Abstract
The pharmacological treatment of depression consists of stages of trial and error, with less than 40% of patients achieving remission during first medication trial. However, in a large, randomized-controlled trial (RCT) in the U.S. (“GUIDED”), significant improvements in response and remission rates were observed in patients who received treatment guided by combinatorial pharmacogenomic testing, compared to treatment-as-usual (TAU). Here we present results from the Canadian “GAPP-MDD” RCT. This 52-week, 3-arm, multi-center, participant- and rater-blinded RCT evaluated clinical outcomes among patients with depression whose treatment was guided by combinatorial pharmacogenomic testing compared to TAU. The primary outcome was symptom improvement (change in 17-item Hamilton Depression Rating Scale, HAM-D17) at week 8. Secondary outcomes included response (≥50% decrease in HAM-D17) and remission (HAM-D17 ≤ 7) at week 8. Numerically, patients in the guided-care arm had greater symptom improvement (27.6% versus 22.7%), response (30.3% versus 22.7%), and remission rates (15.7% versus 8.3%) compared to TAU, although these differences were not statistically significant. Given that the GAPP-MDD trial was ultimately underpowered to detect statistically significant differences in patient outcomes, it was assessed in parallel with the larger GUIDED RCT. We observed that relative improvements in response and remission rates were consistent between the GAPP-MDD (33.0% response, 89.0% remission) and GUIDED (31.0% response, 51.0% remission) trials. Together with GUIDED, the results from the GAPP-MDD trial indicate that combinatorial pharmacogenomic testing can be an effective tool to help guide depression treatment in the context of the Canadian healthcare setting (ClinicalTrials.gov NCT02466477).
Similar content being viewed by others
Introduction
The pharmacological treatment of depression consists of stages of trial-and-error prescribing, with less than 40% of patients achieving remission during their first medication trial and declining remission rates with each subsequent trial [1]. To help improve this state of affairs, organizations such as the Clinical Pharmacogenetics Implementation Consortium (CPIC), the Dutch Pharmacogenetics Working Group (KNMP), the United States (U.S.) Food and Drug Administration (FDA), and the International Society of Psychiatric Genetics (ISPG) provide recommendations and guidance on the use of pharmacogenetic information for several common psychotropic medications [2,3,4,5,6]. A growing body of evidence supports the use of pharmacogenomic testing to help guide the pharmacological treatment of depression and improve patients’ likelihood of achieving remission [7,8,9].
Combinatorial pharmacogenomic testing is distinct from other testing approaches, such as single- and multi-gene genetic testing, as it uses a weighted algorithmic assessment of multiple pharmacokinetic and pharmacodynamic genes to predict gene-drug interactions [10, 11]. The clinical utility of a combinatorial pharmacogenomic test has been assessed through both open-label and blinded clinical trials [10, 12,13,14,15]. This includes an evaluation of the clinical utility of combinatorial pharmacogenomic testing to guide the treatment of depression in the largest randomized controlled trial (RCT; N = 1167) of pharmacogenomic testing in psychiatry, performed in the U.S. from 2014 to 2017 [14]. Among patients with major depressive disorder (MDD) who failed at least one previous medication trial, the Genomics Used to Improve DEpression Decisions (GUIDED) trial demonstrated that combinatorial pharmacogenomic testing was associated with significant relative increases in both response (31%) and remission (51%) rates, compared to treatment-as-usual (TAU) [14]. Furthermore, meta-analyses have demonstrated that combinatorial pharmacogenomic testing is associated with a 49% relative increase in remission rates among patients with depression who have failed at least one previous medication trial when compared with patients who receive standard care [9].
The presence of universal healthcare in Canada, compared to the U.S., makes access to healthcare more equitable across socio-economic strata [16]. As the nature and cost of healthcare differs between the U.S. and Canada, several studies have evaluated the economic and clinical benefit of combinatorial pharmacogenomic testing in the Canadian system. The economic utility of combinatorial pharmacogenomic-guided treatment of depression in Canada has been demonstrated through studies of pharmacy claims and cost-effectiveness modeling [17, 18]. These studies report reduced healthcare costs in patients who receive treatment guided by combinatorial pharmacogenomic testing, compared to TAU. In terms of clinical utility, IMPACT (Individualized Medicine: Pharmacogenetics Assessment and Clinical Treatment), a large, single-arm, naturalistic study, demonstrated improvement in depression symptoms, response, and remission rates following combinatorial pharmacogenomic testing among Canadian patients with moderate to severe depression [15]. This single-arm study provides preliminary evidence of the clinical utility of combinatorial pharmacogenomic testing in Canada.
Although the existing evidence supports the effectiveness of combinatorial pharmacogenomic testing in a Canadian population, a direct evaluation in a patient- and rater-blinded RCT has not yet been reported. Here we present results from the Canadian Genomic Applications Partnership Program-Major Depressive Disorder (GAPP-MDD) RCT on the use of combinatorial pharmacogenomic testing to guide depression treatment. The GAPP-MDD trial evaluated clinical outcomes when treatment was guided by a combinatorial pharmacogenomic test (guided-care) compared to TAU among Canadian patients with MDD who had at least one previous failed medication trial.
Materials and methods
Trial design
The GAPP-MDD trial (ClinicalTrials.gov: NCT02466477) was a 52-week, three-arm, multi-center, patient- and rater-blinded, randomized, controlled trial evaluating clinical outcomes among patients whose treatment was guided by combinatorial pharmacogenomic testing compared to TAU. Patients were enrolled at screening between June 2015 and June 2018. Patient assessments were conducted at weeks 0 (baseline), 4, 8, 12, 24, 36, and 52. The analyses presented here focus on outcomes at Week 8. The 17-item Hamilton Depression Rating Scale (HAM-D17) was the primary assessment and was administered by blinded central rater. The self-rated 16-item Quick Inventory of Depression Symptomology (QIDS-SR16), a secondary assessment, was also administered at each visit. Additional description of the trial design has been reported in the Supplementary Materials.
