Abstract
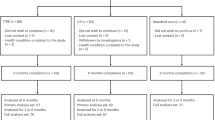
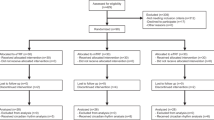
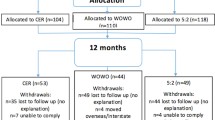
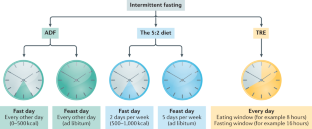
Intermittent fasting diets have become very popular in the past few years, as they can produce clinically significant weight loss. These diets can be defined, in the simplest of terms, as periods of fasting alternating with periods of eating. The most studied forms of intermittent fasting include: alternate day fasting (0–500 kcal per ‘fast day’ alternating with ad libitum intake on ‘feast days’); the 5:2 diet (two fast days and five feast days per week) and time-restricted eating (only eating within a prescribed window of time each day). Despite the recent surge in the popularity of fasting, only a few studies have examined the health benefits of these diets in humans. The goal of this Review is to summarize these preliminary findings and give insights into the effects of intermittent fasting on body weight and risk factors for cardiometabolic diseases in humans. This Review also assesses the safety of these regimens, and offers some practical advice for how to incorporate intermittent fasting diets into everyday life. Recommendations for future research are also presented.
Key points
-
The three main forms of intermittent fasting (alternate day fasting, the 5:2 diet and time-restricted eating) produce mild to moderate weight loss (3–8% loss from baseline) over short durations (8–12 weeks).
-
The degree of weight loss achieved with intermittent fasting is on a par with that achieved with traditional dieting approaches (daily calorie restriction).
-
The ability of these intermittent fasting protocols to help to manage weight long-term is still poorly understood, as the majority of studies to date have run for short durations.
-
Some studies demonstrate that intermittent fasting improves cardiometabolic risk factors such as blood pressure, levels of LDL cholesterol and triglycerides, insulin resistance and HbA1c, while others show no benefit on these parameters.
-
Intermittent fasting is generally safe and produces few gastrointestinal, neurological, hormonal or metabolic adverse effects.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Williamson, D. A., Bray, G. A. & Ryan, D. H. Is 5% weight loss a satisfactory criterion to define clinically significant weight loss? Obesity 23, 2319–2320 (2015).
Brody, J. E. The benefits of intermittent fasting. The New York Times (23 Feb 2020).
Kohik, S. Why is intermittent fasting so popular? BBC News (3 Jun 2019).
de Cabo, R. & Mattson, M. P. Effects of intermittent fasting on health, aging, and disease. N. Engl. J. Med. 381, 2541–2551 (2019).
Brandhorst, S. & Longo, V. D. Dietary restrictions and nutrition in the prevention and treatment of cardiovascular disease. Circ. Res. 124, 952–965 (2019).
Longo, V. D. & Panda, S. Fasting, circadian rhythms, and time-restricted feeding in healthy lifespan. Cell Metab. 23, 1048–1059 (2016).
Mattson, M. P., Longo, V. D. & Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res. Rev. 39, 46–58 (2017).
Paoli, A., Tinsley, G., Bianco, A. & Moro, T. The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients 11, 719 (2019).
St-Onge, M. P. et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation 135, e96–e121 (2017).
Harvie, M. & Howell, A. Potential benefits and harms of intermittent energy restriction and intermittent fasting amongst obese, overweight and normal weight subjects–a narrative review of human and animal evidence. Behav. Sci. 7, 4 (2017).
Patterson, R. E. & Sears, D. D. Metabolic effects of intermittent fasting. Annu. Rev. Nutr. 37, 371–393 (2017).
Tinsley, G. M. & La Bounty, P. M. Effects of intermittent fasting on body composition and clinical health markers in humans. Nutr. Rev. 73, 661–674 (2015).
