetic and exogenous variables could be stable for a particular population. A better understanding of these associations will be beneficial in developing a theoretical basis for strategies for the prevention and control of non-communicable diseases.
The incidence and progression of non-communicable diseases are affected by various factors, which can be stratified into ageing and non-aging variables. Non-ageing variables include exogenous variables and genetic factors. Age is one of the most important risk factors associated with death due to non-communicable diseases7,8,9. Quantitative analysis of the role of ageing in disease can be used to speculate regarding the effect of non-ageing factors. We propose a role for ageing in death due to disease (ARD) based on the difference in cumulative frequency by age in both dead and surviving groups (cumulative frequency model) to evaluate the effect of ageing and non-ageing factors.
The first step towards understanding a selection of non-communicable diseases is the determination of the non-communicable disease characteristics that may be associated with risk factors. Therefore, it is necessary to quantitatively evaluate the effects of risk factors such as age, genetics and extrinsic variables on non-communicable diseases. In the present study, we used death statistics for all age groups from the census data for Mainland China and established methods for assessing the risk factors for death from non-communicable diseases. Simultaneously, we also selected significant non-communicable diseases on the basis of the quantitative effects of ageing, genetics and extrinsic factors and compared the features of these diseases.
Methods
Original data
The raw data were obtained from the dataset of China’s National Disease Mortality Surveillance System for 2011, which was edited by the Chinese Centre for Disease Control and Prevention and published by the People’s Medical Publishing House10. The data for this particular year were obtained from over 77 million people living in urban and rural areas in the eastern, central and western regions of China and representing approximately 6% of China’s total population. The proportion of people surveyed from urban and rural areas in eastern, central and western regions was similar to that of the whole Chinese population. Further details are provided in Tables 1 and 2. The population count at midnight on July 1, 2011, represented the surviving population.
The underlying causes of death were classified according to the International Classification of Diseases (ICD-10 codes) in order to determine mortality statistics11. The raw data are presented in Table 2.
The role of ageing in deaths caused by chronic disease
The observed population was ranked by age in descending order. If age was not associated with death, the cumulative frequency of survival by age group ought to be consistent with the cumulative frequency of death by age group. The cumulative frequency of survival was plotted on the x-axis, and the cumulative frequency of death in the population by age group was plotted on the y-axis. A scatter plot of the 45-degree diagonal segment was obtained (Fig. 1A). If age had an impact on death, the cumulative frequency of survival was different from that of the population who had died, and the scatter plot curve would be distant from the 45-degree diagonal line (Fig. 1B). The area enclosed by the curve and the 45-degree diagonal line was interpreted as the role of ageing in death (ARD). Age has the greatest impact on death, with a value of 0.5. Therefore, the curve and the 45-degree diagonal area enclosed by the ratio of 0.5 defines the role of age in the quantitative value of death. This is how ARD is represented.
Receiver operating characteristics (ROC) analysis can be used to calculate ARD because there is a relationship between the area under the curve (AUC) from ROC analysis and the area enclosed by the curve and the 45-degree diagonal from the ARD analysis12. The x-axis and y-axis denote the cumulative frequency of survival and the population of those who died by age group, respectively. The AUC can represent the impact of age on death, and ARD can be calculated using the following equation:
The range of ARD was between 0 and 1. A high ARD indicated that disease mortality was mainly due to ageing, and the impact of non-ageing factors was less important.
ROC analysis was performed using SPSS for Windows, version 17.0. The difference in the AUC from 0.5 was considered statistically significant when the probability of a type I error was 0.05 or less.
Role of non-age-related diseases resulting in death
Analysis of the role of non-age-related death (NARD) could include two factors: (1) genetic role in death (GRD) and (2) exogenous role in death (ERD). The basic concept of this analysis is to consider the age of onset as a genetic effect based on existing knowledge13,14,15. For complex diseases such as cancer, age of disease onset is generally thought to be related to a combination of influences related to the duration of exogenous exposures and genetic susceptibility; in effect, subjects with an inherited susceptibility may develop cancer at an earlier age when exposed to the same exogenous exposures16,17,18.