The trial protocol was approved by Advarra research ethics board, Clinical Trials Ontario, Hamilton Integrated Research Ethics Board (HiREB), and IRB Schulman, and was performed in accordance with the principles of the Declaration of Helsinki. All patients provided informed consent after receiving a complete description of the study.
Interventions: combinatorial pharmacogenomic testing
GeneSight® Psychotropic combinatorial pharmacogenomic testing was performed by Assurex Health Ltd. (Toronto, ON) on all patients enrolled in the GAPP-MDD trial, using previously described methods [19]. Standard testing (GEN) included select polymorphisms measured within 8 genes (CYP1A2, CYP2B6, CYP2C9, CYP2C19, CYP2D6, CYP3A4, HTR2A, and SLC6A4; U.S. patent no. 8,401,801 and U.S. patent no. 8,688,385). Seven additional polymorphisms within 6 genes shown to have genetic variation associated with antipsychotic-induced weight gain (MC4R, CNR1, NPY, GCG, HCRTR2, NDUFS1) [20,21,22,23,24,25] were measured for a subset of patients receiving “enhanced GeneSight” (EGEN) testing (U.S. patent no. 10,662,475). Genomic DNA was isolated from buccal samples, and the relevant genomic regions were amplified by polymerase chain reaction (PCR). Specific mutations for CYP2B6 (A785G, G516T) and SLC6A4 were detected by gel electrophoresis of PCR products. Analysis of CNR1, CYP1A2, CYP2C19, CYP2C9, CYP3A4, GCG, HCRTR2, HTR2A, MC4R, NDUFS1, and NPY was completed by using a custom xTAG® assay (Luminex Molecular Diagnostics). Analysis of CYP2D6 was completed using xTAG® kits (Luminex Molecular Diagnostics). The following genetic variants may be detected in the assay: CNR1 rs806378; CYP1A2 −3860G > A, −2467T > delT, −739T > G, −729C > T, −163C > A, 2116 G > A, 2499 A > T, 3497 G > A, 3533 G > A, 5090 C > T, 5347 C > T; CYP2B6 *1, *4, *6, *9; CYP2C19 *1, *2, *3, *4, *6, *8, *17; CYP2C9 *1, *2, *3, *5, *6; CYP2D6 *1, *2, *2 A, *3, *4, *5, *6, *7, *8, *9, *10, *11, *12, *14, *15, *17, *41, gene duplication; CYP3A4 *1, *13, *15 A, *22; GCG rs13429709; HCRTR2 rs3134701, rs4142972; HTR2A −1438G > A; MC4R rs489693; NDUFS1 rs6435326; NPY rs16147; SLC6A4 L, S (Supplementary Table 1).
An algorithm weighed the combined influence of each individual genotype on patient response to each individual medication [10]. Based on this weighted and combined phenotype, 33 Health Canada-approved psychotropic medications (Supplementary Table 2) were categorized based on three levels of gene-drug interaction: “use as directed” (no gene-drug interactions), “use with caution” (moderate gene-drug interactions; i.e., medications may be effective with dose modification), and “use with increased caution and with more frequent monitoring” (severe gene-drug interactions that may significantly impact drug safety and/or efficacy).
Randomization and blinding
Pharmacogenomic testing was performed for all patients between the screening and baseline visits. Patients were randomized 1:1:1 to one of three treatment arms, including two intervention arms and a TAU arm. The first intervention arm included patients for whom providers received the standard combinatorial pharmacogenomic test report to guide treatment (GEN arm). The second intervention arm included patients for whom providers received an enhanced combinatorial pharmacogenomic test report to guide treatment (EGEN arm; report included 6 additional genes shown to have genetic variation associated with antipsychotic-induced weight gain). Patients in the control arm (TAU) also received active treatment for their MDD; however, treatment did not include provision of the combinatorial pharmacogenomic test results and recommendations.
Both the patients and raters were blinded to the study arm. The treating clinician had knowledge of the intervention arm because the combinatorial pharmacogenomic report was available to them for patients in the GEN and EGEN arms to guide their treatment approach. In the TAU arm, patients and clinicians were blinded to the combinatorial pharmacogenomic test results until after completion of their week 36 visit.
Participants
The detailed inclusion and exclusion criteria are described in the Supplementary Methods. Briefly, patients were included in the study if they were ≥18 years old, diagnosed with MDD (according to DSM-IV criteria, QIDS-C16 score ≥11 at screening, and QIDS-SR16 score ≥11 at screening and baseline), and had inadequate response to at least one psychotropic medication included on the combinatorial pharmacogenomic report within the current depressive episode. Patients were excluded if they had significant suicidal risk, severe co-occurring psychiatric or cognitive disorders, and/or unstable or significant medical conditions. Patients were recruited from both psychiatric care and primary care settings.
Outcomes
The following outcomes were pre-specified in the Statistical Analysis Plan, available on clinicaltrials.gov as of April 23, 2019 (NCT02466477). The primary outcome was symptom improvement, defined as the mean percent change in HAM-D17 score from baseline to week 8, compared between the GEN and TAU arms in the per-protocol (PP) cohort. Symptom improvement was also compared between GEN and TAU in the intent-to-treat (ITT) cohort. Additionally, the mean absolute change in HAM-D17 score from baseline to week 8 was compared between GEN and TAU arms in both cohorts.