Stekovic, S. et al. Alternate day fasting improves physiological and molecular markers of aging in healthy, non-obese humans. Cell Metab. 31, 878–881 (2020).
Catenacci, V. A. et al. A randomized pilot study comparing zero-calorie alternate-day fasting to daily caloric restriction in adults with obesity. Obesity 24, 1874–1883 (2016).
Johnson, J. B. et al. Alternate day calorie restriction improves clinical findings and reduces markers of oxidative stress and inflammation in overweight adults with moderate asthma. Free Radic. Biol. Med. 42, 665–674 (2007).
Cho, A. R. et al. Effects of alternate day fasting and exercise on cholesterol metabolism in overweight or obese adults: a pilot randomized controlled trial. Metabolism 93, 52–60 (2019).
Trepanowski, J. F. et al. Effect of alternate-day fasting on weight loss, weight maintenance, and cardioprotection among metabolically healthy obese adults: a randomized clinical trial. JAMA Intern. Med. 177, 930–938 (2017).
Hoddy, K. K. et al. Meal timing during alternate day fasting: impact on body weight and cardiovascular disease risk in obese adults. Obesity 22, 2524–2531 (2014).
Antoni, R., Johnston, K. L., Collins, A. L. & Robertson, M. D. Investigation into the acute effects of total and partial energy restriction on postprandial metabolism among overweight/obese participants. Br. J. Nutr. 115, 951–959 (2016).
Harvie, M. N. et al. The effects of intermittent or continuous energy restriction on weight loss and metabolic disease risk markers: a randomized trial in young overweight women. Int. J. Obes. 35, 714–727 (2011).
Schubel, R. et al. Effects of intermittent and continuous calorie restriction on body weight and metabolism over 50 wk: a randomized controlled trial. Am. J. Clin. Nutr. 108, 933–945 (2018).
Carter, S., Clifton, P. M. & Keogh, J. B. Effect of intermittent compared with continuous energy restricted diet on glycemic control in patients with type 2 diabetes: a randomized noninferiority trial. JAMA Netw. Open 1, e180756 (2018).
Cienfuegos, S. et al. Effects of 4- and 6-h time-restricted feeding on weight and cardiometabolic health: a randomized controlled trial in adults with obesity. Cell Metab. 32, 366–378 (2020).
Tinsley, G. M. et al. Time-restricted feeding in young men performing resistance training: a randomized controlled trial. Eur. J. Sport. Sci. 17, 200–207 (2017).
Tinsley, G. M. et al. Time-restricted feeding plus resistance training in active females: a randomized trial. Am. J. Clin. Nutr. 110, 628–640 (2019).
Chow, L. S. et al. Time-restricted eating effects on body composition and metabolic measures in humans who are overweight: a feasibility study. Obesity 28, 860–869 (2020).
Wilkinson, M. J. et al. Ten-hour time-restricted eating reduces weight, blood pressure, and atherogenic lipids in patients with metabolic syndrome. Cell Metab. 31, 92–104.e5 (2020).
Parvaresh, A. et al. Modified alternate-day fasting vs. calorie restriction in the treatment of patients with metabolic syndrome: a randomized clinical trial. Complement. Ther. Med. 47, 102187 (2019).
Bhutani, S., Klempel, M. C., Kroeger, C. M., Trepanowski, J. F. & Varady, K. A. Alternate day fasting and endurance exercise combine to reduce body weight and favorably alter plasma lipids in obese humans. Obesity 21, 1370–1379 (2013).
Bhutani, S. et al. Effect of exercising while fasting on eating behaviors and food intake. J. Int. Soc. Sports Nutr. 10, 50 (2013).
Varady, K. A. et al. Alternate day fasting for weight loss in normal weight and overweight subjects: a randomized controlled trial. Nutr. J. 12, 146 (2013).
Fitzgerald, K. C. et al. Effect of intermittent vs. daily calorie restriction on changes in weight and patient-reported outcomes in people with multiple sclerosis. Mult. Scler. Relat. Disord. 23, 33–39 (2018).