In the present study, the age cut-off at death for different diseases was quantified using ROC analysis, where the ages of people who died from a non-communicable disease were compared to the ages of those who survived over the same period. Mortality should increase markedly when a population exceeds the age cut-off at death for a particular disease; the component below age cut-off at death could be considered GRD, and the component above the age cut-off at death could be considered ERD for this disease.
NARD can be calculated from (1 − ARD). GRD and ERD can be calculated from the following equation:
where Fd represents the cumulative frequency of death in the low age cut-off group.
We used ROC analysis to calculate the ARD for stomach cancer as an example, which is shown in Fig. 2. The cumulative frequency of death (Fd) in the low age cut-off group was 0.145.
Results
The raw data and index of ARD, GRD and ERD for the stipulated non-communicable diseases are summarized in Table 3.
A larger ARD indicated a tendency of natural death from ageing. In descending order, ARD for non-communicable diseases were Alzheimer’s disease, chronic obstructive pulmonary disease, coronary heart disease, cerebrovascular disease, diabetes, lung cancer, stomach cancer, nephritis and nephropathy, liver cancer, cancer of the cervix uteri and uterus, breast cancer, and leukaemia. There were seven non-communicable diseases with an ARD that exceeded all-cause death.
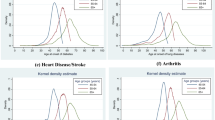
A larger ERD indicated that a disease could be relatively well controlled. In descending order, ERD for non-communicable diseases were breast cancer, leukaemia, cancer of the cervix uteri and uterus, liver cancer, nephritis and nephropathy, stomach cancer, lung cancer, diabetes, cerebrovascular disease, coronary heart disease, chronic obstructive pulmonary disease, and Alzheimer’s disease. There were seven non-communicable diseases with an ERD that exceeded total non-communicable diseases. A smaller ERD also indicated a tendency of natural death, as shown in Fig. 3.
Discussion
Non-communicable diseases are diverse. We mainly selected the non-communicable diseases with the greatest impact on expected survival while simultaneously considering the various types of non-communicable diseases. Tumours are complicated, and different tumours vary significantly in their prognosis and outcomes; therefore, tumours were mainly recorded for the various systems. In this study, 12 non-communicable diseases were included, accounting for 79.46% of the total number of non-communicable diseases. These included the main fatal diseases of the nervous, respiratory, cardiovascular, digestive, endocrine, urogenital, and blood systems.
The cumulative frequency model in this study was based on a comparison between deaths and surviving groups; thus, the influence of the constituent ratio of age in the surviving population should be eliminated. Ageing is a key predictor of mortality for non-communicable disease, and the results show that ageing plays a dominant role in the pattern of chronic disease, suggesting that a model including cumulative frequency of death and survival by age group from dead and surviving populations was reasonable.
It is important to evaluate the effects of ageing on non-communicable disease. We defined non-communicable disease when ARD exceeded all-cause death of ARD as chronic diseases of ageing. Seven diseases (Alzheimer’s disease, chronic obstructive pulmonary disease, coronary heart disease, cerebrovascular disease, diabetes, lung cancer, and stomach cancer) accounted for 89.72% of the non-communicable diseases included in this study. For these particular diseases, ageing appears to be a major precipitant of death, and the role of non-aging variables appears to be limited. Since ageing cannot be influenced, preventative medical care could be a key measure for prolonging survival time with these diseases.
In this study, “exogenous” roles are the causative agents affecting the incidence of non-communicable disease. Non-communicable disease causative agents can be classified as primary (non-medical) factors (such as psychosocial stressors) or secondary causative agents (such as risky behaviours including smoking, diet and obesity, infections, radiation, lack of physical activity, and environmental pollutants)19,20,21. When ERD for a disease exceeded ERD for total non-communicable disease, this disease was defined as exogenous-related chronic disease. Seven diseases (breast cancer, leukaemia, cancer of the cervix uteri and uterus, liver cancer, nephritis and nephropathy, stomach cancer, and lung cancer) accounted for 24.6% of the 12 non-communicable diseases. Since the non-aging factors leading to disease can be influenced to some extent, we suggest that this group of diseases could be prevented by reducing risk factors, including tobacco use, being overweight, a nutritionally inadequate diet, physical inactivity, alcohol consumption, sexually transmitted infections, air pollution and a number of other risk factors that are modifiable. Moreover, a significant aspect of this study is that we included mortality data from women affected by three gynaecological cancers, and these can disproportionately be affected by the exogenous factors associated with such cancers.