Symptom improvement from baseline to week 8 and response and remission rates at week 8 were compared between the EGEN and GEN arms. If no statistically significant difference was observed between the EGEN and GEN arms for any of these outcomes, it was pre-specified that the two arms would be combined into the single “guided-care” arm for all of the subsequent analyses.
The following secondary patient outcomes were compared between the study arms at week 8 in both the PP and ITT cohorts: (1) Response at week 8, defined as ≥ 50% decrease in HAM-D17 from baseline, and (2) Remission at week 8, defined as having a score of ≤ 7 for HAM-D17. Symptom improvement, response, and remission, defined using the HAM-D17 scale, were also evaluated at week 24. The proportion of patients taking only congruent medications at baseline and week 4 and 8 follow-up were assessed in the study arms in both the PP and ITT cohorts.
The number needed to treat (NNT) for response and remission was defined as the number of subjects required to receive combinatorial pharmacogenomic testing in order for one more subject in the GEN or EGEN treatment arms to achieve the clinical outcome (i.e., response or remission) above that observed in the TAU group.
Statistical analysis
Analysis cohorts
Patient outcomes were assessed in the following pre-specified cohorts: PP and ITT. As specified in the study protocol, QIDS-C16 was not conducted at baseline and therefore not included as a requirement for either cohort. The ITT cohort included patients who met eligibility criteria, with the exception of the baseline QIDS-SR16 < 11 requirement; patients with a QIDS-SR16 < 11 were included in analyses as randomization occurred before baseline. As the intention of the trial was to assess the clinical utility of the combinatorial pharmacogenomic test in patients with moderate or worse depression, the PP cohort excluded patients who did not meet this criterion. Therefore, the PP cohort included the subset of patients who met eligibility criteria and additionally excluded patients who had baseline scores <14 on the HAM-D17 to exclude patients with mild depression. Patients were also excluded if they had clinically relevant protocol violations, as described in CONSORT Diagrams (Supplementary Figs 1, 2), or if their clinician did not view the electronic combinatorial pharmacogenomic report prior to the baseline visit (GEN and EGEN arms only, for the latter).
The final ITT and PP cohorts included 371 patients, and 276 patients, respectively. Patient recruitment was terminated prior to achieving the target enrollment sample size (N = 570), which was based on effect sizes of an early open-label study of pharmacogenomic testing, as described in the Supplementary Methods. The early termination of this trial was based on analyses of results from the large GUIDED trial, which was similar in design to the GAPP-MDD trial, and had the same primary outcome. Primary results for the GUIDED trial were reported in May 2018, when the GAPP-MDD trial was still actively enrolling. Using the effect size observed in the GUIDED trial, power was reassessed, and the target sample size for the GAPP-MDD study was found to be powered at less than 25% probability to detect a statistically significant difference between arms. To achieve 90% power, approximately N = 4000 patients would be required, which was not feasible for this trial.
Medication congruence with combinatorial pharmacogenomic testing
Medication congruence was based on whether a medication was subject to gene-drug interactions as determined by the combinatorial pharmacogenomic test results for a given patient [11]. Gene-drug interaction refers to genetic variation that is predicted to impact the pharmacokinetics or pharmacodynamics of a medication. Incongruent medications were classified as those that were subject to significant gene-drug interactions for the given patient. Patients were classified as taking congruent medications if none of their prescribed medications were subject to significant gene-drug interactions (i.e., none of their medications were classified in the “use with increased caution and with more frequent monitoring” bin on the pharmacogenomic report).
Data analysis
All analyses were performed according to a pre-specified statistical analysis plan, available on clinicaltrials.gov as of April 23, 2019 (NCT02466477). Patient demographics and clinical characteristics were assessed using descriptive statistics for the PP and ITT cohorts. A 3-sample test for the equality of proportions was used to assess differences between the 3 treatment arms after randomization for categorical measures and one-way ANOVA was used for continuous measures. A 2-sample test for the equality of proportions was used to compare the number of patients who previously failed three or more medications between treatment arms. Analyses were performed for patients who completed the study through week 8. The severity of depression was categorized according to HAM-D17 scores: 0–7, normal; 8–13, mild depression; 14–18, moderate depression; 19–22, severe depression; ≥23, very severe depression.
A Mixed Model for Repeated Measures (MMRM) including treatment group, week, baseline HAM-D17 score, treatment group-by-week interaction, and baseline HAM-D17-by-week interaction was used for both change and percentage change from baseline in HAM-D17. A generalized linear mixed model including treatment group, week, baseline HAM-D17 score, treatment group-by-week interaction, and baseline HAM-D17-by-week interaction was used for response and remission in HAM-D17. A Chi-Square test was used for medication congruence analyses. Two-sided P values ≤ 0.05 were considered statistically significant. Analyses were performed using SAS software (Version 9.4) and JMP 15 (SAS Institute).
Evaluation of GAPP-MDD and GUIDED
As the design of the Canadian GAPP-MDD trial resembled that of the large U.S. GUIDED trial, [14] these studies were assessed in parallel. In order to evaluate the similarities in patient outcomes between the two trials, endpoints from each study (i.e., outcomes at week 8) are presented here in a side-by-side table when similar data were available (Supplementary Table 3). As described previously, part of the rationale for the current study was to evaluate the clinical utility of combinatorial pharmacogenomic testing to guide depression treatment in the context of the Canadian healthcare system. Therefore, including the U.S. GUIDED results provides context to the Canadian GAPP-MDD results.