Harvie, M. et al. The effect of intermittent energy and carbohydrate restriction v. daily energy restriction on weight loss and metabolic disease risk markers in overweight women. Br. J. Nutr. 110, 1534–1547 (2013).
Sundfor, T. M., Svendsen, M. & Tonstad, S. Effect of intermittent versus continuous energy restriction on weight loss, maintenance and cardiometabolic risk: a randomized 1-year trial. Nutr. Metab. Cardiovasc. Dis. 28, 698–706 (2018).
Overland, J. et al. The safety and efficacy of weight loss via intermittent fasting or standard daily energy restriction in adults with type 1 diabetes and overweight or obesity: a pilot study. Obes. Med. 12, 13–17 (2018).
Gabel, K. et al. Effects of 8-hour time restricted feeding on body weight and metabolic disease risk factors in obese adults: a pilot study. Nutr. Healthy Aging 4, 345–353 (2018).
Lin, S. et al. Does the weight loss efficacy of alternate day fasting differ according to sex and menopausal status? Nutr. Metab. Cardiovasc. Dis. 31, 641–649 (2020).
Gabel, K. et al. Differential effects of alternate-day fasting versus daily calorie restriction on insulin resistance. Obesity 27, 1443–1450 (2019).
Cioffi, I. et al. Intermittent versus continuous energy restriction on weight loss and cardiometabolic outcomes: a systematic review and meta-analysis of randomized controlled trials. J. Transl. Med. 16, 371 (2018).
Harris, L., McGarty, A., Hutchison, L., Ells, L. & Hankey, C. Short-term intermittent energy restriction interventions for weight management: a systematic review and meta-analysis. Obes. Rev. 19, 1–13 (2018).
Headland, M., Clifton, P. M., Carter, S. & Keogh, J. B. Weight-loss outcomes: a systematic review and meta-analysis of intermittent energy restriction trials lasting a minimum of 6 months. Nutrients 8, 354 (2016).
Willoughby, D., Hewlings, S. & Kalman, D. Body composition changes in weight loss: strategies and supplementation for maintaining lean body mass, a brief review. Nutrients 10, 1876 (2018).
Heymsfield, S. B., Gonzalez, M. C., Shen, W., Redman, L. & Thomas, D. Weight loss composition is one-fourth fat-free mass: a critical review and critique of this widely cited rule. Obes. Rev. 15, 310–321 (2014).
Pownall, H. J. et al. Changes in body composition over 8 years in a randomized trial of a lifestyle intervention: the look AHEAD study. Obesity 23, 565–572 (2015).
Ravussin, E. et al. A 2-year randomized controlled trial of human caloric restriction: feasibility and effects on predictors of health span and longevity. J. Gerontol. A Biol. Sci. Med. Sci. 70, 1097–1104 (2015).
Moro, T. et al. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism, maximal strength, body composition, inflammation, and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 14, 290 (2016).
Klempel, M. C., Bhutani, S., Fitzgibbon, M., Freels, S. & Varady, K. A. Dietary and physical activity adaptations to alternate day modified fasting: implications for optimal weight loss. Nutr. J. 9, 35 (2010).
Harvey, J., Howell, A., Morris, J. & Harvie, M. Intermittent energy restriction for weight loss: spontaneous reduction of energy intake on unrestricted days. Food Sci. Nutr. 6, 674–680 (2018).
Dansinger, M. L., Gleason, J. A., Griffith, J. L., Selker, H. P. & Schaefer, E. J. Comparison of the Atkins, Ornish, Weight Watchers, and Zone diets for weight loss and heart disease risk reduction: a randomized trial. JAMA 293, 43–53 (2005).
Das, S. K. et al. Long-term effects of 2 energy-restricted diets differing in glycemic load on dietary adherence, body composition, and metabolism in CALERIE: a 1-y randomized controlled trial. Am. J. Clin. Nutr. 85, 1023–1030 (2007).