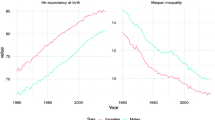
The roles of aging, genetics, and exogenous factors are closely linked to disease status20, 22, 23. Data in this study suggest that ageing plays an important role in chronic disease, indicating that a natural death was the main cause of death from chronic disease. Without considering role of ageing, exogenous factors could play more of a role in the pattern of chronic disease resulting in death than genetic factors. To an extent, this indicates that chronic disease could be both preventable and controllable. With improvements in general health and medical care, the survival time for those with chronic diseases will be extended, which may be the main reason for prolonged life expectancy in more developed societies24.
Notably, the ageing effect, which is counted in the model of chronic disease resulting in death, could also be controlled through manipulation of the exogenous variables that are the causative agents of disease; therefore, the role of exogenous variables in chronic disease using our model may be underestimated. However, we speculate that interaction among aging, genetics, and exogenous factors may be limitation12 and our comprehensive model for chronic disease is still valid because ageing is relatively uncontrollable. Therefore, to improve the general health of the population, we should attempt to delay the biological ageing effect, improve medical care and extend the survival time for those affected by disease, which is the cornerstone of prevention and control of non-communicable diseases. It is clear that an understanding of the aforementioned features of each disease group will be beneficial for the primary prevention of non-communicable diseases.
In summary, 12 diseases were investigated using a cumulative frequency model, and these 12 diseases accounted for 90% of the total number of deaths from non-communicable disease, indicating that individuals with non-communicable diseases tend to die from natural ageing. As exogenous factors are relatively modifiable, it may be more effective to establish prevention and control measures against exogenous-related chronic diseases and may also be more meaningful in improving the level of care while extending the survival of those affected by diseases of ageing beyond their normal life expectancy.
Limitations of this study are that the model for assessing the role of ageing and non-aging factors in death has not been widely used, therefore, the study can only be considered preliminary. China covers a broad geographic area and is undergoing significant regional changes with rapid socioeconomic development. Therefore, earlier data can only be considered as a reference. We propose that the model may provide a better understanding of the characteristics of each non-communicable disease using new systems or concepts. Further studies are warranted to develop a more available model with new data for the identification of novel targets that can be used to create more effective and personalized complex disease prevention strategies.
References
Nakatani, H. Global Strategies for the Prevention and Control of Infectious Diseases and Non-Communicable Diseases. J Epidemiol. 26, 171–178 (2016).
Campbell, D. Economies through Application of Nonmedical Primary-Preventative Health: Lessons from the Healthy Country Healthy People Experience of Australia’s Aboriginal People. Int J Environ Res Public Health. 13, 400 (2016).
Bullen, C. et al. Targets and actions for noncommunicable disease prevention and control in New Zealand. N Z Med J. 128, 55–60 (2015).
Brinks, R., Hoyer, A. & Landwehr, S. Surveillance of the Incidence of Non-Communicable Diseases (NCDs) with Sparse Resources: A Simulation Study Using Data from a National Diabetes Registry, Denmark, 1995–2004. PLoS One. 11, e0152046 (2016).
Ahmadi, B. et al. Multimorbidity: Epidemiology and Risk Factors in the Golestan Cohort Study, Iran: A Cross-Sectional Analysis. Medicine (Baltimore). 95, e2756 (2016).
Hanewinckel, R., van Oijen, M., Ikram, M. A. & van Doorn, P. A. The epidemiology and risk factors of chronic polyneuropathy. Eur J Epidemiol. 31, 5–20 (2016).
Beltrán-Sánchez, H., Soneji, S. & Crimmins, E. M. P. Present, and Future of Healthy Life Expectancy. Cold Spring Harb Perspect Med. 5, a025957 (2015).