Meta-analysis
A meta-analysis was performed to compare the findings from the GAPP-MDD trial with those from previous similarly designed RCTs. Clinical outcomes were compared between baseline and week 8 for the GAPP-MDD and GUIDED [14] trials, and week 10 for the Winner et al. trial [12]. Symptom improvement from baseline was measured by the percentage change in HAM-D17 from baseline. Mean percentage of symptom improvement at week 8 or week 10 comparing the combinatorial pharmacogenomic-guided care arm to TAU (treatment as usual) and standard error of the mean from each study were used for the meta-analysis. For response and remission, the odds ratio (OR) comparing the combinatorial pharmacogenomic-guided care arm to TAU at week 8 or week 10 with standard error for each study was used for analyses. The pooled mean effect of symptom improvement and pooled odds ratios of response and remission for the three studies were calculated using a fixed effects model. The fixed effects model was used as the study designs were the same and the studies all estimate the same treatment effect. Heterogeneity in effect sizes across studies were tested using the Q-statistic and its magnitude was measured with the I2 statistic. Meta-analyses were run using the meta package in R version 4.0.2. The NNT for each study was calculated using the following equation: 1/AAR, where AAR (Absolute Attributable Risk) was the absolute value of (CER – EER); CER (Control Event Rate) was the event rate (i.e., number of patients achieving response or remission) in the TAU arm and EER (Experimental Event Rate) was the event rate in the combinatorial pharmacogenomic test-guided arm. The NNT for all studies was calculated using the combined CER and EER across the three studies.
Results
Cohort description
Study enrollment and follow-up for patients in the PP and ITT cohorts are presented in CONSORT diagrams (Supplementary Figs 1, 2). A total of 570 patients were planned for enrollment, with 190 in each of the TAU, GEN, EGEN arms in accordance with the protocol. After early termination of enrollment due to subsequent determination of lack of power, the final ITT cohort consisted of 371 patients who completed the baseline visit (N = 118 TAU, N = 125 GEN, N = 128 EGEN; Supplementary Fig. 1). In the PP cohort, an additional 95 patients were excluded after randomization as they had a baseline HAMD-17 score <14 or had other protocol violations. Therefore, the final per-protocol cohort consisted of 276 patients (N = 93 TAU, N = 90 GEN, N = 93 EGEN; Supplementary Fig. 2).
Although the primary analyses focus on the PP cohort, the results from the ITT analyses are also shown here for reference. The baseline demographic characteristics of the PP cohort are presented in Table 1. The same information for the ITT cohort can be found in Supplementary Table 4. In the PP cohort, the majority of patients were female (64.5%), 18–64 years of age (93.9%; mean age 41 years), and self-reported as “Caucasian” (84.1%). The mean HAM-D17 score was 21.4, with 30.4% of patients classified as having moderate, 27.5% severe, and 42% very severe depression. Generalized anxiety disorder was the most common psychiatric comorbidity (43.1%). The mean number of lifetime previously failed psychiatric medications was 3.6. The rate of three or more failed medications in the TAU arm was 46.7% (42/90) compared to 60% in GEN + EGEN arm (108/180; p = 0.051). A total of 196 patients in the PP cohort had HAM-D17 scores available at the week 8 endpoint (N = 69 TAU, N = 65 GEN, N = 62 EGEN), and 149 patients had HAM-D17 scores available through the blinded week 24 endpoint (N = 55 TAU, N = 48 GEN, N = 46 EGEN).
Clinical outcomes
There was no significant difference in the primary endpoint, percent decrease in HAM-D17 score, between the GEN and TAU arms at week 8 in the PP cohort (GEN 24.4 vs TAU 22.6, p = 0.738), nor was there a difference in the mean absolute decrease in HAM-D17 score between GEN and TAU (GEN 5.2 vs TAU 5.1, p = 0.901; Table 2). Similar results were found in the ITT cohort (Table 2).
When comparing the GEN and EGEN arms at week 8 in the PP cohort, there was no significant difference in HAM-D17 endpoints (symptom improvement, p = 0.244; response, p = 0.332; remission, p = 0.834; Supplementary Table 5). Furthermore, due to the similarity between the combinatorial pharmacogenomic algorithms used in the GEN and EGEN arms, there was no difference at week 8 in medication binning on the pharmacogenomic report according to the two algorithms (i.e., medications categorized as “use as directed”, “use with caution”, or “use with increased caution and with more frequent monitoring”). At week 24, only one patient was taking a medication that changed bins in the GEN and EGEN algorithms, but this did not impact their congruence categorization. Based on the above, and as prespecified in the Statistical Analysis Plan, the GEN and EGEN arms were combined for the remainder of the study and referred to as the guided-care arm.
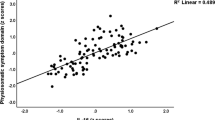
The key outcomes comparing the guided-care and TAU arms at week 8 in the GAPP-MDD study are provided in Fig. 1 and Supplementary Table 3. To help interpret these results and provide additional clinical context, the corresponding data from the prior GUIDED study are also presented. As shown, in the PP cohort of the current GAPP-MDD study, compared to TAU, patients in the guided-care arm had greater HAM-D17-measured symptom improvement (27.6% versus 22.7%; p = 0.274), higher response rate (30.3% versus 22.7%; p = 0.262), and higher remission rate (15.7% versus 8.3%; p = 0.131), although comparisons did not reach statistical significance. Nonetheless, these statistically non-significant values in the GAPP-MDD study are in the direction of improvement, with relative improvements of 22% in symptoms, 33% in response rates, and 89% in remission rates among patients in the guided-arm, compared to TAU. Findings in the ITT cohort at week 8 were similar.