Jospe, M. R. et al. Intermittent fasting, Paleolithic, or Mediterranean diets in the real world: exploratory secondary analyses of a weight-loss trial that included choice of diet and exercise. Am. J. Clin. Nutr. 111, 503–514 (2020).
Kalam, F. et al. Beverage intake during alternate-day fasting: relationship to energy intake and body weight. Nutr. Health 25, 167–171 (2019).
Sutton, E. F. et al. Early time-restricted feeding improves insulin sensitivity, blood pressure, and oxidative stress even without weight loss in men with prediabetes. Cell Metab. 27, 1212–1221.e3 (2018).
Lowe, D. A. et al. Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: the TREAT randomized clinical trial. JAMA Intern. Med. 180, 1491–1499 (2020).
Andersson, B., Wallin, G., Hedner, T., Ahlberg, A. C. & Andersson, O. K. Acute effects of short-term fasting on blood pressure, circulating noradrenaline and efferent sympathetic nerve activity. Acta Med. Scand. 223, 485–490 (1988).
Johnston, J. G., Speed, J. S., Jin, C. & Pollock, D. M. Loss of endothelin B receptor function impairs sodium excretion in a time- and sex-dependent manner. Am. J. Physiol. Ren. Physiol. 311, F991–F998 (2016).
Rolland, C. & Broom, I. The effects of very-low-calorie diets on HDL: a review. Cholesterol 2011, 306278 (2011).
Kodama, S. et al. Effect of aerobic exercise training on serum levels of high-density lipoprotein cholesterol: a meta-analysis. Arch. Intern. Med. 167, 999–1008 (2007).
Leon, A. S. & Sanchez, O. A. Response of blood lipids to exercise training alone or combined with dietary intervention. Med. Sci. Sports Exerc. 33, S502–S515 (2001).
Browning, J. D., Baxter, J., Satapati, S. & Burgess, S. C. The effect of short-term fasting on liver and skeletal muscle lipid, glucose, and energy metabolism in healthy women and men. J. Lipid Res. 53, 577–586 (2012).
Halberg, N. et al. Effect of intermittent fasting and refeeding on insulin action in healthy men. J. Appl. Physiol. 99, 2128–2136 (2005).
Salgin, B. et al. Effects of prolonged fasting and sustained lipolysis on insulin secretion and insulin sensitivity in normal subjects. Am. J. Physiol. Endocrinol. Metab. 296, E454–E461 (2009).
Freckmann, G. et al. Continuous glucose profiles in healthy subjects under everyday life conditions and after different meals. J. Diabetes Sci. Technol. 1, 695–703 (2007).
Cervantes Gracia, K., Llanas-Cornejo, D. & Husi, H. CVD and oxidative stress. J. Clin. Med. 6, 22 (2017).
Donath, M. Y. & Shoelson, S. E. Type 2 diabetes as an inflammatory disease. Nat. Rev. Immunol. 11, 98–107 (2011).
Maritim, A. C., Sanders, R. A. & Watkins, J. B. 3rd Diabetes, oxidative stress, and antioxidants: a review. J. Biochem. Mol. Toxicol. 17, 24–38 (2003).
Siti, H. N., Kamisah, Y. & Kamsiah, J. The role of oxidative stress, antioxidants and vascular inflammation in cardiovascular disease (a review). Vasc. Pharmacol. 71, 40–56 (2015).
Tsalamandris, S. et al. The role of inflammation in diabetes: current concepts and future perspectives. Eur. Cardiol. 14, 50–59 (2019).
Wellen, K. E. & Hotamisligil, G. S. Inflammation, stress, and diabetes. J. Clin. Invest. 115, 1111–1119 (2005).
Houstis, N., Rosen, E. D. & Lander, E. S. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 440, 944–948 (2006).
Rains, J. L. & Jain, S. K. Oxidative stress, insulin signaling, and diabetes. Free Radic. Biol. Med. 50, 567–575 (2011).
