Abstract
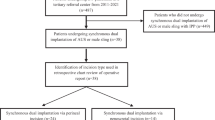
Men with neurogenic bladder (NGB) often have concomitant erectile dysfunction and may be considered for inflatable penile prosthesis (IPP) placement. However, it is unclear if NGB is a risk factor for complications associated with IPP placement. The aim of this study is to compare surgical outcomes after IPP placement in a contemporary cohort of patients with NGB to that of a non-neurogenic control group. To accomplish this, consecutive records of patients who underwent IPP implantation between 2007 and 2018 were retrospectively reviewed. Patients with a known neurologic lesion and documented NGB by clinical or urodynamic criteria were compared with a non-neurogenic control group of men with erectile dysfunction. We found that patients in the NGB cohort were younger (median age 48 vs. 62 years, p < 0.001) and less likely to void spontaneously prior to surgery (3% vs. 97%, p < 0.001). The most common cause for NGB was spinal cord injury (46%). There was a 24.3% overall rate of complication (infection, erosion, or mechanical failure) in the NGB cohort compared with a 7.5% rate in the non-neurogenic control group (p = 0.001). On multivariate logistic regression modeling, NGB (OR 3.47; 95% CI 1.13–10.71; p = 0.03) was independently associated with risk of IPP complication. First time penile prosthesis was associated with lower risk of IPP complication (OR 0.25 95% CI 0.09–0.71; p = 0.01). In conclusion, patients with NGB are at increased risk for complications after IPP placement. Patients should be counseled accordingly, and all efforts should be made to stabilize bladder function prior to surgery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Barton GJ, Carlos EC, Lentz AC. Sexual quality of life and satisfaction with penile prostheses. Sex Med Rev. 2019;7:178–88.
Rodriguez KM, Kohn TP, Davis AB, Hakky TS. Penile implants: a look into the future. Transl Androl Urol. 2017;6 Suppl 5:S860–6.
Li K, Brandes ER, Chang SL, Leow JJ, Chung BI, Wang Y, et al. Trends in penile prosthesis implantation and analysis of predictive factors for removal. World J Urol. 2019;37:639–46.
Trost L, Hellstrom WJ. History, contemporary outcomes, and future of penile prostheses: a review of the literature. Sex Med Rev. 2013;1:150–63.
Montague DK, Angermeier KW, Lakin MM. Penile prosthesis infections. Int J Impot Res. 2001;13:326–8.
Wilson SK, Delk JR 2nd. Inflatable penile implant infection: predisposing factors and treatment suggestions. J Urol. 1995;153(3 Pt 1):659–61.
Pineda M, Burnett AL. Penile prosthesis infections-a review of risk factors, prevention, and treatment. Sex Med Rev. 2016;4:389–98.
Levine LA, Becher EF, Bella AJ, Brant WO, Kohler TS, Martinez-Salamanca JI, et al. Penile prosthesis surgery: current recommendations from the international consultation on sexual medicine. J Sex Med. 2016;13:489–518.
Kimoto Y, Iwatsubo E. Penile prostheses for the management of the neuropathic bladder and sexual dysfunction in spinal cord injury patients: long term follow up. Paraplegia. 1994;32:336–9.
Smith AD, Sazama R, Lange PH. Penile prosthesis: adjunct to treatment in patients with neurogenic bladder. J Urol. 1980;124:363–4.
Zermann DH, Kutzenberger J, Sauerwein D, Schubert J, Loeffler U. Penile prosthetic surgery in neurologically impaired patients: long-term followup. J Urol. 2006;175:1041–4.
Jarow JP. Risk factors for penile prosthetic infection. J Urol. 1996;156:402–4.
Steidle CP, Mulcahy JJ. Erosion of penile prostheses: a complication of urethral catheterization. J Urol. 1989;142:736–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dave, C.N., Khalaf, A., Patel, H.D. et al. Neurogenic bladder is an independent risk factor for complications associated with inflatable penile prosthesis implantation. Int J Impot Res 32, 520–524 (2020). https://doi.org/10.1038/s41443-019-0210-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-019-0210-3
This article is cited by
-
Factors associated with postoperative urinary retention in patients undergoing penile prosthesis implantation
International Journal of Impotence Research (2022)
-
Infection rate of penile prosthesis implants in men with spinal cord injury: a meta-analysis of available evidence
International Journal of Impotence Research (2022)