The durability of clinical outcomes was also compared between the guided-care and TAU arms at week 24 (Supplementary Tables 6, 7). In the PP cohort, patients in the guided-care arm experienced an improvement in HAM-D17-measured symptom improvement, response, and remission rates compared to patients in the TAU arm, although no differences reached statistical significance. In the ITT cohort, patients in the guided-care arm continued to experience greater HAM-D17-measured symptom improvement, response, and remission through week 24 compared to patients in the TAU arm, although these improvements did not reach statistical significance.
Decision impact regarding medication congruence
The proportion of patients taking congruent medications at baseline and week 8 was compared between the guided-care and TAU arms in the PP cohort (Fig. 2; Supplementary Table 8). Congruent prescribing increased over the course of the study in the guided-care arm but not in the TAU arm. In the guided-care arm, 83.4% of patients were taking genetically congruent medications at baseline, which increased to 91.1% at week 8. Conversely, in the TAU arm, 81.1% of patients were taking genetically congruent medications at baseline, and 82.1% were taking congruent medications at week 8 (p = 0.070 for the guided-care arm compared to TAU at week 8). Similar results were observed within the ITT cohort (Fig. 2; Supplementary Table 8).
Clinical outcomes in the GAPP-MDD and GUIDED RCTs
As the design of the GAPP-MDD trial resembled that of the U.S. GUIDED trial, clinical outcomes and congruency were presented for the two studies in parallel. The improvement in clinical outcomes observed in the PP cohort of the GAPP-MDD trial was similar to what was observed in the GUIDED trial (Supplementary Table 9). In fact, improvement in HAM-D17-measured symptom improvement, response, and remission at week 8 in the guided-care arm compared to TAU was numerically greater in the GAPP-MDD trial, compared to GUIDED (Fig. 1; Supplementary Table 3). In addition, the increase in medication congruence within the guided-care arms was consistent between studies. Findings within the ITT cohort for GAPP-MDD and GUIDED were also similar (Fig. 1; Supplementary Table 3).
Meta-analysis
The primary end point of the three studies was symptom improvement, measured as percent change from baseline HAMD-17 score to week 8 (for GAPP-MDD and GUIDED trials) or 10 (for Winner et al. 2013). The effect size of symptom improvement was consistent across the three studies (Q = 0.74; p = 0.69; I2 = 0). The fixed effects model suggests that symptom improvement was significantly better when combinatorial pharmacogenomic test results were available to the physician, with HAM-D17 scores decreasing an additional 3.33% (95% CI: 0.17–6.49; p = 0.039) from baseline to week 8 or 10 for guided-care versus TAU (Fig. 3A).
Overall response based on HAM-D17 was also evaluated for the three studies, defined as at least a 50% reduction in HAM-D17 score from baseline to week 8 or 10. The effect size of response was consistent across the three studies (Q = 0.41; p = 0.82; I2 = 0). The pooled odds ratio from the fixed effects model suggests the guided-care arm had a 44% relative improvement in response rate compared with the TAU arm (OR = 1.44, 95% CI: 1.12–1.85; p = 0.004; Fig. 3B). The NNT (i.e., number of patients needed in the GEN and EGEN arms for one more patient to achieve clinical outcomes) for the response was 13.16 for GAPP-MDD, 16.39 for GUIDED, and 6.58 for Pine Rest. The combined NNT for response across the three studies was 14.47.
All three studies also evaluated remission, defined as HAM-D17 ≤ 7 at week 8 or 10. The effect size of remission was consistent across the three studies (Q = 0.524; p = 0.77; I2 = 0). The pooled odds ratio from the fixed effects model suggests that the guided-care arm achieved a 69% relative improvement in remission compared to TAU (OR = 1.69, 95% CI: 1.22–2.34; p = 0.001; Fig. 3C). The NNT for remission was 13.51 for GAPP-MDD, 19.23 for GUIDED, and 8.55 for Pine Rest. The NNT for remission across all three studies combined was 17.62.
Discussion
In both the U.S. and Canada, pharmacotherapy is a first-line treatment option for patients suffering from MDD [26, 27]. However, approved medications can differ across countries, along with healthcare pathways and costs associated with treatment. Therefore, it is important to evaluate the clinical utility of combinatorial pharmacogenomic testing and confirm the U.S. findings in other populations, including Canadian patients with MDD. The GAPP-MDD trial presented clinical outcomes among MDD patients in Canada whose treatment was guided by combinatorial pharmacogenomic testing compared to TAU. Although this trial was underpowered to detect statistically significant differences, numeric improvements in depression symptoms, response rate, and remission rates were observed among patients in the guided-care arm (i.e., who received treatment guided by combinatorial pharmacogenomic testing), compared to TAU. Combinatorial pharmacogenomic-guided treatment also resulted in positive treatment decision impact for prescribing clinicians, where the proportion of patients taking congruent medications increased to over 90% in the guided-care arm, with no change in the TAU arm.
As the intention of the GAPP-MDD trial was to evaluate the utility of the combinatorial pharmacogenomic test in a Canadian population, this trial was assessed in conjunction with a trial conducted in a U.S. population (GUIDED trial). In the GAPP-MDD trial, relative improvements observed in depression symptoms, response, and remission rates in the guided-care arm were consistent with those reported in GUIDED. The GUIDED trial was a larger RCT (N = 1167) and was, therefore, better powered to achieve statistical significance. The results from the GAPP-MDD trial were consistent with significant improvements in response and remissions rates from the GUIDED trial, even though the GAPP-MDD trial, itself, was statistically underpowered. Notably, of the outcomes assessed, we observed the most improvement in remission rates in both studies (51% in GUIDED, statistically significant; 89% in GAPP-MDD, not statistically significant). This is particularly relevant, as remission, the resolution of depression symptoms, is the most challenging endpoint to achieve when treating MDD, and the Canadian Network for Mood and Anxiety Treatments (CANMAT) identifies symptom remission as the primary target of the acute treatment of MDD [28]. The findings from the GAPP-MDD trial, although not statistically significant, are broadly consistent with other studies in the field. Given that trial-and-error is the most common strategy for antidepressant prescribing, even small gains in response can be clinically meaningful. The meta-analysis contributes to the growing body of evidence on the clinical usefulness of combinatorial pharmacogenomics testing [10, 12,13,14,15, 29, 30].