Zaulkffali, A. S. et al. Vitamins D and E stimulate the PI3K-AKT signalling pathway in insulin-resistant SK-N-SH neuronal cells. Nutrients 11, 2525 (2019).
Manning, P. J. et al. Effect of high-dose vitamin E on insulin resistance and associated parameters in overweight subjects. Diabetes Care 27, 2166–2171 (2004).
Gabel, K., Hoddy, K. K. & Varady, K. A. Safety of 8-h time restricted feeding in adults with obesity. Appl. Physiol. Nutr. Metab. 44, 107–109 (2019).
Hoddy, K. K. et al. Safety of alternate day fasting and effect on disordered eating behaviors. Nutr. J. 14, 44 (2015).
Blau, J. N., Kell, C. A. & Sperling, J. M. Water-deprivation headache: a new headache with two variants. Headache 44, 79–83 (2004).
Spigt, M. G. et al. Increasing the daily water intake for the prophylactic treatment of headache: a pilot trial. Eur. J. Neurol. 12, 715–718 (2005).
Akasheh, R. T. et al. Weight loss efficacy of alternate day fasting versus daily calorie restriction in subjects with subclinical hypothyroidism: a secondary analysis. Appl. Physiol. Nutr. Metab. 45, 340–343 (2020).
Heilbronn, L. K., Smith, S. R., Martin, C. K., Anton, S. D. & Ravussin, E. Alternate-day fasting in nonobese subjects: effects on body weight, body composition, and energy metabolism. Am. J. Clin. Nutr. 81, 69–73 (2005).
Jebeile, H. et al. Intermittent energy restriction is a feasible, effective, and acceptable intervention to treat adolescents with obesity. J. Nutr. 149, 1189–1197 (2019).
Lister, N. B. et al. Fast track to health – intermittent energy restriction in adolescents with obesity. A randomised controlled trial study protocol. Obes. Res. Clin. Pract. 14, 80–90 (2020).
Vidmar, A. P., Goran, M. I. & Raymond, J. K. Time-limited eating in pediatric patients with obesity: a case series. J. Food Sci. Nutr. Res. 2, 236–244 (2019).
Culbert, K. M., Racine, S. E. & Klump, K. L. The influence of gender and puberty on the heritability of disordered eating symptoms. Curr. Top. Behav. Neurosci. 6, 177–185 (2011).
Klump, K. L. Puberty as a critical risk period for eating disorders: a review of human and animal studies. Horm. Behav. 64, 399–410 (2013).
Klump, K. L., Culbert, K. M., O’Connor, S., Fowler, N. & Burt, S. A. The significant effects of puberty on the genetic diathesis of binge eating in girls. Int. J. Eat. Disord. 50, 984–989 (2017).
Jebeile, H. et al. Treatment of obesity, with a dietary component, and eating disorder risk in children and adolescents: a systematic review with meta-analysis. Obes. Rev. 20, 1287–1298 (2019).
Antoni, R., Johnston, K. L., Collins, A. L. & Robertson, M. D. Intermittent v. continuous energy restriction: differential effects on postprandial glucose and lipid metabolism following matched weight loss in overweight/obese participants. Br. J. Nutr. 119, 507–516 (2018).
Chaix, A., Manoogian, E. N. C., Melkani, G. C. & Panda, S. Time-restricted eating to prevent and manage chronic metabolic diseases. Annu. Rev. Nutr. 39, 291–315 (2019).
Wegman, M. P. et al. Practicality of intermittent fasting in humans and its effect on oxidative stress and genes related to aging and metabolism. Rejuvenation Res. 18, 162–172 (2015).
Apolzan, J. W., Carnell, N. S., Mattes, R. D. & Campbell, W. W. Inadequate dietary protein increases hunger and desire to eat in younger and older men. J. Nutr. 137, 1478–1482 (2007).
Leidy, H. J., Tang, M., Armstrong, C. L., Martin, C. B. & Campbell, W. W. The effects of consuming frequent, higher protein meals on appetite and satiety during weight loss in overweight/obese men. Obesity 19, 818–824 (2011).