King, M. & Lipsky, M. S. Clinical implications of aging. Dis Mon. 61, 467–474 (2015).
Rodríguez Mañas, L. Determinants of Frailty and Longevity: Are They the Same Ones? Nestle Nutr Inst Workshop Ser. 83, 29–39 (2015).
Chinese C for Disease Control and Prevention. National Disease Mortality Surveillance System, 2011. People’s Medical Publishing House 171–405 (2013).
World Health Organization. International Statistical Classification of Diseases and Related Health Problems, Tenth Revision. Geneva, Switzerland: World Health Organization (1992).
Hui, L. Aging and chronic disease as independent causative factors for death and a programmed onset for chronic disease. Arch Gerontol Geriatr. 60, 178–182 (2015).
Strober, M. Relevance of early age-of-onset in genetic studies of bipolar affective disorder. J Am Acad Child Adolesc Psychiatry. 31, 606–610 (1992).
Hui, L., Jing, Y., Rui, M. & Weijian, Y. Novel association analysis between 9 short tandem repeat loci polymorphisms and coronary heart disease based on a cross-validation design. Atherosclerosis. 218, 151–155 (2011).
Hui, L., Jun, T., Jing, Y. & Yu, W. Screening of cerebral infarction-related genetic markers using a Cox regression analysis between onset age and heterozygosity at randomly selected short tandem repeat loci. J Thromb Thrombolysis. 33, 18–21 (2012).
Liang, J. & Church, J. How to manage the patient with early-age-of-onset (<50 years) colorectal cancer? Surg Oncol Clin N Am. 19, 725–731 (2010).
Fengzhi, T., Weijian, Y. & Hui, L. Efficient association analysis between colorectal cancer and allelic polymorphisms of HLA-DQB1 by comparison of age of onset. Oncol Lett. 3, 517–519 (2012).
Hui, L., Liping, G., Jian, Y. & Laisui, Y. A new design without control population for identification of gastric cancer-related allele combinations based on interaction of genes. Gene. 540, 32–36 (2014).
Renehan, A. G. et al. Body mass index at different adult ages, weight change, and colorectal cancer risk in the National Institutes of Health-AARP Cohort. Am J Epidemiol. 176, 1130–1140 (2012).
Xin, G., Shong, L. & Hui, L. Effect of genetic and non-genetic factors, including aging, on waist circumference and BMI, and inter-indicator differences in risk assessment. Exp Gerontol. 60, 83–86 (2014).
Wenping, S., Ying, L., Song, L., Yuzhong, L. & Hui, L. Objective assessment of health or pre-chronic disease state based on a health test index derived from routinely measured clinical laboratory parameters. J Transl Med. 13, 127 (2015).
An, W. X., Fan, Y. X., Liang, X. H. & Liu, H. Changes in median ages at death from selected cancer types in relation to HLA-DRB1/DQB1. Asian Pac J Cancer Prev. 15, 4125–4128 (2014).
Sun, W., Xv, Z., Wang, C. & Liu, H. Evaluation of Aging and Health Status in Real Time Based on Routine Urinalysis Using an Automated Urine Analyzer. Clin Lab. 61, 1883–1887 (2015).
Hui, L. Chronic Diseases and Societal Development, Based on the Death-risk Index. Epidemiology. 26, e9–e10 (2015).
Author information
Authors and Affiliations
Contributions
L.H. conceived of the study, performed the statistical analysis and drafted the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The author declares that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hui, L. Assessment of the role of ageing and non-ageing factors in death from non-communicable diseases based on a cumulative frequency model. Sci Rep 7, 8159 (2017). https://doi.org/10.1038/s41598-017-08539-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-08539-0
This article is cited by
-
A grading system from health to death using routine experimental indicators based on the pre-chronic disease status theory
BMC Geriatrics (2020)
-
Comprehensive analysis of circular RNAs in pathological states: biogenesis, cellular regulation, and therapeutic relevance
Cellular and Molecular Life Sciences (2019)
-
Quantifying the effects of aging and urbanization on major gastrointestinal diseases to guide preventative strategies
BMC Gastroenterology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.