Changes in clinicians’ prescribing of genetically congruent medications in GAPP-MDD paralleled that of the GUIDED trial. Both studies reported a similar increase in clinicians prescribing congruent medications for patients in the guided-care arm, but not TAU arm. This demonstrates consistency in the decision impact of combinatorial pharmacogenomic testing when clinicians have the test available to guide treatment decisions. The high baseline medication congruence in both studies may have resulted from the trial and error involved in selecting an average of 3.6 prior medications per patient; this may have further resulted in more patients on congruent medications. Still, the number of patients in the guided-care arm who were prescribed non-congruent (i.e., genetically discordant) medications decreased by 50% during the study, whereas no decrease occurred in patients in the TAU arm.
A notable difference between the GAPP-MDD and GUIDED RCTs is the ethnicity composition of the patient cohorts. In the PP cohort of both studies, the majority of patients reported “Caucasian” as their ethnicity (GAPP-MDD 84.1%, GUIDED 73.5%). Additionally, the second most common self-reported ethnicity was different between the two studies (“Asian” in the GAPP-MDD cohort, 8.7%; “Black” in the GUIDED cohort, 14.5%). There was also a considerable difference in the proportion of patients who identified as “Latin American” (GAPP-MDD 1.8%, GUIDED 7.9%) between studies. These distributions of patient ethnicities are largely consistent with those observed on a population level within the respective country in which each study was run [31, 32]. Despite differences in self-reported ethnicity between the GAPP-MDD and GUIDED trials, we observed similar improvements in patient outcomes in both cohorts.
One important component of both the GAPP-MDD and GUIDED RCTs is the assessment of outcomes in both the PP and ITT cohorts. In the GAPP-MDD trial, the demographic characteristics of the PP and ITT cohorts were comparable, with the exception that patients with no or mild depression were included in the ITT cohort. Additionally, all patients in the PP cohort had moderate, severe, or very severe depression, whereas 13% of the patients in the ITT cohort had no or mild depression, as determined by baseline HAM-D17 scores of 0–7 and 8–13, respectively. Despite some demographic differences between each of the two cohorts, results were similar, with improved clinical outcomes in the guided-care arm, compared to TAU.
There were several limitations to the current study. The statistical power and design of the GAPP-MDD was determined using effect size estimates for symptom improvement (mean percent change in HAM-D17 score from baseline to week 8) from an earlier open-label clinical trial of combinatorial pharmacogenomic testing [13]. However, as the GAPP-MDD trial was in progress, it became apparent upon release of data from the much larger GUIDED RCT, that the current trial was underpowered based on the GUIDED RCT effect size for symptom improvement. However, we include the GUIDED trial results in this report to provide additional clinical context and relevance. Additional limitations of the GAPP-MDD trial include the following: the majority of the cohort were “Caucasian” (as determined by self-report); lack of assessment of adherence; the impact of polypharmacy on outcomes was not evaluated; and the sample size in the PP and the ITT populations differed due to exclusion of patients with no or mild depression from the PP analyses (although results were similar in both cohorts). In addition, positive expectations are known to influence treatment response. Since the clinicians were not blinded to study arm, positive expectations might have subtle influence on the observations made in this study. A potential strength of the GAPP-MDD study is that this patient population received care under the universal Canadian healthcare system; therefore, socioeconomic biases related to accessibility and affordability of care may have been reduced (although this may have varied by specific study site).
In summary, we observed similar improvement in clinical outcomes following combinatorial pharmacogenomic testing in a Canadian population of patients with MDD who failed to respond to at least one previous medication trial as was seen in the large U.S. GUIDED trial. The similar effect sizes in response and remission between the two studies indicate that the differences observed in the GAPP-MDD trial may represent true differences between arms that did not reach statistical significance due to cohort size. Therefore, results from the GAPP-MDD trial, conducted in the context of the Canadian universal healthcare setting, together with evidence from the GUIDED trial, indicate that combinatorial pharmacogenomic testing is an additional tool available to clinicians that provides clinically useful information to help guide the treatment of depression.
Change history
30 May 2022
A Correction to this paper has been published: https://doi.org/10.1038/s41398-022-01963-5
References
Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–17.
Hicks JK, Bishop JR, Sangkuhl K, Muller DJ, Ji Y, Leckband SG, et al. Clinical pharmacogenetics implementation consortium (CPIC) guideline for CYP2D6 and CYP2C19 genotypes and dosing of selective serotonin reuptake inhibitors. Clin Pharmacol Therapeutics. 2015;98:127–34.
Hicks JK, Sangkuhl K, Swen JJ, Ellingrod VL, Muller DJ, Shimoda K, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharm Ther. 2017;102:37–44.
KNNMP. Pharmacogenetics. 2021; https://www.knmp.nl/patientenzorg/medicatiebewaking/farmacogenetica/pharmacogenetics-1.
U.S. Food & Drug Administration. Table of Pharmacogenomic Biomarkers in Drug Labeling. 2020; https://www.fda.gov/drugs/science-and-research-drugs/table-pharmacogenomic-biomarkers-drug-labeling.
Bousman CA, Bengesser SA, Aitchison KJ, Amare AT, Aschauer H, Baune BT, et al. Review and consensus on pharmacogenomic testing in psychiatry. Pharmacopsychiatry. 2021;54:5–17.