Weigle, D. S. et al. A high-protein diet induces sustained reductions in appetite, ad libitum caloric intake, and body weight despite compensatory changes in diurnal plasma leptin and ghrelin concentrations. Am. J. Clin. Nutr. 82, 41–48 (2005).
Cava, E., Yeat, N. C. & Mittendorfer, B. Preserving healthy muscle during weight loss. Adv. Nutr. 8, 511–519 (2017).
Mettler, S., Mitchell, N. & Tipton, K. D. Increased protein intake reduces lean body mass loss during weight loss in athletes. Med. Sci. Sports Exerc. 42, 326–337 (2010).
Swithers, S. E. Artificial sweeteners produce the counterintuitive effect of inducing metabolic derangements. Trends Endocrinol. Metab. 24, 431–441 (2013).
Hartmann-Boyce, J. et al. Cognitive and behavioural strategies for weight management in overweight adults: results from the Oxford Food and Activity Behaviours (OxFAB) cohort study. PLoS ONE 13, e0202072 (2018).
Kelley, C. P., Sbrocco, G. & Sbrocco, T. Behavioral modification for the management of obesity. Prim. Care 43, 159–175 (2016).
Teixeira, P. J. et al. Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med. 13, 84 (2015).
Ghelani, D. P., Moran, L. J., Johnson, C., Mousa, A. & Naderpoor, N. Mobile apps for weight management: a review of the latest evidence to inform practice. Front. Endocrinol. 11, 412 (2020).
Carter, S., Clifton, P. M. & Keogh, J. B. Intermittent energy restriction in type 2 diabetes: a short discussion of medication management. World J. Diabetes 7, 627–630 (2016).
Grajower, M. M. & Horne, B. D. Clinical management of intermittent fasting in patients with diabetes mellitus. Nutrients 11, 873 (2019).
Varady, K. A., Bhutani, S., Church, E. C. & Klempel, M. C. Short-term modified alternate-day fasting: a novel dietary strategy for weight loss and cardioprotection in obese adults. Am. J. Clin. Nutr. 90, 1138–1143 (2009).
Carlson, O. et al. Impact of reduced meal frequency without caloric restriction on glucose regulation in healthy, normal-weight middle-aged men and women. Metabolism 56, 1729–1734 (2007).
Higgins, J. P. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928 (2011).
Acknowledgements
The authors thank the participants in the trials discussed in this Review for their time and effort. The authors acknowledge support from the National Institute of Diabetes and Digestive and Kidney Diseases (grant no. R01DK119783). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
K.A.V., S.C., M.E. and K.G. contributed to all aspects of the preparation and writing of this Review.
Corresponding author
Ethics declarations
Competing interests
K.A.V. received author fees from Hachette Book Group for the book, The Every Other Day Diet. The other authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Endocrinology thanks M. Harvie, K. Petersen and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Varady, K.A., Cienfuegos, S., Ezpeleta, M. et al. Clinical application of intermittent fasting for weight loss: progress and future directions. Nat Rev Endocrinol 18, 309–321 (2022). https://doi.org/10.1038/s41574-022-00638-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41574-022-00638-x
This article is cited by
-
Network meta-analysis of three different forms of intermittent energy restrictions for overweight or obese adults
International Journal of Obesity (2024)
-
Role of dietary interventions on microvascular health in South-Asian Surinamese people with type 2 diabetes in the Netherlands: A randomized controlled trial
Nutrition & Diabetes (2024)
-
Systemic proteome adaptions to 7-day complete caloric restriction in humans
Nature Metabolism (2024)
-
Early time-restricted carbohydrate consumption vs conventional dieting in type 2 diabetes: a randomised controlled trial
Diabetologia (2024)
-
Intermittent fasting: consider the risks of disordered eating for your patient
Clinical Diabetes and Endocrinology (2023)