Bousman CA, Arandjelovic K, Mancuso SG, Eyre HA, Dunlop BW. Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 2019;20:37–47.
Rosenblat JD, Lee Y, McIntyre RS. The effect of pharmacogenomic testing on response and remission rates in the acute treatment of major depressive disorder: A meta-analysis. J Affect Disord. 2018;241:484–91.
Brown L, Vranjkovic O, Li J, Yu K, Al Habbab T, Johnson H, et al. The clinical utility of combinatorial pharmacogenomic testing for patients with depression: a meta-analysis. Pharmacogenomics. 2020;21:559–69.
Hall-Flavin DK, Winner JG, Allen JD, Jordan JJ, Nesheim RS, Snyder KA, et al. Using a pharmacogenomic algorithm to guide the treatment of depression. Transl Psychiatry. 2012;2:e172.
Altar CA, Carhart JM, Allen JD, Hall-Flavin DK, Dechairo BM, Winner JG. Clinical validity: Combinatorial pharmacogenomics predicts antidepressant responses and healthcare utilizations better than single gene phenotypes. Pharmacogenomics J. 2015;15:443–51.
Winner JG, Carhart JM, Altar CA, Allen JD, Dechairo BM. A prospective, randomized, double-blind study assessing the clinical impact of integrated pharmacogenomic testing for major depressive disorder. Disco Med. 2013;16:219–27.
Hall-Flavin DK, Winner JG, Allen JD, Carhart JM, Proctor B, Snyder KA, et al. Utility of integrated pharmacogenomic testing to support the treatment of major depressive disorder in a psychiatric outpatient setting. Pharmacogenetics Genomics. 2013;23:535–48.
Greden JF, Parikh SV, Rothschild AJ, Thase ME, Dunlop BW, DeBattista C, et al. Impact of pharmacogenomics on clinical outcomes in major depressive disorder in the GUIDED trial: A large, patient- and rater-blinded, randomized, controlled study. J Psychiatr Res. 2019;111:59–67.
Tanner JA, Davies PE, Voudouris NC, Shahmirian A, Herbert D, Braganza N, et al. Combinatorial pharmacogenomics and improved patient outcomes in depression: Treatment by primary care physicians or psychiatrists. J Psychiatr Res. 2018;104:157–62.
Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health. 2006;96:1300–7.
Tanner JA, Brown LC, Yu K, Li J, Dechairo BM. Canadian medication cost savings associated with combinatorial pharmacogenomic guidance for psychiatric medications. Clinicoecon Outcomes Res. 2019;11:779–87.
Tanner JA, Davies PE, Overall CC, Grima D, Nam J, Dechairo BM. Cost-effectiveness of combinatorial pharmacogenomic testing for depression from the Canadian public payer perspective. Pharmacogenomics. 2020;21:521–31.
Jablonski M, King N, Wang Y, Winner JG, Watterson LR, Gunselman S, et al. Analytical validation of a psychiatric pharmacogenomic test. Personalized Medicine. 2018;15:189–197.
Malhotra AK, Correll CU, Chowdhury NI, Müller DJ, Gregersen PK, Lee AT, et al. Association between common variants near the melanocortin 4 receptor gene and severe antipsychotic drug–induced weight gain. Arch Gen Psychiatry. 2012;69:904–12.
Tiwari A, Zai C, Likhodi O, Lisker A, Singh D, Souza R, et al. Association of a common polymorphism in the Cannabinoid receptor 1 (CNR1) gene with antipsychotic-induced weight gain in chronic schizophrenia subjects. Neuropsychopharmacol: Off Publ Am Coll Neuropsychopharmacol. 2010;35:1315–24.
Tiwari AK, Brandl EJ, Weber C, Likhodi O, Zai CC, Hahn MK, et al. Association of a functional polymorphism in neuropeptide Y with antipsychotic-induced weight gain in schizophrenia patients. J Clin Psychopharmacol. 2013;33:11–17.
Brandl EJ, Tiwari AK, Chowdhury NI, Zai CC, Lieberman JA, Meltzer HY, et al. Genetic variation in the GCG and in the GLP1R genes and antipsychotic-induced weight gain. Pharmacogenomics. 2014;15:423–31.
Tiwari AK, Brandl EJ, Zai CC, Goncalves VF, Chowdhury NI, Freeman N, et al. Association of orexin receptor polymorphisms with antipsychotic-induced weight gain. World J Biol Psychiatry. 2016;17:221–9.
Gonçalves VF, Zai CC, Tiwari AK, Brandl EJ, Derkach A, Meltzer HY, et al. A hypothesis-driven association study of 28 nuclear-encoded mitochondrial genes with antipsychotic-induced weight gain in schizophrenia. Neuropsychopharmacol: Off Publ Am Coll Neuropsychopharmacol. 2014;39:1347–54.
Kennedy SH, Lam RW, McIntyre RS, Tourjman SV, Bhat V, Blier P, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: Section 3. pharmacological treatments. Can J Psychiatry Rev Canadienne de Psychiatr. 2016;61:540–60.
American Psychiatric Association. Practice Guidelines. 2020; https://psychiatryonline.org/guidelines.
Lam RW, McIntosh D, Wang J, Enns MW, Kolivakis T, Michalak EE, et al. Canadian network for mood and anxiety treatments (CANMAT) 2016 clinical guidelines for the management of adults with major depressive disorder: Section 1. Disease burden and principles of care. Can J Psychiatry Rev Canadienne de Psychiatr. 2016;61:510–23.
Dunlop BW, Parikh SV, Rothschild AJ, Thase ME, DeBattista C, Conway CR, et al. Comparing sensitivity to change using the 6-item versus the 17-item Hamilton depression rating scale in the GUIDED randomized controlled trial. BMC Psychiatry. 2019;19:420.
Thase ME, Parikh SV, Rothschild AJ, Dunlop BW, DeBattista C, Conway CR, et al. Impact of pharmacogenomics on clinical outcomes for patients taking medications with gene-drug interactions in a randomized, controlled trial. J Clin Psychiatry. 2019;80:19m12910.
U.S. Department of Commerce. United States Census Beurau: Quick Facts 2019; https://www.census.gov/quickfacts/fact/table/US/PST045219.
Statistics Canada. Data Tables, 2016 Census 2019; https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/dt-td/Rp-eng.cfm?TABID=2&Lang=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=1341679&GK=0&GRP=1&PID=110528&PRID=10&PTYPE=109445&S=0&SHOWALL=0&SUB=0&Temporal=2017&THEME=120&VID=0&VNAMEE=&VNAMEF=&D1=0&D2=0&D3=0&D4=0&D5=0&D6=0.
Acknowledgements
We would like to thank Dr. Azhar Toma and the other investigators and study personnel who contributed to this work. We would also like to thank all study participants as well as Rachel Daut, PhD, Anna Gardiner, PhD, Krystal Brown, PhD, and Brenda Rubalcaba for their assistance with manuscript preparation. The study was initiated as part of the MaRS EXCITE program.
Funding
Funding was provided by Assurex Health, Ltd., Ontario Genomics and Genome Canada. In-kind testing was performed by Assurex Health, Ltd. and in-kind contributions were provided by CAMH.
Author information
Authors and Affiliations
Contributions
AKT: Conceptualization; Formal Analysis; Methodology; Project Administration; Supervision; Writing – Original Draft; Writing – Review & Editing. CCZ:Conceptualization Formal Analysis; Methodology; Project Administration; Supervision; Writing – Original Draft; Writing – Review & Editing. CAA: Conceptualization; Funding acquisition; Investigation; Methodology; Project administration; Supervision; Writing – Original Draft; Writing – Review & Editing. JAT: Visualization; Writing – Original Draft; Writing – Review & Editing. PED: Data curation; Formal analysis; Methodology; Visualization; Software; Validation; Writing – Original Draft PT: Methodology; Software; Validation; Formal Analysis; Data Curation; Visualization. JL: Formal Analysis; Visualization. ESC: Writing – Original Draft; Writing – Review & Editing; MTK: Formal analysis; Writing – Review & Editing. AG: Data curation; Project Administration; Resources. NB: Project administration. HE: Investigation. GZ: Conceptualization; Methodology; Investigation; Supervision; Writing – Review & Editing. DJM: Investigation; Writing – Original Draft; Writing – Review & Editing. RL: Project Administration; Supervision; Writing – Review & Editing. SK: Investigation; Resources; Writing – Review & Editing. ZJD: Investigation. BNF: Investigation; Resources; Supervision; Writing – Review & Editing. JMB: Conceptualization; Funding acquisition; Methodology; Investigation; Project administration; Writing – Review & Editing. JET: Conceptualization; Funding acquisition; Methodology; Investigation; Project administration; Supervision; Writing – Review & Editing. RT: Investigation. RC: Investigation. NV: Conceptualization; Writing – Review & Editing. VHT: Investigation; Writing – Review & Editing. RT: Investigation; Writing – Review & Editing. VS: Investigation; Resources; Writing – Review & Editing. AV: Writing – Reviewing & Editing. PD: Investigation. LP: Investigation. TG: Investigation; Data curation. BMD: Conceptualization, Formal Analysis, Methodology, Supervision, Writing – Review & Editing. JLK: Conceptualization; Funding acquisition; Formal Analysis; Methodology; Project Administration; Resources; Supervision; Writing – Original Draft; Writing – Review & Editing.
Corresponding author
Ethics declarations
Competing interests
AKT is a co-inventor on a patent for antipsychotic-induced weight gain at the time of this study (U.S. patent no. 10,662,475). CCZ had a patent on antipsychotic-induced weight gain markers at the time of this study. CAA had ownership/partnership in Splice Therapeutics at the time of this study, and also serves on the advisory board for AxoSim Inc. and the board of directors for ASENT. JAT, PED, PT, JL, MTK, and AG were employed by Myriad Neuroscience/Assurex Health at the time of this study. MTK and ESC were employed by Myriad Genetics at the time of this study. DJM was a co-inventor on two patents assessing risk for antipsychotic-induced weight gain at the time of this study and was also a co-investigator on two pharmacogenetic studies where genetic test kits were provided as in-kind contribution by Myriad Neuroscience but did not receive any salary, equity, stocks, or options from any pharmacogenetic companies. SK received research support from the University of Toronto, Department of Psychiatry Academic Scholar Award, the Labatt Family Innovation Fund in Brain Health, and the Canadian Institutes of Health Research (CIHR) at the time of this study, and received honorarium from Empowerpharm for past consultation. JMB and JET received funding and payment from Myriad Neuroscience to conduct the GAPP-MDD trial until the contract was terminated by Myriad Neuroscience. BMD was employed by Myriad Genetics at the time of this study and received salary and stock options. JLK is an unpaid member of the Myriad Neuroscience Scientific Advisory Board. All other authors declare no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tiwari, A.K., Zai, C.C., Altar, C.A. et al. Clinical utility of combinatorial pharmacogenomic testing in depression: A Canadian patient- and rater-blinded, randomized, controlled trial. Transl Psychiatry 12, 101 (2022). https://doi.org/10.1038/s41398-022-01847-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-01847-8